Pregnancy is commonly managed in general practice.1 In contrast to the UK, Canada and New Zealand, where general practitioner (GP) involvement in pregnancy care has decreased, GPs in Australia continue to be high providers of antenatal care.2 However, there is very little published research about the antenatal care provided by GPs in Australia.
Australia has consistently had lower maternal and perinatal death rates than the majority of comparable Organisation for Economic Co-operation and Development (OECD) countries over the past decade. This makes Australia one of the safest countries in the world in which to give birth or to be born.3 The World Health Organization recommends that expectant mothers receive antenatal care at least four times during pregnancy.4 Australian guidelines for antenatal care recommend having the first antenatal visit within the first 10 weeks of pregnancy and 7–10 follow-up visits.5 Australia’s record on antenatal care provision is sound, where 87% of women who gave birth in 2013 had seven or more antenatal visits.6
Australian women have a variety of options for antenatal care, many of which involve their GP. The aims of this article are to describe the content of pregnancy-related GP visits, and how pregnancy and pregnancy-related problems are managed by GPs.
Method
Data from the Bettering the Evaluation and Care of Health (BEACH) program, a national study of general practice activity in Australia, involving encounters where pregnancy was managed for patients aged less than 55 years, were analysed. The encounters were limited to those recorded between April 2010 and March 2015. BEACH methods are described in detail elsewhere.7
The problems managed were classified according to the International Classification of Primary Care, Version 2 (ICPC-2).8 Pregnancy-related encounters were defined as those at which one or more of the following problems were managed:
- pregnancy, including pregnancy check-ups and antenatal care (ICPC-2 code W78, W30 and W31010)
- unwanted pregnancy (W79)
- vomiting/nausea in pregnancy (W05)
- high-risk pregnancy (W84)
- antepartum bleeding (W03)
- toxaemia of pregnancy (W81)
Encounters where gestational diabetes mellitus (GDM) was managed without one of the above problems also managed were excluded; GDM requires monitoring after pregnancy and we could not determine whether the patient was pregnant at the time of the consultation. Encounters involving pre-conceptual counselling and testing for pregnancy were also excluded if pregnancy had not been confirmed.
Ethics approval for the BEACH program was obtained from the Human Research Ethics Committee of the University of Sydney.
Results
Between April 2010 and March 2015, 7335 pregnancy-related problems were managed at 7222 GP encounters. These encounters accounted for 2.71% of all GP–patient encounters during the study period.
On average, GPs managed 2.8 pregnancy-related problems per 100 total encounters and 4.5 per 100 encounters with female patients. Extrapolation of our results suggests that nationally, on average, there were about 1.9 million (95% confidence interval [CI]: 1.8–2.0) encounters per year involving the management of pregnancy-related problems.
