In Australia and other developed countries, the provision of after-hours primary care services is a challenging policy area. Limited access to after-hours services, geographical inequities in provision of services, burden on hospital emergency departments and workload for general practitioners (GPs) have prompted governments to implement after-hours primary care reforms. One such initiative is telephone-based assessment, advice and referral.1,2
The first nurse-led telephone triage service in Australia, ‘Healthdirect’, commenced in Western Australia in 1999.3 Since that time, nurse telephone triage and advice has been extended throughout Australia. As part of national primary care reforms, an after-hours GP helpline was established in Australia in July 2011. The helpline was an addition to the existing 24-hour nurse triage and advice lines operating in Australian states and territories. Nurses use clinical software to triage the patient in relation to service need and time frame for attention. Callers to the nurse lines in the after-hours period, or those calling the ‘after hours GP helpline’ (AGPH) number directly, speak first to a nurse who triages the patient’s health issue. In the study period, callers were transferred to a GP on the line if the patient was triaged as needing to see a GP immediately, within four hours or within 24 hours. Nurses handled calls that were triaged as needing emergency care, or care beyond 24 hours and home-based or self-care. The after-hours period is defined as before 8.00 am and after 6.00 pm on weekdays, before 8.00 am and after 12.00 pm on Saturdays, and all day Sundays and public holidays.4
In common with telephone triage and advice services (TTAS) in other countries, such as the UK, Denmark, the Netherlands,1,5 the US,6 Canada7 and New Zealand,8 the AGPH was intended to help manage after-hours demand for urgent care and improve access to GP assessment and advice for those in need, regardless of their location.9 The AGPH is funded by the Australian Government, commissioned by Healthdirect Australia, a company established by the Council of Australian Governments (COAG) in 2006,10 and is operated by a third-party service provider. Limited marketing of the service was undertaken in the establishment phase through Medicare Locals, hospital emergency departments, GP clinics, pharmacies and aged care facilities. During the study period, Healthdirect Australia published quarterly reports on the 20 most common presenting conditions to the AGPH. These presenting conditions were fairly stable, with minor variation across the period. Table 1 presents an example of the top 20 presenting conditions from one quarterly report.
Table 1. Twenty most common clinical presentations to AGPH April–June 2012
|
| 1. Respiratory symptoms (P) |
| 2. Vomiting |
| 3. Rash |
| 4. Cough (P) |
| 5. Headache |
| 6. Vomiting (P) |
| 7. Diarrhoea |
| 8. Gastrointestinal bleeding |
| 9. Chest pain |
| 10. Cold (P) |
| 11. Postoperative problems |
| 12. Asthma (P) |
| 13. Sore throat |
| 14. Bloody urine |
| 15. Cough |
| 16. Dizziness/vertigo |
| 17. Urinary symptoms: female |
| 18. Constipation (P) |
| 19. Flank pain |
| 20. Diarrhoea (P) |
|
P, paediatric
Reproduced with permission from National Health Call Centre Network from the Quarterly Report April–June 2012. Available at www.healthdirect.gov.au/corporate-publications [Accessed 6 October 2015].
|
An evaluation of the first two years of operation of the AGPH, 2011–13 (Centre for Health Policy, 2013, unpublished), examined many aspects of the service, including use, quality and clinical appropriateness, consumer satisfaction, clinical service provider experiences and service costs. This study presents information on the use of the service, describing the age, gender, location and socioeconomic advantage profile of users of the AGPH during the establishment phase of the service. The study is the starting point in ongoing profiling of TTAS use in Australia. The study is modelled on similar investigations, over time, of the characteristics of users of NHS Direct (an English TTAS that operated for almost two decades before recent replacement with NHS 911). The service was comparable to Australian telephone-based primary care advice services. Age, gender, ethnic background and socioeconomic deprivation of NHS Direct users have been extensively studied11–17 and provide a comparative point of reference for our findings. This study adds an Australian component to what is known internationally about the characteristics of users of patient-initiated telephone-based health advice services.
