Marine envenoming can be considered in two broad categories: jellyfish stings and penetrating venomous marine injuries. Jellyfish stings range from the life-threatening major box jellyfish (Chironex fleckeri) to painful, but generally benign, bluebottle stings common to most southeastern Australian beaches (Figure 1). Penetrating venomous marine injuries often occur when handling fish, but can occur to anyone involved in water activities, fresh water or marine. They are typically more painful than just the trauma of the wound, and injury severity is related to the anatomical location. Deaths, although rare, have occurred from penetrating thoracoabdominal injuries from stingrays.
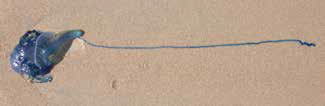 |
Figure 1. Blue bottle (Physalia spp.) from eastern Australia
Photo by Geoffrey Isbister |
Jellyfish stings
Jellyfish cause stings when their tentacles contact skin. Contact triggers the jellyfish to release venom from millions of tiny stinging cells (nematocytes) covering the tentacles. The venom is released via a harpoon-like mechanism that injects venom into the dermis.
Sting severity is related to:
- the number of stinging cells that fire, which depends on the amount of tentacle contact with skin
- the potency of injected venom, which depends on the species.
The most dangerous jellyfish, the major box jellyfish (C. fleckeri), has a highly potent venom as well as multiple long tentacles. Deaths from the major box jellyfish have occurred in Northern Australia, but remain rare. Bluebottles (Physalia species) are the most common cause of jellyfish stings worldwide and in Australia, although few people present to hospital. Stings occur at times when swarms of bluebottles are in shallow coastal waters or along the shoreline. Irukandji-like stings occur in Northern Australia, most commonly due to Carukia barnesi, but cases have occurred less commonly in other parts of Australia and from other jellyfish types.
Clinical manifestations
Patients stung by jellyfish present in one of two ways:
- the majority present with an immediately painful, linear/tentacle-like sting
- a minority present with delayed pain – Irukandji-like sting (Table 1).
Linear/tentacle stings usually result in local pain where the tentacles contact skin. There is a raised erythematous or urticarial lesion that is distinctive and can last hours to days (Figure 2A, B). Typically, the pain resolves within 1–2 hours. Mild systemic symptoms such as nausea, vomiting and malaise occur uncommonly. Rarely, there may be delayed reactions such as papular urticarial rashes along the sting sites
(C. fleckeri), bullous lesions or keloid scarring (usually in predisposed individuals). Although the presentation of most C. fleckeri stings is similar to other stings, severe envenoming resulting in cardiovascular collapse and death can occur. These cases are characterised by significant hypotension within 20–30 minutes, which leads to death without basic life support.

A |

B |
Figure 2.
A. Bluebottle sting on the back of a child 2 days after the sting;
B. Multiple linear stings following a major box jellyfish (C. fleckeri) sting
Photos by Geoffrey Isbister |
Irukandji-like stings can often initially go unnoticed in divers in deep water. Within 20–30 minutes they develop severe, excruciating generalised pain (abdominal, back and chest pain). There is rarely local pain and often there is only a minimal skin reaction. The patient is often distressed and may have associated agitation, nausea, vomiting and diaphoresis. Patients can develop tachycardia and hypertension, which may result in myocardial injury and pulmonary oedema. Animal studies have shown that C. barnesi envenoming is associated with the release of endogenous catecholamines, consistent with a sympathomimetic toxidrome.1 Electrocardiogram (ECG) ST segment and T wave changes, and elevated troponins due to myocardial injury can occur.