 |
|
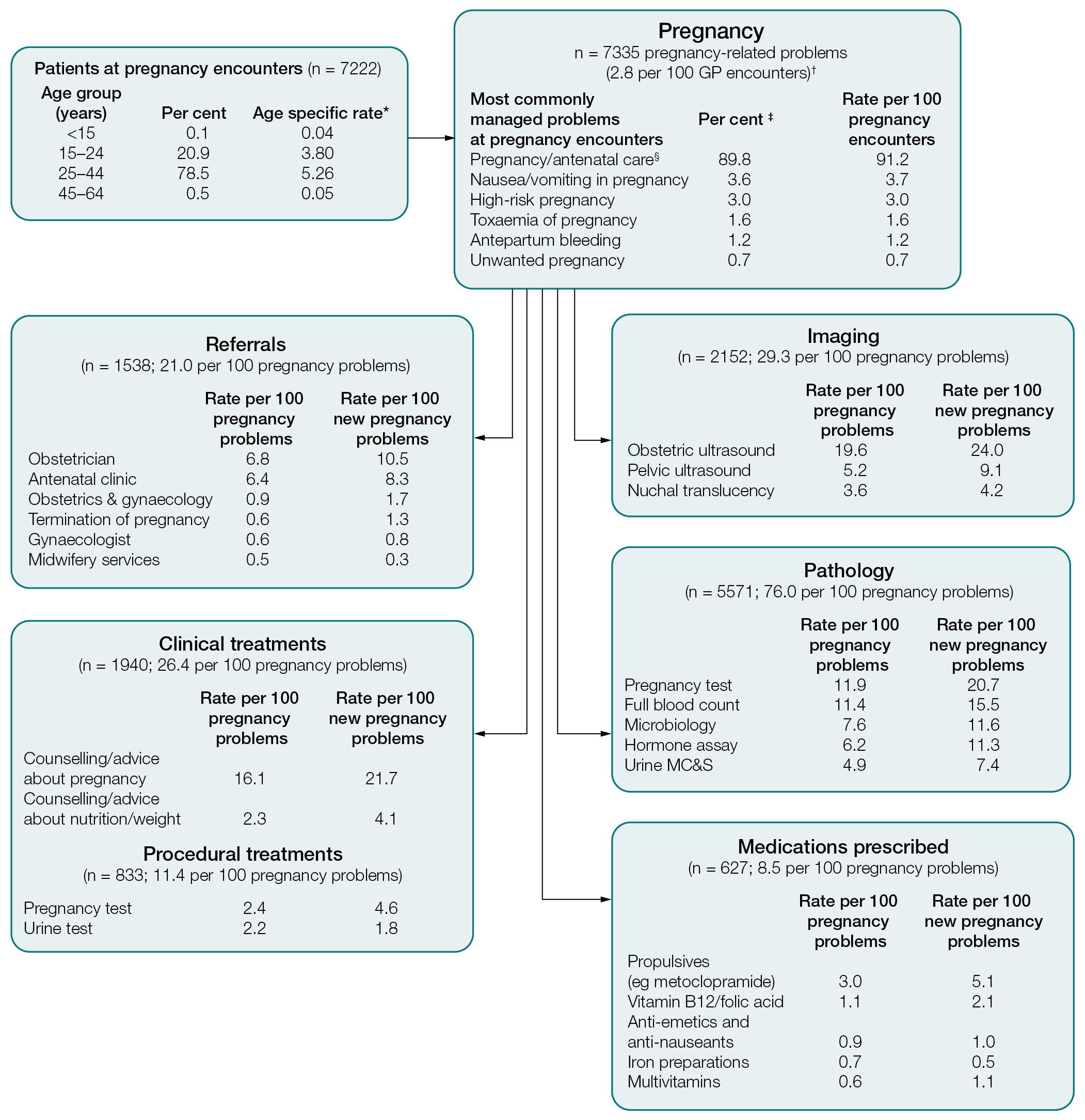
Figure 1. Content of encounters where pregnancy was managed
Note: medications were classified according to the World Health Organization's Anatomical Therapeutic Chemical (ATC) classification level 4.
*Specific rate per 100 encounters with patients in each age group;
†encounters with patients aged younger than 55 years recorded between April 2010 and March 2015;
‡per cent of all pregnancy problems managed (n = 7335);
§includes multiple ICPC-2 and/or ICPC-2 PLUS codes MC&S, microscopy, culture and sensitivity
|
Figure 1 shows that most patients at pregnancy encounters were 25–44 years of age (78.5%) and 20.9% were 15–24 years of age. Very few patients were aged 45 years or older (0.5%) or under 15 years (0.1%). Most encounters (91.1%) with women who were pregnant occurred in a practice they had previously attended and 53.9% of encounters were with female GPs. In 2014–15, 42% of active GPs in Australia (according to BEACH selection criteria1) were female.