Methods
De-identified data routinely collected by the service provider and reported quarterly to the service commissioner were made available to the researchers. The age, gender and postcode of callers and patients (the user with the health condition, who may not be the caller), and the total number of calls for the eight quarters from July 2011 to June 2013, were examined. The data were descriptively analysed for frequencies using Microsoft Excel. During the first two years of operation, postcodes were coded by the service commissioner according to the Rural, Remote, Metropolitan Areas (RRMA) population classification system.18 The geographic profile of callers was analysed in relation to the recorded RRMA classification.
Investigation of the relative socioeconomic advantage or disadvantage of the postcode areas of users was undertaken using the Australian Bureau of Statistics’s (ABS’s) Socio-Economic Indexes for Areas, Index of Relative Socio-economic Advantage and Disadvantage (SEIFA IRSAD). SEIFA IRSAD rankings reflect the socioeconomic wellbeing of an area, rather than the individuals within it.19 All postcodes and their corresponding RRMA classification were joined to a SEIFA IRSAD decile, with 10 being the most advantaged and 1 being the most disadvantaged. Population-adjusted use of the AGPH by postcode and SEIFA IRSAD classification were spatially mapped and analysed using ESRI ArcGIS 10.2.2. This study was deemed as not requiring ethical approval given its reliance on de-identified secondary data.
Results
Service use 2011–13
The AGPH handled 334,654 calls in its first two years of operation, averaging 3218 calls per week and 144.67 calls per 10,000 head of population.20 The service exceeded its call target of 150,000 calls per year. Calls triaged to the AGPH represented 20% of the 1.6 million calls handled by the ‘Healthdirect’ nurse triage line in the study period.
Gender and age of patients
Patients who used the AGPH were more likely to be female (approximately 61% female and 39% male). As shown in Figure 1, the gender split was fairly even for child patients aged up to 14 years, but thereafter more female patients were found in each age group. There were markedly higher numbers of female patients in the 15–44 years age range. The single largest patient age group was 0–4 years, representing more than one-quarter (27%) of presentations to the AGPH, with more than one-third of patients (34%) aged under 10 years. Almost three-quarters (72%) of patients were aged under 40 years. Five per cent of patients were aged 40–44 years, and the age groups 45–49, 50–54, 55–60 and 60–64 each represented approximately 3% of calls. Patients from 65 years onwards represented 8.5% of calls.
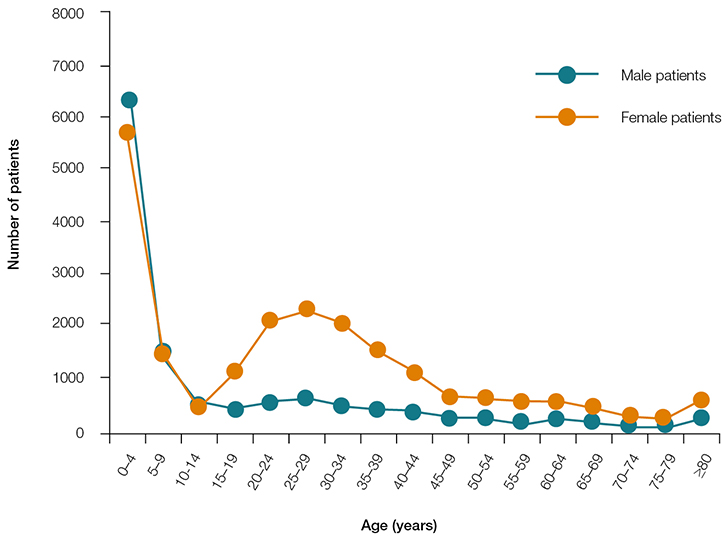 |
| Figure 1. Age and gender of AGPH patients July 2011 – June 2013 |
Relationship of caller to patient
Calls to the service by patients themselves were the most common call category (52%). Parents of patients (38%) were the next most common call category, followed by partners of patients (4%) and children of patients (2%).
Ethnic and cultural background
Callers who identified as Aboriginal or Torres Strait Islander (in response to a question from the triage nurse) represented 3.5% of all calls. Ethnic background or language most commonly spoken at home were not recorded; therefore, the ethnic background of callers is unknown. However, fewer than 100 callers used an interpreter service to access the AGPH.
