There is a variety of antenatal care service models in Australia including:1
- the traditional obstetrician-led clinic approach
- midwifery-led models including group practice and midwifery teams
- models centred on culturally appropriate care (eg models for Aboriginal and Torres Strait Islander women and culturally and linguistically diverse [CALD] women)
- group assessment and care models
- antenatal shared care (ANSC).
Antenatal shared care (ANSC) is described in Australia as a service delivery model whereby ‘several health professionals are involved in the care of a woman during her pregnancy, often in the context of a formal arrangement’.2 General practitioner (GP)-led ANSC aims to provide pregnant women with flexibility, choice and continuity of care, while enhancing the skills of GPs working with pregnant women and promoting better communication between GPs and the antenatal clinic.3 An additional benefit of any shared care model is the reduced workload for hospital antenatal clinics.
To date, there has been limited research regarding the effectiveness of ANSC and women’s satisfaction with this type of care. Available research suggests that the ANSC model may result in improved obstetric outcomes4 and be as acceptable to women as the traditional care alternative.5 However, inconsistency and sometimes lack of information provided to pregnant women have been identified as disadvantages.6
The Australian Clinical Practice Guidelines for Antenatal Care outline the importance of continuity of care, and specify the provision of information about key pregnancy topics such as food safety, folic acid and iodine supplementation, physical activity and preparation for breastfeeding.2 There are no national defined pathways for ANSC, but different states and health districts have developed their own guidelines, which vary in terms of recommendations for what advice should be provided to women, at which time points and by whom. For example, the defined clinical pathway for ANSC in the Illawarra region, a GP-led model, suggests that breastfeeding advice should be provided by GPs in weeks 16–24, whereas advice on nutrition supplementation should be provided at the first ANSC visit, before 12 weeks gestation.3 Compliance with these guidelines, however, is yet to be investigated.
Although there is limited research related to the nutritional advice that pregnant women receive and how this advice is used,7 some studies have shown that pregnant women may be more likely to take pregnancy supplements if verbally recommended to do so by their healthcare provider, and if they have received ongoing counselling regarding supplement use.7 In adults with chronic lifestyle-related diseases, evidence suggests that advice from GPs is effective in improving nutrition-related behaviour.8
The aim of this study is to assess the satisfaction of pregnant women with the ANSC program and their perceived adequacy of the advice they received about nutrition-related issues and other important topics for pregnancy.
Methods
As part of a larger study that assessed the nutrition-related knowledge and practices, including supplement use, of pregnant women and healthcare providers who participate in the GP-led ANSC in the Illawarra region of NSW,9 enrolled women also completed questions related to their satisfaction of the service. The self-completed satisfaction survey comprised items related to1 relevant topics discussed with their GP, such as diet, physical activity, and breastfeeding;2 satisfaction with explanation of tests;3 and satisfaction with waiting times and the general service provided (Table 1).
Table 1. Satisfaction questions
|
- Have you previously participated in Shared Care during pregnancy? (Closed question; Answers: Yes; No; Do not know)
- Were you happy with the number of visits you had with your GP during this pregnancy? (Closed question; Answers: Yes; No – I would have preferred more visits; No – I would have preferred fewer visits)
- (A) Were you satisfied with the amount of information you received regarding your pregnancy from the Antenatal Shared Care Program? (Closed question; Answers: Yes; No)
(B) If no, please describe the further information you would have liked to receive (Open question)
- Were you provided with enough time to discuss any questions you had regarding your pregnancy during visits with your GP? (Closed question; Answers: Yes – on every visit; Yes – on most visits; Yes – on some visits; No)
- Were the tests conducted during your pregnancy clearly explained to you by your GP? (Closed question; Answers: Always; Sometimes; Rarely; Never)
- Which of the following did you discuss on at least one of your visits with your GP during your pregnancy? (Closed question; Topics: Diet; Exercise; Physical changes to you during pregnancy; Emotional changes to you during pregnancy; Infant feeding. Answers: Yes; No; Do not know)
- When visiting the hospital clinics were you happy with the waiting time? (Closed question; Answers: Always, Usually; Sometimes; Never)
- (A) When visiting the hospital clinics were you happy with the service provided? (Closed question; Answers: Always; Usually; Sometimes; Never)
(B) If you answered ‘Usually’, ‘Sometimes’ or ‘Never’, which aspects of the service were you unsatisfied with? (Open question)
- The following statements ask how you felt about various aspects of the Antenatal Shared Care Program. (Closed question; Statements: ‘I felt confident in my Doctor’; ‘I felt anxious about participating in the Shared Care Program’; ‘I felt involved in my Antenatal Shared Care for this pregnancy’; ‘Talking to my doctor about problems was easy’; ‘I felt in control of my pregnancy’; ‘I understood what was happening in this pregnancy’; ‘When I asked my GP about specific information about my pregnancy it was always provided’; ‘I was always able to obtain the advice I needed from my GP’. Answers: Strongly agree; Agree; Disagree; Strongly Disagree; Don’t know)
- Do you believe that you have received enough dietary information to make informed decisions concerning the following topics during this pregnancy? (Closed question; Topics: Iron; Iodine; Calcium; Healthy eating; Folate; Listeria and/or food poisoning; Use of dietary supplements during pregnancy. Answers: Yes; No; Do not know)
- How did you receive this information? (Closed question; Topics as above. Answers: Written information from health professionals; Verbal information from health professionals; Newspaper; Magazine; Television; Radio; Internet; Did not receive any information; Do not know)
- Do you have any other comments related to your experience with the Antenatal Shared Care program? (Open question)
|
The satisfaction questions were developed in conjunction with midwives and managers of ANSC, and were designed to provide a process for evaluation of the service against clinical guidelines, as well as more detailed constructive feedback for future improvement of the service.
