Background
In common with many countries, the training of medical graduates for entry into general practice in Australia uses an apprenticeship model of experiential learning in accredited teaching practices (TPs). The content of the experience is an important factor in ensuring that trainees are equipped to enter independent practice. This study uses data from the Bettering the Evaluation and Care of Health (BEACH) study of general practitioner (GP) activity in Australia to explore differences between the clinical activity of general practice registrars (trainees) and practising GPs in TPs and non-TPs.
Previous studies in Australia and elsewhere have found that the patient mix seen by registrars differs significantly from that seen by practising (registered specialist) GPs.1–3 However, direct comparisons between the clinical activity of registrars and practising GPs are scarce. In addition, the extent to which TPs and non-TPs differ in terms of patient mix and clinical activity is not known.
Aims
The aim of this study was to identify differences in the clinical activities undertaken and patient mix seen by general practice registrars and practising GPs who are working at TPs and non-TPs.
Methods
Data from the BEACH program between April 2007 and March 2012 were analysed. Detailed methods for the BEACH program are described elsewhere.4 Approximately 1000 randomly selected, currently active GPs in Australia complete the study each year. Each GP provides data on 100 encounters with consenting patients. Characteristics of the GP participants are also collected on an additional questionnaire.
During this time period, participants were asked whether they were a general practice registrar and whether their major practice taught registrars. In this study, TPs were defined as those at which general practice registrars were taught. For this study, BEACH data were analysed in four groups:
- general practice registrars
- non-registrars at TPs (ie practising GPs)
- all clinicians at TPs (combining registrars and practising GPs in teaching practices)
- GPs at non-TPs.
Results
Between 2007 and 2012, 145 BEACH participants self-identified as registrars and 1527 responded that they worked at TPs but were not registrars. A further 3178 participants indicated that they did not work at a TP (Table 1).
Table 1. Clinical activities of general practice registrars and GPs at teaching practices, and GPs at non-teaching practices
|
| Registrars | Non-registrars at teaching practices | All GPs at
non-teaching practices |
|---|
| GPs (n) |
145 |
1527 |
3178 |
| Encounters (n) |
14,500 |
152,700 |
317,800 |
| Management |
Per 100 encounters (95% confidence interval) |
| Number of problems |
144.7(140.3–149.1) |
162.2(160.5–163.8) |
155.4(154.2–156.5) |
| Number of chronic problems |
40.2(36.4–44.0) |
58.9(57.5–60.2) |
54.8(53.9–55.8) |
| |
Per 100 problems managed (95% confidence interval)
|
| Number of medications(prescribed, supplied or advised) |
68.1(65.3–70.9) |
63.4(62.6–64.3) |
68.1(67.4–68.8) |
| Number of non-pharmacological treatments |
35.8(32.2–39.4) |
38.8(37.8–39.8) |
37.0(36.3–37.7) |
| Number of pathology tests |
34.5(31.6–37.3) |
35.0(34.2–35.8) |
31.4(30.7–32.0) |
| Number of imaging tests |
7.3(6.8–7.9) |
6.6(6.4–6.7) |
6.5(6.3–6.6) |
GP characteristics
The trend towards feminisation of the GP workforce was evident in the sex distribution of registrars. Nearly two-thirds of registrars were female (64.1%; 95% confidence interval [CI]: 56.2–72.0), compared with 40.2% (95% CI: 37.8–42.7) of non-registrars at TPs and 36.4% (95% CI: 34.7–38.1) of GPs at non-TPs (results not tabled).
It is notable that the average age of non-registrars at TPs was younger (49.5 years; 95% CI: 49.0–50.0) than GPs at non-TPs (53.4 years; 95% CI: 53.0–53.8). There were significantly fewer
non-registrars at TPs aged 55–64 years (23.4%; 95% CI: 21.3–25.5) and ≥65 years (7.0%; 95% CI: 5.7–8.2) than GPs in these age groups at non-TPs (30.7% aged 55–64 years, 95% CI: 29.1–32.3; and 14.6% aged 65+ years, 95% CI: 13.4–15.9; results not tabled).
Patient characteristics
Patients seeing registrars were younger (average age 40.9 years; 95% CI: 39.6–42.2) than those seen by non-registrars at TPs (48.9 years; 95% CI: 48.4–49.4) and GPs at non-TPs (47.9 years; 95% CI: 47.5–48.3; results not tabled). The age distribution of patients seen did not differ between TPs and non-TPs, but significantly fewer male patients were seen at TPs (39.7%) than at non-TPs (41.1%). Registrars saw significantly more patients who were new to the practice than non-registrars at TPs and GPs at non-TPs (Figure 1).