Geographic location of users
The majority of calls came from New South Wales (NSW), representing almost 40% of all calls. Western Australians were the next most frequent users of the service, representing 22% of all calls. It should be noted that Western Australia and NSW have had established ‘Healthdirect’ nurse lines since 1999 and 2007 respectively. Victorians accounted for 16% of service users, noting that Victoria did not join the AGPH until late April 2012. Queenslanders were low users of the service, noting that this state did not join the AGPH until March 2012. Only 630 callers were from Tasmania. Figure 2 presents the distribution of callers by state.
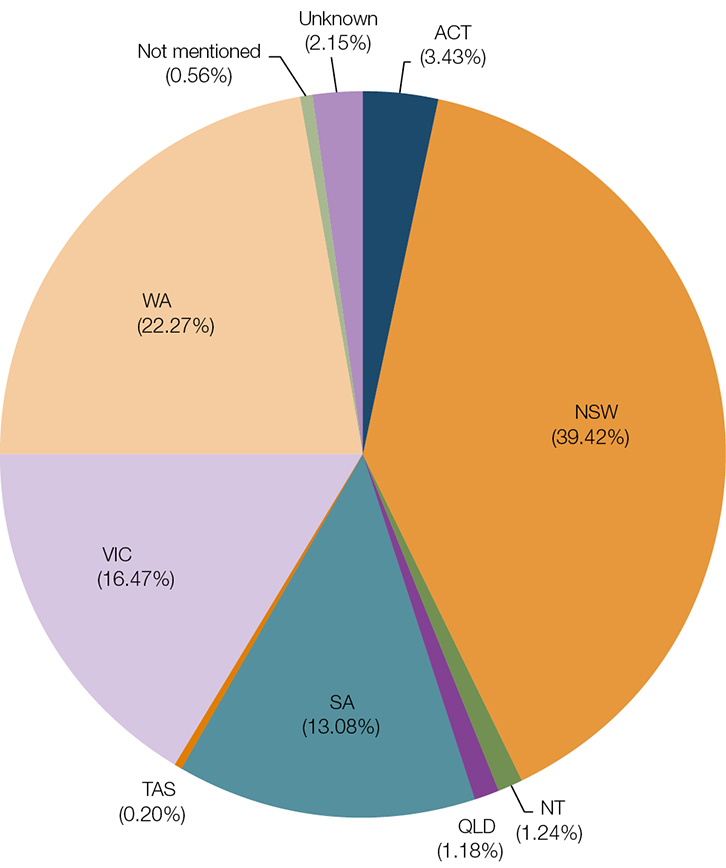 |
Figure 2. State and territory origin of calls to the AGPH July 2011 to June 2013 (n = 334,654)
Callers by state or territory to the 'after hours GP helpline' (AGPH) July 2011 − June 2013 |
Almost three-quarters of callers lived in a capital city (72%), and a further 6% lived in other metropolitan areas. Twenty per cent had a rural area postcode (the sum of large, small or other rural area postcodes), and almost 2% identified as living in a remote area. On a population-adjusted basis, the highest usage was in capital cities (an average of 183.8 calls per 10,000 population) followed by remote areas (an average of 161 calls per 10,000 population) and remote centres (an average of 148.4 calls per 10,000 population). The lowest average call rate of 97.7 calls per 10,000 of population was found in large rural centres.
Socioeconomic advantage/disadvantage of caller’s area of residence
On a population-adjusted basis averaged across all RRMA SEIFA IRSAD categories, the highest call rate was found in less advantaged remote areas (288.4 calls per 10,000 population; SEIFA IRSAD ranking 2). Four of the five highest average call rates were in SEIFA IRSAD categories 5 and below. In capital cities, the highest call rate was found in SEIFA IRSAD category 6; however, more calls were made from less socioeconomically advantaged postcodes than advantaged postcodes. In remote centres and other remote areas, the calls were spread across the spectrum of low to high advantage. Calls from non-capital city metropolitan areas and large and small rural centres were more common in lower SEIFA IRSAD postcode rankings. Population-adjusted SEIFA IRSAD classification of caller postcodes is shown in Figure 3.
