Saliva is a complex mixture of water, electrolytes, and organic micromolecules and macromolecules.1 Its secretion is regulated by reflexes involving the autonomic nervous system.1 Serving many roles, saliva is vital not only to one’s daily functioning but also to one’s general wellbeing.2,3 Affecting 10–30% of the general population,2,4 dryness of the mouth is considered to be one of the most common yet underappreciated, underdiagnosed and undermanaged oral health conditions, which can significantly diminish quality of life.3
The problem of mouth dryness is evident across the age spectrum, but is particularly common among the elderly.2 Medication use is the most important risk factor.2,4 Dryness of the mouth has been associated with generalised oral discomfort, difficulty tolerating dentures, dysphonia, dysphagia, dysgeusia, sleep disturbances, halitosis, increased risk of oral mucosal disease, sialadenitis, dental caries, impaired nutritional status, increased risk of depression and social isolation.1,3
What is a ‘dry mouth’?
Mouth dryness may present as a symptom (xerostomia), a sign (salivary gland hypofunction [SGH]) or both.3 Xerostomia is the subjective experience of oral dryness1,3 and diagnosis is based on questioning the individual about their dry mouth symptoms. SGH refers to diminished salivary flow and is based on objective measures of saliva production.1,3 It is generally agreed that an unstimulated salivary flow rate of <0.1 mL/min or a stimulated salivary flow rate of <0.2 mL/min is considered abnormal.1
The relationship between SGH (sign) and xerostomia (symptom) is complex.5 Studies show that mouth dryness is observed when an individual’s baseline salivary output falls by about 50%, but the mechanisms by which decreases in salivary flow are interpreted as the sensation of mouth dryness are not well understood.5,6 Factors besides salivary volume seem important, which is why increasing salivary flow rate in an individual with xerostomia does not necessarily resolve the xerostomia, and why individuals with normal salivary flow rates may also complain of xerostomia.5,7,8 SGH and xerostomia may coexist, but more often than not, one problem presents without the other.8
Causes of SGH and xerostomia
There are many causes of SGH and xerostomia, including systemic disease and/or treatment of systemic disease (Table 1).2,5,9–18 Understanding these causes is important because in some cases, the aetiology can be addressed and mouth dryness eliminated.
The causes of SGH can be broadly attributed to water or metabolite loss, salivary gland injury, or interferences with neural control of salivary secretion.10,12 Although the ageing process has been linked to SGH, it is believed that the functional reserve capacity of the salivary glands compensates for the observed decrease in the number of acinar cells, provided that no additional stresses are placed on the system.2
Table 1. Diseases associated with and iatrogenic causes of SGH and xerostomia
|
|
Developmental
|
- Salivary gland aplasia or agenesis
|
|
Autoimmune/chronic inflammatory
|
- Sjögren syndrome
- Rheumatoid arthritis
- Juvenile idiopathic arthritis
- Systemic lupus erythematosus
- Primary biliary cirrhosis
- Sarcoidosis
|
|
Endocrine
|
- Diabetes insipidus
- Diabetes mellitus
- Hypothyroidism
|
|
Neurological/psychiatric
|
- Anxiety
- Depression
- Parkinson’s disease
|
|
Metabolic
|
- Dehydration
- Chronic renal failure
- Bulimia
- Anaemia
- Alcohol abuse
|
|
Infectious
|
- Human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS)
- Hepatitis C
|
|
Iatrogenic
|
- Graft versus host disease
- Radiation therapy
- Medication
- Anticholinergic
- Sympathomimetic
- Antihypertensive
- Cytotoxic
- Anti-HIV
- Opioids and benzodiazepines
- Antimigraine
|
The causes of xerostomia span beyond inadequate salivary volume. Factors that have been attributed to xerostomia include qualitative changes in salivary composition, such as mucin abnormalities.13 Changes in salivary calcium concentrations have been linked to xerostomia in postmenopausal women.14,15 Other factors that have been associated with xerostomia include:5,16,17
- abnormally low salivary film thicknesses
- oral mucosal disease
- various deficiency states
- changes in patient’s perception mechanisms
- medication use.