Table 1. Summary of the clinical effects, first aid and treatment of the most common medically important jellyfish
|
|
Jellyfish stings
|
|---|
|
Linear/tentacle-like stings
|
Irukandji-like stings
|
|---|
|
Bluebottle and minor jellyfish
(Physalia spp, Pelagia, Cyanea, Aurelia, some Carybdidae)
|
Major box jellyfish
(Chironex fleckeri)
|
Other box jellyfish
(Carukia barnesi, etc)
|
|
Clinical effects
|
|---|
|
Typically, these stings cause immediate local intense pain for 1–2 hours, and associated linear erythematous eruptions
|
These stings cause severe local pain and associated erythematous eruptions along the lines of tentacle contact. In large surface area contact exposures cardiovascular collapse and death can occur
|
Irukandji syndrome is typically delayed (20–30 mins) with generalised severe pain and systemic effects (tachycardia, agitation, hypertension) and in a small proportion cardiac injury/pulmonary oedema
|
|
First aid
|
|---|
- Wash sting site with seawater and remove tentacles
- Hot water immersion (45°C for 20 minutes*)
- Avoid vinegar as it may worsen the pain
|
- Apply vinegar and remove tentacles
- Commence immediate cardiopulmonary resuscitation on any patient who is unconscious
|
- Apply vinegar and remove any remaining tentacles
|
|
Further medical management
|
|---|
|
Generally no further intervention is necessary
|
Transport to hospital for:
- Analgesia (oral and IV)
- Consider antivenom in patients with cardiovascular collapse not responsive to standard advanced life support
|
Transport to hospital for:
- Analgesia (oral and intravenous)
- Investigation and treatment of cardiac effects (troponin, ECHO)
- Cardiac monitoring
|
|
*Evidence only for bluebottle stings but likely to work with other minor jellyfish stings2
|
|---|
Treatment
Linear/tentacle stings
In all cases the tentacles should be carefully removed, either by washing with seawater, or by hand. For bluebottles, the sting site should be immersed in hot water for 20 minutes. This treatment is supported by an open-labelled randomised controlled trial that showed hot water immersion (45°C) for 20 minutes was effective, compared with ice packs.2 Immersion should be limited to 20 minutes and the water should be tested to prevent burns. For other minor jellyfish stings, hot water can be used but there is less evidence to support this.
C. fleckeri stings can be life-threatening so early resuscitation may be required. Recommended first aid is the liberal application of vinegar after tentacles are removed to potentially prevent further discharge of venom from nematocysts. The aim is to prevent life-threatening envenoming. Vinegar is not a treatment for pain, which should be treated with ice packs, oral analgesia and titrated intravenous opioid analgesia, as required. The role of hot water immersion in C. fleckeri stings remains unclear. Patients with severe systemic envenoming and cardiac arrest should be treated according to standard advanced cardiac life support protocols, including initiation of cardiopulmonary resuscitation (CPR) at the scene. Antivenom is available and intravenous administration should be considered in severe cases where cardiac collapse occurs, although immediate CPR is by far the most critical life-saving intervention.3
Irukandji-like stings
Patients presenting with Irukandji-like stings often require hospital admission for large doses of titrated opioid analgesia. Additional treatment with antiemetics and benzodiazepines may provide symptomatic relief. Hypertension will almost always resolve with good analgesia and benzodiazepines. Patients should have cardiac monitoring, including careful evaluation for hypertensive emergencies such as myocardial injury, pulmonary oedema and intracranial haemorrhage. All patients should have an ECG and troponin, and if these are abnormal then an echocardiogram should be obtained.
Penetrating venomous marine injury
Venomous fish and stingrays all have sheath-covered venomous spines in their dorsum, ventral surface or tail. These spines can penetrate human tissue. As the spine penetrates, the venom between the sheath and spine is injected into the wound. The venom seems to contribute to the severity of the pain, typically out of proportion with the extent of the wound. Penetrating venomous marine wounds can present with delayed healing and secondary infection, again worsened by the dermonecrotic effects of the venom (Table 2). Larger penetrating injuries, usually from stingrays, and thoracoabdominal penetrations in particular, can lead to major and life-threatening trauma and should be treated as such. For this reason spines should not be removed before admission to hospital.