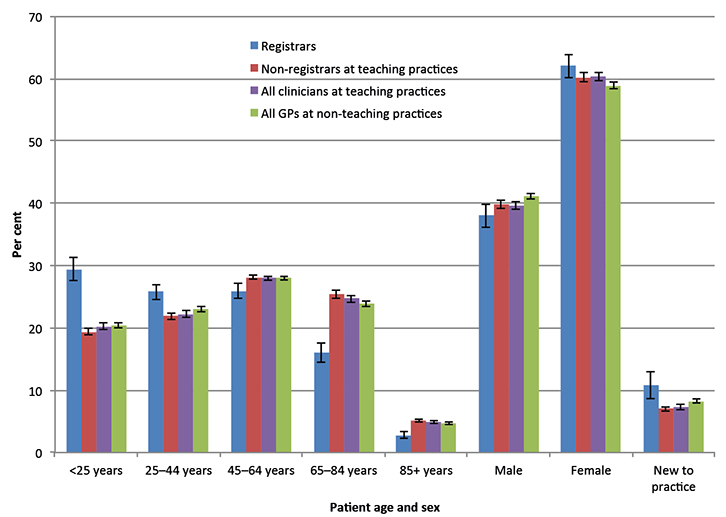 |
| Figure 1. Age and sex distributions of patients seen at encounters |
Problems managed
Registrars managed the lowest average number of problems per encounter, whereas non-registrars at TPs managed the highest average number of problems, significantly more than their counterparts in non-TPs (Table 1).
These findings were reflected in the rates at which chronic problems were managed, with registrars managing significantly fewer chronic problems than non-registrars at TPs and GPs at non-TPs. Non-registrars at TPs managed significantly more chronic problems than their colleagues at non-TPs (Table 1).
Management
Registrars and GPs at non-TPs prescribed, advised or supplied medications at an identical rate (68.1 per 100 problems managed). This is a significantly higher rate than that recorded by non-registrars at TPs (63.4 per 100 problems managed; Table 1).
Higher rates of non-pharmacological treatments were provided by non-registrars at TPs than by GPs at non-TPs (38.8 compared with 37.0 per 100 problems), but there was no difference between registrars and either of the two groups of practising GPs.
Registrars ordered more imaging tests (7.3 per 100 problems) than either non-registrars at TPs (6.6 per 100 problems) or GPs at non-TPs (6.5 per 100 problems). Although pathology test ordering did not differ between registrars and practising GPs at either TPs or non-TPs, non-registrars at TPs ordered significantly more pathology (35.0 per 100 problems) than GPs at non-TPs (31.4 per 100; Table 1).
Discussion
We found numerous differences in the patient mix and clinical activity of general practice registrars, compared with practising GPs in TPs and non-TPs.
Nearly two-thirds of the registrar participants were female, consistent with national figures for the proportion of females undertaking vocational training in general practice (63.1%).5 There are known differences in the patient mix and practice styles between male and female GPs,6 which suggest that the continuing feminisation of the GP workforce may require workforce planning to ensure adequate supply of general practice services.
Findings from this study suggest that GPs at TPs are, on average, younger than those at non-TPs. We were unable to identify which practising GPs at TPs were supervisors, but this finding appears to counter the perception that a large number of GP supervisors are nearing retirement age.7
The age distributions of patients attending TPs and non-TPs were similar, but registrars saw a greater number of younger patients and those who were new to the practice than did non-registrars at TPs. Registrars also managed fewer problems, with almost all the difference due to registrars managing fewer chronic problems. This probably reflects the younger population seen by registrars who have fewer problems managed. Previous Australian8 and Dutch2 studies have expressed concern that registrars are not sufficiently exposed to chronic disease. A Dutch study suggests that ‘exposure to chronic diseases increased steadily during training’.3 Information about the stage of registrar training is not collected in BEACH, so this cannot be tested using BEACH data. Previous research based on BEACH methods suggested that registrar exposure to patients with chronic conditions needed to be improved.1 However, coordinating the patient mix seen by registrars may be complex. Older people in particular may prefer to see their regular GP to maintain continuity of care.9
Conclusion
Through the apprenticeship model of general practice registrar training, registrars should be exposed to a wide range of clinical experiences during their training. The findings of this study could be taken into consideration by training providers when organising training programs.
Authors
Julie Gordon BAppSc (HIM) (Hons), PhD, Research Fellow, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW. julie.gordon@sydney.edu.au
Christopher Harrison BPsych (Hons), MSocHlth, Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Graeme Miller MBBS, PhD, FRACGP, Associate Professor, Medical Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck, Sharp and Dohme (Australia) Pty Ltd, Pfizer Australia, National Prescribing Service Ltd, GlaxoSmithKline Australia Pty Ltd, Sanofi-Aventi Australia Pty Ltd, Bayer Australia Ltd, Janssen-Cilag Pty Ltd, Abbott Australasia Pty Ltd, Wyeth Australia Pty Ltd and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.