Pregnancy and routine antenatal care accounted for 89.8% of pregnancy-related problems managed by GPs, followed by nausea/vomiting in pregnancy (3.6%; Figure 1). Other commonly managed problems at pregnancy encounters included upper respiratory tract infection (1.7 per 100 pregnancy encounters), vitamin/nutritional deficiency (1.3 per 100 pregnancy encounters), test results (1.1 per 100 pregnancy encounters), depression (1.0 per 100 pregnancy encounters) and anxiety (1.0 per 100 pregnancy encounters). These results are not tabled.
New pregnancy-related problems resulted in significantly more management actions (eg referrals, clinical treatments, pathology tests, imaging tests, prescribed medications) than previously managed problems. Overall, GPs ordered 76.0 pathology tests and provided 21.0 referrals per 100 pregnancy-related problems. This is more than double the average pathology test rate (30.3 per 100 problems) and referral rate (10.3 per 100 problems) for all problems managed in 2014–15. The imaging order rate (29.3 per 100 pregnancy problems) was four times the average of 7.4 per 100 problems.
Medications were prescribed at a very low rate (8.5 per 100 pregnancy problems), compared with the average rate of 55.2 per 100 problems. However, significantly more over-the-counter medications were advised (results not tabled; 8.0 per
Medications were prescribed at a very low rate (8.5 per 100 pregnancy problems), compared with the average rate of 55.2 per 100 problems. However, significantly more over-the-counter medications were advised (results not tabled; 8.0 per 100 pregnancy problems) than the average (6.1 per 100 problems).
Discussion
These findings provide relevant and recent information about GP management of pregnancy and pregnancy-related conditions. GPs provide important services to women seeking pregnancy-related healthcare. The rate at which pregnancy tests were performed at encounters (4.6 per 100 new pregnancy-related problems) suggests that GPs have an important role in confirming early pregnancy.
The high rate of management actions undertaken when managing pregnancy problems reflects the number of pathology tests, imaging orders, nutritional and supplement advice, and referrals recommended under Australian guidelines for antenatal care.5 The rates and categories of medications prescribed are also broadly in keeping with Australian antenatal guidelines.5 Interestingly, GPs provided more nutritional and weight advice at pregnancy-related encounters (4.1 per 100 pregnancy problems) than average at all general encounters (rate 1.9 per 100 overall problems).
In Australia, pregnant women have a number of options regarding antenatal care and birth in the public or private health system. In the public system, most women receive care through an obstetrician-led antenatal clinic or midwives clinic in a public hospital.9 Women can also choose to see a GP and an obstetrician at a public antenatal clinic through a shared-care program, which has been shown to reduce public clinic waiting times10 and improve caregiver continuity.11 In our study, it was clear that pregnancy-related care was commonly provided (91%) in a practice the woman had previously attended.
In this study, we were not able to identify patients seen as part of a GP shared-care program and unable to determine how these encounters differ from those of other antenatal care services. The study only included encounters with patients who were known to be pregnant at the encounter. Notably, GDM was excluded because this label is also used in the postnatal period.
Despite the decline in the number of GPs involved in procedural obstetrics over recent years,12,13 pregnancy remains an important part of Australian general practice and GPs continue to play a crucial role in the provision of maternity services in Australia.
Authors
Carmen Wong BHS, MHI, Research Officer, School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Julie Gordon BAppSc (HIM) (Hons), PhD, Research Fellow, School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Ying Pan BMed, MCH, (formerly) Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Joan Henderson BAppSc (HIM) (Hons), PhD, (formerly) Deputy Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW
Helena Britt BA, PhD, Professor of Primary Care Research, School of Public Health, Sydney Medical School, University of Sydney, Parramatta, NSW. helena.britt@sydney.edu.au
Competing interests: None
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck, Sharp and Dohme (Australia) Pty Ltd, Pfizer Australia, National Prescribing Service Ltd, GlaxoSmithKline Australia Pty Ltd, Sanofi-Aventis Australia Pty Ltd, Bayer Australia Ltd, AbbVie Pty Ltd and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.