Traumatic brain injury is one of the most common causes of neurological morbidity, and is more common in childhood and adolescence than at any other time of life.1–3 Concussions in young people account for 90% of all traumatic brain injuries.4 One in five children will experience a concussion by the age of 10 years.5 Falls (51%) and sports-related activities (25%) are the most common causes of concussion.5,6 The highest rates of sports-related concussion are reported in males aged 10–19 years, although young females also sustain concussions.7,8 Contact football has the highest reported rate of concussion, although all sports-related activities entail some risk.9 Early detection of injury, proper evaluation and appropriate decision-making for return to activity (physical and cognitive) remain paramount for the treating clinician in the care of post-concussive injury in young people.
Definitions and presentation
Concussion is defined as a form of mild-traumatic brain injury that occurs as a result of a direct impact to the head or impact to the body that causes transmission of forces to the head and brain.10 In terms of initial presentation, common early symptoms include:
- headache
- dizziness
- vertigo or imbalance
- lack of awareness of surroundings
- nausea
- vomiting.
Confusion is another hallmark of concussion and may include amnesia, usually of the traumatic event, but can frequently include losing recall of events immediately preceding a traumatic insult.11 Previous generations of concussion experts have defined loss of consciousness as necessary for the diagnosis of concussion, but nowadays, this is not the case; indeed, loss of consciousness is noted in only 8–10% of concussion cases.12 Patients with a concussion usually experience symptomatic recovery within 2–10 days of injury.6,8 However, this can vary, particularly in cases where concussion is complicated by other factors and important comorbidities. Symptoms experienced by patients in the context of concussion can vary widely and evolve over time. This makes it difficult, and indeed inaccurate, to predict the severity of total symptom load for a patient at the time of injury (Figure 1).13
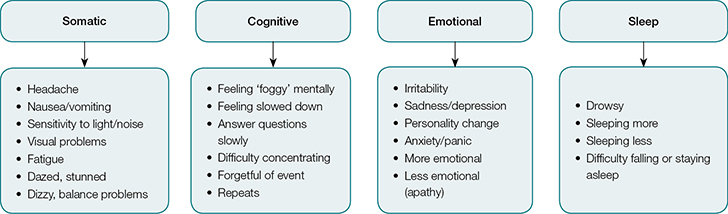 |
| Figure 1. Concussion clinical domains |
Concussion in the immature brain
The paediatric brain has different mechanical and compositional properties (eg increased water content, decreased myelin, increased transition of acceleration-deceleration forces due to decreased neck strength). This results in an increased potential for brain tissue displacement and shear injury.14,15 These properties can amplify the complex neurometabolic cascade that follows a concussive injury, resulting in increased vulnerability of the immature brain to secondary insults (eg second-impact syndrome) and more prolonged recovery.16–18 Further, the prefrontal cortex, the region responsible for executive function, is particularly vulnerable to injury in adolescence.18,19
The fundamental domains of interest in the clinical assessment of children and adolescents with concussion parallel those of adults, but there are important differences. Assessment of children and adolescents must be framed within the context of differences in:20
- neuronal development
- physical, cognitive, behavioural and emotional maturation
- the influences of home, school and community supports
- demands placed on the child and adolescent.
Responses to concussive injury in children and adolescents must therefore be treated as unique to the individual.
Initial assessment
Exclusion of other significant structural trauma, a preliminary diagnosis and immediate withdrawal from play are important in the acute stage after a concussive-type blow. Rare but life‑threatening entities to consider include:
- intracranial haemorrhage
- extradural haematoma
- cervical spine injury
- other acute intracranial injury
- skull fracture.
Players who show signs of more severe or life-threatening injury should be immobilised using appropriate C-spine precautions and transferred to the nearest emergency department. If these conditions have been tentatively excluded in the initial assessment, the player should be removed from play. Thereafter, the sideline examination can be conducted using Child-SCAT (Sports Concussion Assessment Tool) for children, SCAT3 for adolescents or the Pocket Concussion Recognition Tool (refer to Resources).2 The presence of any symptom should prompt removal of the young person from the game. Suspicion of concussion is further supported by changes in vision, balance and cognitive function using the SCAT framework.