Data collection was carried out in two recruitment phases. First, all women enrolled in ANSC as of 28 December 2012 (n = 515) were sent two mailed flyers requesting their participation in an online survey using the Survey Monkey website, to which 37 responded (7% response rate). Given the low response rate, a second recruitment phase was undertaken during the month of August 2013, whereby women enrolled in ANSC were approached directly while waiting for their routine obstetrician appointments at the major public antenatal clinic in the catchment area. A total of 152 women enrolled in ANSC were booked for obstetric appointments in August 2013, but not all women were invited to participate as some may have attended obstetric appointments at the second, smaller public antenatal clinic in the Illawarra catchment area. Enrolled women were identified through their antenatal file and those who consented completed a self-administered, paper-based version of the questionnaire (n = 105).
Data were analysed using SPSS 19.0 (SPSS Inc Chicago, IL, USA) using descriptive statistics. For results on the discussion of infant feeding, only women at >24 weeks gestation and women who had already given birth were included, as the guidelines recommend this discussion occurs between 16 and 24 weeks gestation. Ethical approval to conduct the study was obtained from the Human Research Ethics Committee of the University of Wollongong and site-specific permission was obtained from NSW Health (HREC11/254).
Results
A total of 142 women consented to participate; however, two women were excluded from analyses secondary to incomplete surveys. Demographics of participants are presented in Table 2.
Table 2. Socio-demographic characteristics of women including gestational age and intention to breastfeed
|
|
Age
|
|---|
|
Mean SD (years)
|
29 ± 5.1
|
|
Range (years)
|
18–46
|
|
Education
|
n (%)
|
|
Completed post-school education
|
87 (62%)
|
|
Trimester
|
|
|
1 (0–12 weeks)
|
17 (12%)
|
|
2 (13–24 weeks)
|
20 (14%)
|
|
3 (>25 weeks)
|
103 (74%)
|
|
Already given birth
|
17 (12%)
|
|
First pregnancy/birth
|
66 (47%)
|
|
Intend to breastfeed (n = 124)
|
126 (90%)
|
|
Currently breastfeeding (n = 17)
|
14 (82%)
|
|
Previous miscarriage
|
26 (19%)
|
|
Multiparous women (n = 74) who had previously participated in ANSC
|
55 (72%)
|
|
Total n = 140
|
|
Satisfaction with ANSC services
Overall, women expressed a high satisfaction with the antenatal services provided by their GP. The majority (93%) of women were happy with the number of visits they had had with their GP. Most women ‘strongly agreed’ or ‘agreed’ when asked how they felt about positive statements on ANSC services on a 5-item Likert scale (Table 3).
Table 3. Percentage of women who ‘strongly agreed’ or ‘agreed’ with statements regarding ANSC services on a 5-item Likert scale
|
|
Statement about ANSC
|
‘Strongly agreed’ or ‘Agreed’
|
|---|
|
I felt confident with my doctor
|
93%
|
|
I felt involved in my antenatal shared care this pregnancy
|
83%
|
|
Talking to my doctor about problems was easy
|
87%
|
|
I felt in control of my pregnancy
|
86%
|
|
I understood what was happening in this pregnancy
|
91%
|
|
When I asked my GP about specific information about my pregnancy it was always provided
|
96%
|
When asked about their experiences at visits to the public hospital antenatal clinic, over half (59%) of the participants reported being ‘sometimes’ or ‘never’ satisfied with the waiting time; however, most (80%) were ‘always’ or ‘usually’ happy with the services provided. The most commonly reported reasons for dissatisfaction (open-ended question) were:
- long waiting times (n = 20)
- unfriendly and rushed staff (n = 16)
- staff not answering questions or providing explanations (n = 8)
- inconsistent information and lack of continuity of care (n = 6).