More than 500 medications that are currently in use list mouth dryness as a side effect; however, in the majority of cases, the mechanisms are unknown. Nonetheless, it is predominantly believed to be the result of changes in salivary quality more so than the quantity.18
Problems associated with mouth dryness
There are many possible complications associated with persistent mouth dryness, ranging from mucosal discomfort, oral soft and hard tissue disease to significant functional disturbances.1,3 Oral burning sensation is common, although it is not unique to mouth dryness (Table 2).1,19,20 Patients with dry mouth are at increased risk of sialadentitis and oral mucosal disease including mucositis and oral ulceration, and infections such as oral candidiasis (Figure 1).1 A lack of adequate lubrication of the oral mucosa leads to dysgeusia, dysphagia and dysphonia.3 Sleep disturbances arise from the need to relieve xerostomia at night.1
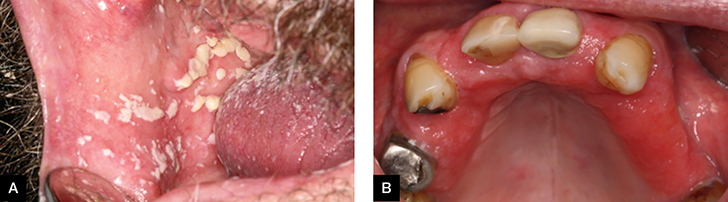 |
Figure 1. Oral candidiasis
(A) Acute oral candidiasis; (B) chronic oral candidiasis (denture stomatitis) |
Table 2. Causes of oral burning sensation
|
|
Local factors
|
- Poorly fitting dentures
- Dental trauma
- Parafunctional habits
- Allergic reactions
- Infections
- Immunologically mediated disease (eg oral lichen planus)
- Chemical irritants
- Galvanism
- Dry mouth (eg post-radiation therapy)
|
|
Systemic factors
|
- Nutritional deficiencies (eg vitamin B12, folate, iron, zinc)
- Endocrine alterations (eg hypothyroidism, diabetes, menopause)
- Dry mouth (eg Sjögren syndrome)
- Medication
- Gastro-oesophageal reflux
|
|
Psychological factors
|
- Anxiety
- Depression
- Obsessive-compulsive disorder
- Psychosocial stress
- Cancer phobia
|
|
Other
|
|
Dental complications are also frequent. Difficulty tolerating dentures is usually due to poor denture retention and increased susceptibility of dry oral mucosa to trauma.1 Dental input is important to ensure that poor denture fit and design are not also contributing to the difficulty tolerating the prosthesis.1 One of the most devastating consequences of persistent mouth dryness is the rapid and preventable loss of dentition (Figure 2). This often occurs as a result of the increased risk of dental caries and erosion posed by the dry mouth environment.1,3 Halitosis may occur as a consequence of decreased oral clearance due to SGH or as a result of dental and oral mucosal disease.1 These wide-ranging consequences of persistent mouth dryness may eventually lead to impaired nutritional status, increased risk of depression and social isolation.1,3
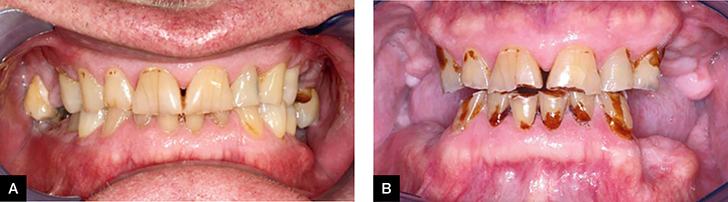 |
Figure 2. Dental status of a patient
(A) before and (B) after radiation therapy-induced dry mouth |
Management of a patient with dry mouth
Successful care of a patient with dry mouth depends on the correct diagnosis, identification of any contributing or causative factors, and appropriate management of all the associated oral mucosal and dental complications. A detailed medical history that includes a careful assessment of all medications and recreational drugs used is paramount. Oral examination will determine the presence or absence of saliva in the mouth. In some individuals, it may be possible to eliminate or significantly improve mouth dryness by addressing the underlying medical condition. Medication changes may be considered, if it is safe to do so, and if the symptomatic management of mouth dryness has failed. The importance of adequate hydration cannot be overstated. In cases where the cause is unknown, or cannot be eliminated, consideration may be given to the use of oral lubricants, antimicrobial saliva substitutes or salivary stimulation.21,22
Oral lubricants may be used to manage xerostomia. One of the simplest and cheapest substances that may be used as an oral lubricant is olive oil, which has been shown to be of some benefit in patients with medication-induced xerostomia.23 There is also a wide range of commercially available oral lubricants, predominantly based on the carboxymethylcellulose (CMC) gel.21 Examples of such products include the Biotene product range (GalaxoSmithKline), GC dry mouth gel (GC corporation), Aquae range (Hamilton Company) and Colgate dry mouth relief mouthwash (Colgate-Palmolive Company). Products such as the Oral7 range (Pharma 777) also incorporate antimicrobial agents such as lactoferrin, lysozyme and lactoperoxidase, which are naturally found in saliva.24 Oral lubricants and antimicrobial salivary substitutes may be applied as a bolus to the oral mucosa or used in custom-made, intra-oral slow-release devices.25 Despite this range of treatments, none of the currently available products adequately reproduce the complex makeup of saliva and their usefulness is therefore limited.25 The duration of action is usually very short (due to the water-soluble nature of the CMC gel) and the low pH of some products may contribute to dental erosion.21