Following the initial sideline assessment, the young concussed person should be systematically re-evaluated at 15-minute intervals to ensure their condition stabilises. Educating the young person being sent home and the caregiver about reporting and monitoring any features of deterioration until follow-up assessment in primary care is critical. At home, parents should monitor the young person who has had a concussion for the development of any of the features of HEAD BUMPS (Figure 2). Should any of these symptoms occur, and are of concern to parents, or if they are progressively worsening, the parent/player should seek urgent medical assistance.
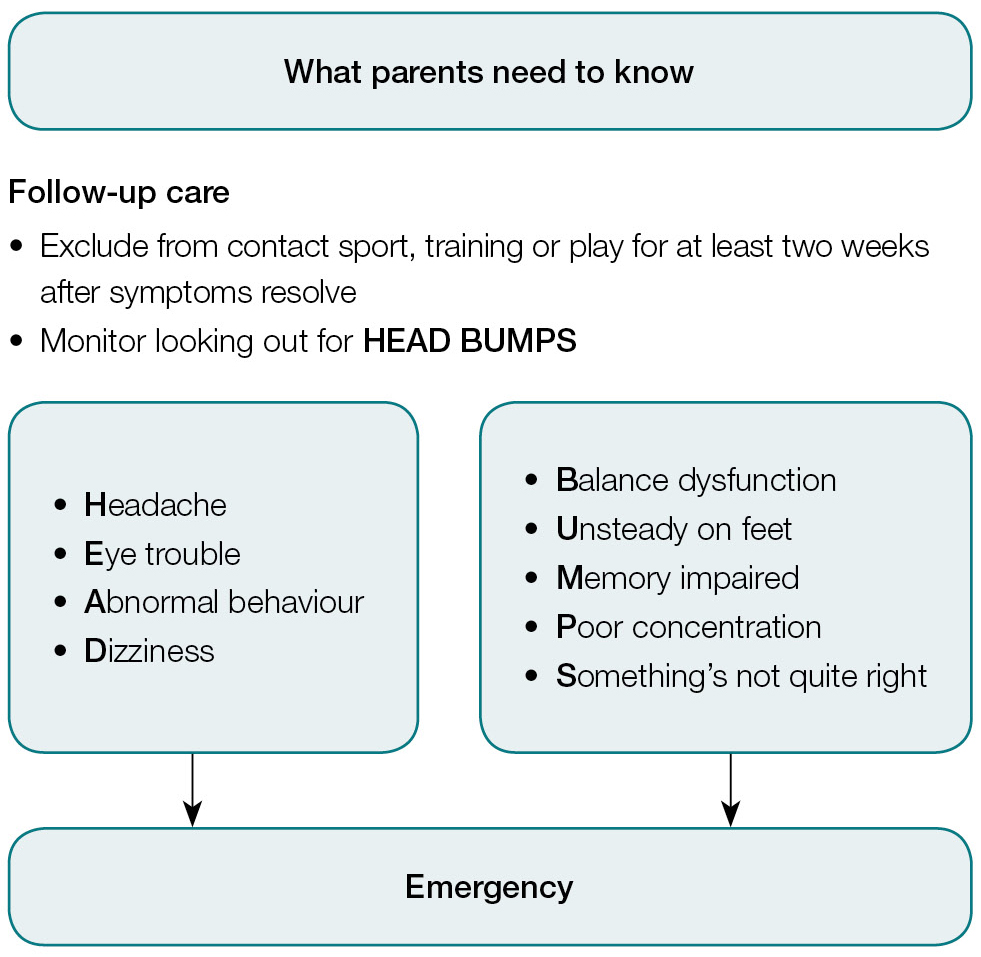 |
| Figure 2. Look for HEAD BUMPS in young children post-discharge |
Integrated recovery model
The current understanding of concussion in children and adolescents converge around an integrated model of clinical and physiological recovery. This model proposes a progression of recovery characteristics from an acute period of clinical signs (eg symptoms, functional abilities and concurrent physiologic dysfunction) to persistent physiological dysfunction in the post-acute period (after resolution of clinical signs of injury) and, finally, complete clinical and physiological recovery.21,22 This model proposes that for satisfactory resolution of concussion to occur, the clinical and physiological injury must have resolved, as the young person with concussion remains vulnerable to secondary injury throughout these phases.
Primary assessment – Re-evaluation in primary care
At the first follow-up appointment, the initial approach should be to verify the diagnosis of concussion by carefully documenting the history of recent head impact together with symptoms and signs of concussion that have followed. Some young people have subtle changes or may be unaware of change following injury, making the diagnosis less than certain. As not every symptom complex experienced by a young person following a contact play in sports is caused by a concussion, differential diagnoses should consider concussion mimics (eg heat illness, migraine headache or even benign positional vertigo). A focused assessment and observation over a short time period will resolve this dilemma in most cases.