One woman commented, ‘I found that there was little continuity of care, and differing opinions and advice every time I came. There was no liaising with my GP’.
Satisfaction with amount of information received
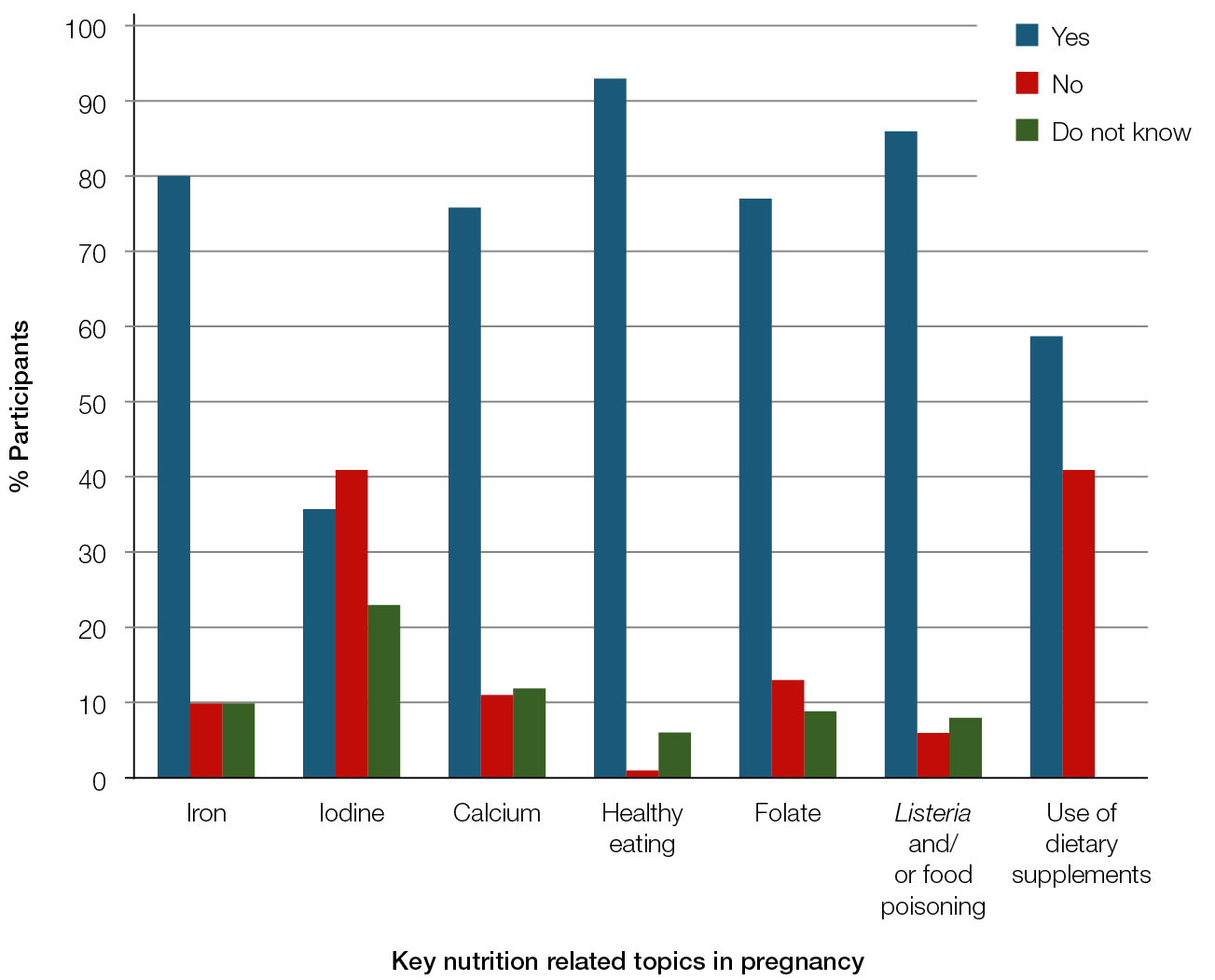 |
| Figure 1. Participants’ perception of whether they received adequate dietary information to make informed decisions about key nutrition related topics in pregnancy |
Most women (84%) were satisfied with the amount of information they had received from the ANSC program regarding their pregnancy. Women reported wanting more information about a variety of topics, including the process of ANSC, ‘More information about dealing with the antenatal clinic, and expectations regarding appointments with antenatal clinic staff’.