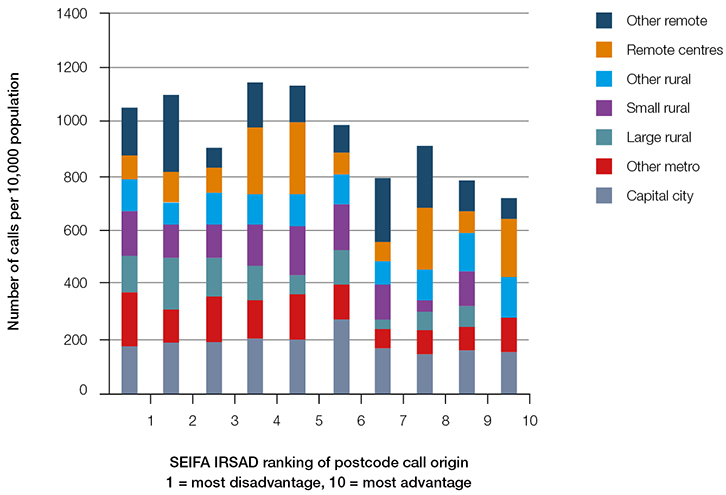 |
Figure 3. Distribution of calls to the AGPH by RRMA and SEIFA-IRSAD classification per 10,000 population (n = 334,654)
Population-adjusted number of calls to the 'after hours GP helpline' (AGPH): Rural, Remote and Metropolitan Areas (RRMA) classification by SEIFA IRSAD ranking of postcode call origin July 2011 − June 2013 |
Figure 4 illustrates the socioeconomic variability of caller residential location. The map shows the number of calls per 10,000 population by postcode and advantage ranking in Sydney, the nation’s most populous city. The six highest calling postcodes (greater than 300 calls per 10,000) were less socioeconomically advantaged, but many postcodes with call rates of between 200 and 300 calls per 10,000 population were at the more advantaged end of the scale.
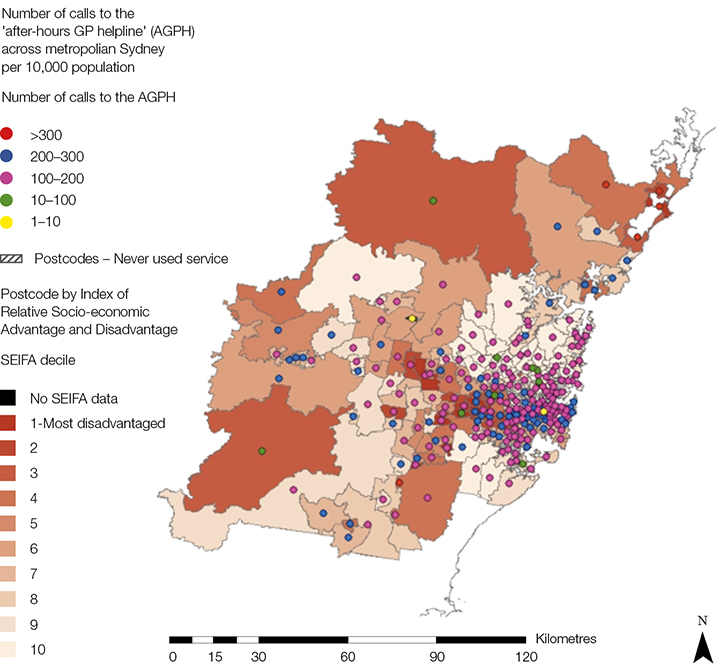 |
Figure 4. Distribution of calls by postcode and SEIFA IRSAD classification in Greater Sydney
Note: multiple dots in the inner city represent multiple postcodes |
Discussion
During its first two years of operation, the AGPH was used most by women; infants and children aged under five years were the biggest patient group. Among adult patients, women aged under 45 years were high users of the service. Older people were proportionally lower users of the service. Although 14% of the Australian population is aged over 65,20 and older people are relatively high users of health services,21 this population group was under-represented in AGPH patients.
These findings on a new Australian after-hours primary care telephone service are in keeping with the profile of users of NHS Direct in England. Younger children represented the largest patient group of the English service, which was identified as an important support to parents of young children.15 Lower use of NHS Direct services by older people was found to reflect factors such as less comfort in using the telephone and preference for face-to-face consultation.14 As older people may have ageing-related health needs and associated difficulties in accessing health services,22 particularly in the after-hours period, targeted promotion of telephone-based primary care advice could assist in better meeting the needs of this growing age group in the Australian population.