At this point in time, concussion remains a clinical diagnosis as determined by the attending clinician.23 Therefore, the key to assessment in primary care is a thorough, focused concussion assessment using the four pillars of concussion evaluation:23–25
- History
- Physical examination with focused neurological assessment
- Balance testing
- Cognitive testing.
The assessment begins with a careful history of how the injury was sustained to understand the concussive event, determining the patient’s symptoms and severity, and asking about potential factors or comorbidities that may influence recovery (eg previous concussions).26 Factors such as a loss of consciousness, amnesia or impact seizure activity are not reliable enough or sensitive enough for diagnostic purposes, but should be sought on history.
If any one or more of the symptoms of concussion are present in a young person following a recent head injury, then concussion should be suspected. It is typical for a young person’s symptoms to fade or stabilise during the acute post-injury period;6,8,9 however, increasing severity requires due diligence to exclude serious injuries. Risk factors such as younger age, female gender, history of migraine or behavioural disorder, nature of sport/activity undertaken and history of prior concussion should be explored during history-taking and documented. These risk factors make some patients more susceptible to injury and cause others to have a prolonged recovery. This information should ideally be gathered from someone who witnessed the episode or a parent in the case of a young child or an uncooperative adolescent. In an increasing number of cases, the parent or young person will often have a video recording of the event on their electronic devices.
A general physical examination is important as autonomic instability may manifest with symptoms such as postural dizziness. A comprehensive neurological examination should be completed, focusing on cognitive function, eye movements, balance and gait, and coordination.27 Post-traumatic amnesia should have resolved by this stage, and if it is prolonged, a more serious injury should be considered. The young person can be asked Maddock’s questions (SCAT), which assess attention and memory. The Abbreviated Westmead Post-Traumatic Amnesia Score (A-WPTAS) is now widely used to assess for amnesia, and is a valid measure of post-traumatic amnesia in amateur athletes.28
Focal neurological findings (eg abnormal pupillary responses, extraocular movements and motor or sensory functions) raise concern over serious traumatic brain injury and should initiate immediate referral for emergency department review, neurosurgical assessment and neuroimaging. Abnormalities in the gaze system are evaluated and, together with the vestibular system, can be affected following a concussion. These tests include static acuity testing, ocular alignment testing, smooth pursuits, saccades testing and abnormal near point convergence testing. Together with the vestibular ocular reflex test, they are collectively known as the vestibular ocular motor screening (refer to Resources).
One of the most consistent findings in concussion is postural instability. Station is tested by observing the young person while they are standing still. The clinician examines a patient’s ability to maintain balance, including their posture and feet positioning. The primary care physician should also document the compensatory mechanisms to maintain balance. Gait examination is assessed in the presence of the patient’s parent or guardian, and any deficits or changes noted. Romberg, together with Tandem-Romberg tests is sensitive for subtle postural change in young people.20
Neurocognitive testing, which includes auditory, visual and working memories, processing speed and executive function, is important as it can not only reveal impaired cognitive function, but also demonstrate sequential recovery.8 While comprehensive neurocognitive testing in primary care is impractical, an abbreviated form using the SCAT framework is less time‑consuming in providing this valuable clinical information (refer to Resources).
When interpreting the clinical information obtained from the concussion examination, the primary care physician must be aware that there is wide variation in acquisition of developmental skills among young people. As it is not routine to perform baseline pre-participation testing in Australia, the lack of reference values for some of these tests limits their clinical utility in the young. The primary care physician can resolve this problem by repeating the assessment at frequent intervals, as well as enquiring about the young person’s pre-injury status to the parent or guardian.