Table 2. Penetrating venomous marine injuries
|
|
Venomous fish
|
Stingray
|
Sea urchin
|
Sponges
|
|---|
|
Clinical effects
|
|---|
|
Typically present as puncture wounds with localised pain. The pain is dependent on how much venom is injected
|
Injury more trauma than venom-induced. Local bleeding with swelling and oedema. Rare cases develop necrosis with secondary infection
|
Pain generally not severe but multiple retained spines
|
Local pain, itchiness, paraesthesia and numbness
Gradually occur over hours and can last for days
|
|
First aid
|
|---|
|
Wash the wound site
Immerse in hot (45°C) water for up to 90 minutes
|
Wash out wound
|
|
Further medical management
|
|---|
|
Due to the risk of a retained foreign body the wound(s) needs irrigation and debridement
Consider local or regional analgesia to assist debridement
XR/US to exclude retained spine
Consider surgical referral for deep or truncal wounds, wounds involving joints/bones or retained spines
|
Simple analgesia
|
|
Stonefish antivenom is available if simple measures do not control pain
|
Truncal injuries can cause severe haemorrhage requiring urgent resuscitation and theatre as a major trauma
|
These wounds may require regular follow up and review to ensure all retained spines are removed and to prevent infection
|
|
|
Although uncommon, observe for secondary infection for at least a week
Typical organisms are Vibrio spp. in marine injuries and Aeromonas spp. in freshwater
Commence antibiotics if any evidence of infection (once swabbed)
|
Clinical manifestations
The site of injury is typically related to the type of encounter with venomous fish or stingrays. Stonefish and bullrout tend to cause injuries when trodden on (foot wounds), whereas catfish tend to sting fingers (Figure 3) and hands when handled. These wounds are typically very painful, with minimal bleeding, but can develop swelling and oedema. Stingrays are most often trodden on, causing an injury to the ankle as the tail spine whips around behind the leg (Figure 4). Serious trauma and death can occur when the spine enters major body cavities, which can occur during diving.
 |
Figure 3. Catfish sting at the base of the index finger
Photo by Geoffrey Isbister |
 |
Figure 4. Sting ray injury to the back of the ankle
Photo by Geoffrey Isbister |
Treatment
First aid for venomous fish stings and stingray injuries is hot water immersion (45°C) for up to 90 minutes. This provides symptomatic relief while the limb is immersed, but pain often returns once removed. There is little evidence except experience and case reports to support hot water immersion. It is important to check the water temperature with an unaffected limb to prevent burns and it should not be used for more than 90 minutes. If hot water immersion and oral analgesia are not sufficient then titrated intravenous opioids should be administered while arranging local anaesthesia at the wound site or regional nerve block. These will also assist exploration and cleaning of the wound, but should not be used with hot water. All penetrating marine injuries require irrigation and cleaning. Larger wounds, those involving joints or containing debris, require surgical review, exploration and debridement.
Secondary infection is the most important complication of penetrating marine injuries and is more likely to occur with unclean and larger wounds. Other complications are related to the site of the injury (eg thoracoabdominal trauma). The use of prophylactic antibiotics is controversial but is suggested for high-risk wounds. It is more important for the wounds to be irrigated and cleaned, and patients to be reviewed every 1–2 days for the first week after discharge home.
Sea urchins
Sea urchins cause injury when they are trodden on or picked up. Sea urchins cause a penetrating marine injury but rarely cause severe pain. The major problem is multiple retained spines within the injury site, which can cause persistent pain. Removal of the spines, especially if deep, can be particularly problematic, and may require referral for surgical management. Imaging of the wound site with X-ray and/or ultrasonography is essential to locate any embedded spines and those close to the surface should be removed.
Sponges
Sponge-related injuries are rare. Patients may present with local pain or a tingling sensation that develops over hours, paraesthesia and/or itch. In most cases symptoms persist for hours to 1 day. Patients injured by fire sponges (Tedania spp.) can represent with erythema, swelling and, sometimes, desquamation 2 weeks after the contact. First aid includes ensuring the wound site is cleaned, simple analgesia and antihistamines. There is no specific treatment.
Blue-ringed octopus
The blue-ringed octopus has tetrodotoxin in its saliva, which is injected when it bites. In the majority of cases, the bite causes local pain, but severe envenoming is similar to puffer fish poisoning, which causes rapid-onset generalised paralysis requiring mechanical ventilation. Most bites occur when the octopus is unwittingly picked up. First aid is a pressure bandage with immobilisation and, if necessary, CPR.
Conclusion
Most marine envenomations are treated with simple first aid so patients rarely seek medical assistance. Knowledge of the effective use of hot-water immersion, appropriate use of vinegar and identification of patients who require further referral to hospital or follow-up is vital for GPs, particularly in coastal regions. Further expert toxicology advice can be obtained from the Australian Poisons Information Centre on 13 11 26.
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.