Salivary stimulation can be used in the management of SGH and xerostomia, and may be considered in an individual with functioning salivary gland tissue. It can be achieved by the use of chewing gum, pharmacologically or through the use of electro-stimulating devices.7,21,22,25 Chewing any gum, importantly, sugar-free, will stimulate saliva, but certain products are specifically marketed for that purpose. Such products often contain additives claimed to provide further benefits, predominantly pertaining to prevention of dental caries.21 Although chewing gum is effective in stimulating saliva, its usefulness in the management of xerostomia is limited, highlighting the complex nature of the relationship between SGH and xerostomia.25 However, the benefits of salivary stimulation are wider-ranging, including a decreased risk of dental caries.21
A novel way of stimulating saliva includes the use of electro-stimulating devices such as the Saliwell device (Saliwell Ltd), which was developed in Israel.22,26 It is designed to augment the salivary reflex and directly stimulate the efferent neural pathways of the submandibular and sublingual salivary glands by strategic placement of the stimulating electrodes, which can be incorporated into a removable device or a dental implant.22,26,27 At present, the literature pertaining to the effectiveness of electrostimulation on dry mouth symptoms is limited.28
Salivary stimulation can also be achieved through the use of secretagogues such as pilocarpine.7 Pilocarpine is effective in stimulating saliva; however, a disconnection exists between the objective measures of salivary production and subjective reporting of xerostomia, with the objective response dominating the subjective one – the objective response of increased salivary production by pilocarpine does not always translate to the same degree of symptom improvement. This disconnection arises from our poor understanding of xerostomia.7,29 Numerous adverse effects and drug interactions limit the use of oral pilocarpine, and it is generally contraindicated in individuals with significant cardiovascular and pulmonary disease.7
The care of a patient with dry mouth must also encompass management of any potential oral mucosal and dental complications. Mucosal diseases, such as oral candidiasis, mucositis, and the increased risk of oral ulceration are managed through the use of appropriate antimycotic agents and by reducing exposure to irritants such as alcohol, smoking and hot or spicy food. Mucosal trauma from a dental prosthesis can be minimised by ensuring adequate fit. The main dental problem encountered in the dry mouth environment is the high risk of dental caries, which all too often leads to the devastating, yet preventable, loss of dentition.30 Prevention of dental caries is multifaceted and includes regular dental care, maintenance of meticulous oral hygiene, fluoride use, and dietary modifications to minimise the consumption of cariogenic (high in simple sugars) and acidic foods.31
Unfortunately, mouth dryness can, and often does, alter food choices, frequently in favour of cariogenic foods.1 The link between a cariogenic diet and dental caries is well established.32 It is imperative to provide appropriate dietary counselling that focuses on the elimination of foods high in simple sugars, and advise avoidance of sugar-containing medications if possible. Halitosis can be prevented by ensuring good oral hygiene and appropriate management of oral mucosal and dental disease.
Conclusion
Mouth dryness is a common and growing problem.33 It is also a potentially difficult problem to manage as the associations between SGH and xerostomia are complex and poorly understood. While oral health complaints are generally left to the dental professional to manage, mouth dryness is often not only associated with systemic disease and/or its treatment, but may also have a significant impact on an individual’s general wellbeing. Successful management of mouth dryness is dependent on the effective communication between the dental and medical professions. Management of the problem should focus on identifying and eliminating the cause, if possible. In situations where mouth dryness is expected to be a persistent problem, oral lubricants, antimicrobial salivary substitutes or salivary stimulation may be considered. It is also crucial to appropriately manage the potential oral mucosal and dental complications of mouth dryness.
Author
Agnieszka M Frydrych BDSc (Hons), MDSc (Oral Med/Oral Path), FRACDS (Oral Med), FOMAA, FPFA, Associate Professor (Oral Medicine), School of Dentistry, University of Western Australia, Crawley, WA. agnieszka.frydrych@uwa.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.