Management in primary care
Anticipatory guidance is the mainstay of management in primary care. Reassurance, education about the injury and brief psychological counselling in the early phase can reduce the risk for later development of post-concussion syndrome.29 Rest is the initial intervention and best used as needed and tolerated, but not overdone.30 Severe and prolonged restriction of activity, referred to as ‘cocoon therapy’, can prolong symptoms.31,32 Controlled activity (cognitive and physical) in patients with rapidly resolving symptoms should be considered.33–36 Provided that the patient’s activity remains below the symptom threshold in which a patient is still injured but not producing a detectable clinical syndrome, progressive challenges with controlled activity can improve symptom tolerance.37,38 This has led to the concept of early ‘relative rest’, a degree of activity that is reached by careful evaluation of symptom exacerbation brought on by any particular activity.39
Imaging is unnecessary in the young person with a typical concussion. The primary care physician should explain to the family that existing evidence for simple sports concussion suggests that computed tomography (CT) has little advantage over simple observation, even in the primary care context.40,41 Once this has been discussed, aspects of concussion management can then be best framed into three distinct management phases. Each phase is defined by the current clinical experience of the individual patient. These time frames are only estimates, and are often longer in younger persons and those with complicating comorbid diagnosis.
Acute rest phase (2–5 days)
Because of their severity, acute symptoms significantly limit cognitive and physical activities. A brief period of physical and cognitive rest is initially recommended. During this phase, the young person is typically unable to tolerate routine activities of daily living. This is also the best time to set expectations for recovery.39
Total resolution of symptoms at this stage is not necessary prior to resuming school. However, it is important to balance cognitive exertion and rest and, if done well, most young people will be absent from school for only two to three days (Table 1).39
Supportive care is critical and includes a healthy diet and good nutrition, adequate hydration, avoidance of meal-skipping and good sleep hygiene. Symptoms such as headache, nausea and sleep disturbance can be addressed with medications as they would in patients who are non-concussed.39
Table 1. Graded return to school
| Stage |
Activity |
Practical implications |
Teacher notes |
| 1 |
- No cognitive activity as long as there are symptoms
|
- Complete cognitive rest at home (including screen time*, TV)
|
|
|
Can go to next stage if no headache, and concentration and fatigue have significantly improved
|
| 2 |
|
- Attend school 3 half-days a week
(or build up to this)
- Rest periods during recess (no sport)
- Rest days in between with minimal
screen time*
|
- Reduce workload and have less complex learning objectives
- Allow the student to ‘audit’ the material rather than need to learn (eg provide notes to highlight rather than having to take notes)
- Exempt student from routine work or tests
- Ask about symptoms after class
|
|
Progress to next stage if no headache after half day, and concentration and fatigue have significantly improved to be able to tolerate full day
|
| 3 |
- Moderate and more frequent cognitive activity
|
- Attend school full-time with frequent rest periods at recess and lunch
|
- Reduce workload and have less complex learning objectives
- Exempt student from routine work or tests, minimal homework
- Ask about symptoms after class
|
|
Progress to next stage if no headache after full day, and concentration and fatigue have significantly improved
|
| 4 |
- Return to school full-time
- Increase cognitive load
|
- Increase cognitive load during school
- Increase homework load (individualised)
|
- Increase cognitive load to a moderate level
- Re-introduce complex learning objectives, routine work and tests as tolerated, with accommodations
|
| 5 |
- Back to regular,
full cognitive activity
|
- Able to participate in all school
academic activities
|
|
|
*Screen time is defined as time on the computer, phone (texting/calling), social media, computer games, video games, watching TV or DVDs
|
Relative rest phase (5–7 days)
During the relative rest phase, the young person is symptomatic, but not to a degree that consistently limits routine activity. Return to school is the focus and, as cognitive stamina is limited, any prolonged cognitive activity required by school attendance and participation should be shortened. Introduction of reading, computer work and schoolwork within symptom threshold is now appropriate. Liaison by the general practitioner (GP) with the young person’s teacher can ensure cooperation with this strategy at school. As a general rule, most young people are ready to return to school once they are asymptomatic or can comfortably tolerate more than 30 minutes of cognitive activity (Table 1). 39
The use of medication to control concussion symptoms should begin to be tapered and limited at this stage. At this point, facilitated low-impact exercise may be re-introduced.36,37 This phase heralds the beginnings of physiological recovery with cognitive and exercise tolerance, although not to pre-injury levels.39
Graduated exertion phase (7–14 days)39
The young person should not be using medications for the treatment of concussion-related symptoms at the graduated exertion phase. At this stage, they should have completed a full return-to-school program. Once back at school, they are ready to undergo an active process of return to play (Table 2). The activity plan should proceed with a minimum of 24 hours spent at each level.24,37,38
As young people have a more prolonged recovery from concussion, it makes sense to be cautious in returning the patient to contact sport. A minimum of 14 days from when symptoms cease before returning to full-contact sport (after medical clearance) is the safest approach in primary care and recommended by the Australian Institute of Sport and the Australian Medical Association (AMA).42
The concussion care plan described here is intended for the patient with a typical concussion recovery pattern, in which symptoms abate in response to cognitive and physical rest, and the individual is able to gradually increase cognitive and physical activity via a controlled ramp-up over the course of three to four weeks.