People living in remote areas and those who identified as Aboriginal and Torres Strait Islander were proportionally over-represented in their use of the service when compared with current population figures;23 however, there was not strong uptake by those residing in rural areas. Given that access to after-hours primary care services is more limited in rural Australia,24 geographically targeted promotion of telephone-based healthcare advice could increase its use and help better meet the after-hours needs of rural communities.
There is considerable variation by state in the use of the service. State-based use variation may reflect in part variable entry dates to the service, such as Victoria and Queensland, although Queensland’s particularly low use also reflects a lower transfer rate to the AGPH from the state-based nurse triage service 13-Health. Non-urgent and emergency medical coverage of remote Queensland by the Royal Flying Doctor Service may also contribute to lower use. Minimal use of the service by Tasmanians is due to the operation of the pre-existing, well-known ‘GP Assist’ after-hours telephone service in that state.
The socioeconomic status of users is also variable. Similar variability was observed in the use of NHS Direct,11,17 although some NHS Direct studies also found higher levels of disadvantage associated with higher levels of service use.13,17 Slightly higher use of the service in more socioeconomically disadvantaged areas is apparent in our study too, although the service was used across all socioeconomic advantage rankings. In the service establishment phase, variable use may reflect variable awareness of the service, differences in health literacy and help-seeking behaviour across age groups, area of residence and level of advantage, and uneven adoption of new technologies and models of care, as has been found with diffusion of other innovations.25
Limitations
This study has several limitations. The user profile should be seen in the context of the service as a supplement to nurse triage services in the after-hours period. Therefore, it may include users who telephoned the nurse line in the after-hours period, intending to speak to a nurse, but who were offered the opportunity to speak to a GP on the basis of the nurse’s disposition. It may exclude those who specifically called the AGPH telephone number wishing to speak to a GP but were triaged as not needing GP advice. Therefore, not all users of the service were necessarily seeking the AGPH when they called and some intending users may not have reached it.
A further limitation relates to coding of postcode by RRMA. The RRMA was developed in 1994 and is based on 1991 population census estimates. This system of classification was progressively replaced from July 2009 in Australian population analysis. Healthdirect Australia transitioned to use of the Australian Standard Geographical Classification – Remoteness Areas (ASGC-RA)26 system in 2013.
Conclusion
It is important to monitor the characteristics of users of primary care helplines in the after-hours period to ensure that groups with high needs or limited access to healthcare are making appropriate use of the services. While the AGPH has been well used by parents of young children and adult women of reproductive age, relatively low use by some groups is of concern. Targeted promotion may assist underserviced communities, such as those in rural areas and high-need groups (eg older people), to benefit.
Implications for general practice
After-hours primary care telephone advice is sought by consumers with urgent healthcare needs that their regular GP may be unable to meet in that period. Information about the uptake and characteristics of users will help community-based GPs better understand the role of a telephone-based advice service and the potential support it offers to their practices and patients.
Postscript
In September 2015 the ‘after hours GP helpline’ operating model changed to focus on consumers who do not have access to face-to-face GP care in the after-hours period. GP call back is now available to callers who live outside Australia’s major cities across all after-hours periods and those living in major cities in the unsociable after-hours period of 11.00 pm to 7.00 am. Nurse-provided telephone triage and advice continues to be available 24 hours a day in Australian states and territories.
Authors
Rosemary McKenzie BA, PGDipHP, MPH, Director of Teaching and Learning, Deputy Director Centre for Health Policy, Melbourne School of Population and Global Health, University of Melbourne, Carlton, VIC. r.mckenzie@unimelb.edu.au
Michelle Williamson BHlthSci (Hons), Research Fellow, Melbourne School of Population and Global Health, University of Melbourne, Carlton, VIC
Rebecca Roberts BSci, BForSci, BGeoIT, Research Fellow, Melbourne School of Population and Global Health, University of Melbourne, Carlton, VIC
Competing interests: Healthdirect Australia funded the evaluation in 2011–13 on which this study is based. The University of Melbourne received further funding from Healthdirect Australia in 2014–15 to undertake a project led by the first author, RM.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
Professor David Dunt jointly led with Rosemary McKenzie the evaluation of the ‘after hours GP helpline’ 2011–13. Allison Yates was project officer on the evaluation. Maureen Robinson, Mary Byrne and Andrew Cole from Healthdirect Australia facilitated access to data.