Most women (96%) reported that they had enough time to discuss questions with their GP on all or most visits, and 81% reported that tests were always explained by their GP. Women were asked whether their GP had discussed specific pregnancy-related topics (Table 4). Women were also asked whether they received enough dietary information to make informed decisions about key nutrient topics in pregnancy (Figure 1). Most women reported receiving either written or verbal advice from a healthcare professional about iron (79%), calcium (66%), healthy eating (81%), folate (74%), Listeria infection and/or food poisoning (80%) and use of dietary supplements (71%). Less than half (46%) reported receiving information about iodine.
Table 4. Proportion of participants who reported that they discussed specificpregnancy related topics with their GP (closed question: yes; no; do not know)
|
|
Topic
|
Percentage of participants who reported discussing with GP
|
|---|
|
Diet
|
79%
|
|
Exercise
|
66%
|
|
Physical changes
|
75%
|
|
Emotional Changes
|
62%
|
|
Infant Feeding (n=122)‡
|
30%
|
|
‡Women at 24 weeks gestation or above and women who had already given birth
|
Discussion
Overall, the women seemed to be highly satisfied with ANSC, with the exception of long waiting periods experienced when attending the public antenatal clinic. Most multiparous women (72%) had previously participated in ANSC and their re-attendance was likely to indicate their satisfaction with the model. This research reinforces the importance of providing women with realistic expectations of the service. One woman commented, ‘I was advised to bring a book because the wait was often long. I came prepared and had taken the day off work in case the wait and/or appointment were longer than expected. In that respect I wasn’t inconvenienced and didn’t feel frustrated’.
The majority of women were satisfied with the amount of information they had received from their GP; however, it seemed that infant feeding and iodine supplementation were not being adequately discussed. Lack of verbal guidance on breastfeeding is particularly concerning, as some limited research has suggested that the discussion of breastfeeding with healthcare professionals increases the initiation and duration of breastfeeding.10 Although breastfeeding initiation rates are relatively high in Australia, only 14% of infants are exclusively breastfed to 6 months,11 in line with World Health Organization recommendations.12 Qualitative research has highlighted that healthcare professionals lack confidence in discussing breastfeeding,13 and a recent survey has found that most GPs do not discuss breastfeeding with expectant mothers during antenatal consultations.14 There is currently no consistent approach to educating healthcare providers, including GPs, on breastfeeding in Australia.15 Encouragingly, however, an objective of the Australian National Breastfeeding Strategy (2010–2015) is to ensure that health professionals are appropriately trained to provide breastfeeding support and advice.16
There is a clear lack of information being provided to pregnant women about iodine requirements, compared with other key nutrition topics, which has been demonstrated previously.17 Just under half (41%) of the women reported that they had not received enough information to make an informed decision about the use of dietary supplements. Research has highlighted suboptimal rates of iodine supplementation in pregnant women,9,17–19 which is concerning as even mild iodine deficiency during pregnancy can result in reduced cognitive outcomes in childhood.20 Following a survey conducted by the research group in 2008,21 the public antenatal clinic included in this study changed its practice to provide a written information sheet, specifically focusing on iodine, to all pregnant patients. Despite this change in clinical practice, only 46% of participants reported having received written or verbal information about iodine. It is possible that women may have received but not read the handout and some research suggests that health information provided in the written format has little impact if not also discussed verbally.22 Barriers to providing nutritional advice to pregnant women identified by healthcare professionals include inadequate time, lack of training and insufficient educational resources.7
The main limitations of the study are the use of a non-representative, convenient sample and potential bias introduced by recruitment of volunteers who may have been more interested in health than the general population of pregnant women. As participants were recruited while waiting in the public antenatal clinic, responses may have been further biased in a positive direction because of the dissatisfaction with waiting times at the clinic. The poor response rate for the initial recruitment phase is an additional limitation. However, it is noted that the response rate for the second recruitment phase is likely to be higher than 69% secondary to being unable to invite all women enrolled to participate despite best efforts. Non-English-speaking women were also excluded from the study. In 2013, 26 women who participated in ANSC required an interpreter.
Implications for general practice
Ensuring a high level of ongoing communication between the antenatal clinic and general practice staff participating in ANSC, including establishing realistic expectations and delivering consistent nutrition and health messages, is essential to providing a high-quality service. Exploration of antenatal care providers’ compliance with information delivery and the method of delivery are warranted, as is further research into how women use health and nutrition information.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.