Table 2. Graded return to play10
| Stage |
Activity |
Functional exercise |
Child or student equivalent |
Objective of stage |
| 1 |
No physical activity as long as there are symptoms
(days or weeks) |
Complete physical rest |
Quiet time with maximum rest |
Recovery |
|
Proceed to Stage 2 when 100% symptom-free for 24 hours. Younger children may need 48–72 hours
|
| 2 |
Light aerobic activity |
Walking, swimming, stationary cycling, 10–15 minutes, no resistance exercise (eg weights) |
Solitary play or quiet play alone or with parent |
Increase heart rate (light-to-moderate workout that does not require high degree of coordination or cognitive attention ) |
|
Return to the previous stage if symptoms re-emerge with this level of exertion.
Proceed to the next stage if the child remains symptom-free for 24 hours after this level of exertion.
|
| 3 |
Sport-specific exercise |
Running/cycling/ball skills for 20–30 minutes. No weightlifting or head contact |
Supervised play, low-risk activities |
Add movement (increased attention and coordination required) |
|
Return to the previous stage if symptoms re-emerge with this level of exertion.
Proceed to the next stage if the child remains symptom-free for 24 hours after this level of exertion.
|
| 4 |
Non-contact training drills |
Progression to more complex training drills; may start progressive resistance training |
May run or jump as tolerated |
Exercise, coordination (mimics athlete’s sport without risk of head injury) |
|
Return to the previous stage if symptoms re-emerge with this level of exertion.
Proceed to the next stage if the child remains symptom-free for 24 hours after this level of exertion.
|
| 5 |
Full-contact practice |
Following medical clearance, participate in normal training activities; full exertion |
Normal participation with parental or adult supervision |
Restore confidence and assess functional skills by coaching staff (or family) |
|
Return to the previous stage if symptoms re-emerge with this level of exertion.
Proceed to the next stage if the child remains symptom-free for 24 hours after this level of exertion.
|
| 6 |
Return to play |
Normal game play |
Normal playtime |
No restrictions |
Secondary assessment – Specialist concussion service
A proportion of patients (15–20%) have symptoms that do not resolve with appropriate intervention. Management of patients with this atypical recovery is challenging and best referred to a specialist clinic that can provide a multidisciplinary and interdisciplinary approach to care (eg the Children’s Institute of Sports Medicine at the Children’s Hospital at Westmead,
www.schn.health.nsw.gov.au/parents-and-carers/our-services/sports-and-exercise-medicine/chw.
Long-term risk
Tremendous concern exists about neurodegeneration induced by repetitive concussions – chronic traumatic encephalopathy. Unlike the dose–response relationship reported in professional athletes, the risk of long-term cognitive sequelae in children is uncertain. The relationship between repeated concussions and chronic neurocognitive impairment appears less consistent in adolescents.43,44 This does not imply that no risk exists for chronic problems after concussion in young people and more study is needed.44
Conclusion
Although our understanding of concussive injury is evolving, concussion remains a clinical diagnosis, with clinicians assessing patients using standard clinical assessment methods. The education of patients, parents and sporting groups acts as a catalyst for ongoing change. Prevention strategies are critically important, and the GP stands as a key agent for change in this field, as the best prevention is good concussion care.
More information for parents and physicians can be found at www.sitoutconcussion.org.au, a free service made available through Concussion Clinical Services, Children’s Hospital Institute of Sports Medicine, The Children’s Hospital at Westmead, Sydney Children’s Hospital Network.
Authors
Gary J Browne MD, MBBS, MSpMed, FRACP, FACEM, FAAP, Medical Director, Concussion Service, Children’s Hospital Institute of Sports Medicine (CHISM), Children’s Hospital Westmead, Sydney Children’s Hospital Network, Westmead, NSW. gary.browne@health.nsw.gov.au
Stefan Dimou MBBS, Concussion Service, Children’s Hospital Institute of Sports Medicine (CHISM), Children’s Hospital Westmead, Sydney Children’s Hospital Network, Westmead, NSW; Westmead Hospital, Westmead, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Resources