Normal sleep
Sleep that is of sufficient quality is essential for children’s growth, development, learning and wellbeing.1 Before understanding what constitutes a ‘problem’, we first need to understand what constitutes normal sleep.
Like adults, children cycle through rapid eye movement (REM; light sleep) and non-REM sleep (deep sleep) throughout the night. Children have proportionally more REM sleep than adults, so are often reported as ‘restless’ sleepers by their parents. Children use particular cues to fall asleep. These cues can be parent-independent (eg use of a transitional object such as a teddy bear) or parent-dependent (eg when a parent rocks or feeds their baby to sleep or lies next to their child in order for them to fall asleep).
Once asleep, children tend to be in deeper sleep for the first few hours of the night, before coming into REM sleep, waking briefly, then returning to non-REM sleep. This pattern is repeated in cycles throughout the night, with each cycle lasting around 40 minutes in infants,2 increasing to 90 minutes in adults. Figure 1 is a simple schematic of sleep cycles that can be used to explain sleep cycles to parents.
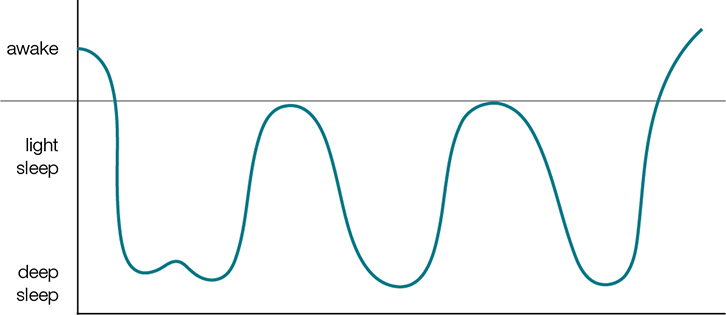 |
| Figure 1. Simplified schematic of sleep cycles |
The ideal sleep duration for children is disputed, and it may be that the timing of going to sleep and rising, and sleep fragmentation, have more impact on health and behaviour outcomes than the duration of the sleep per se. Figure 2 shows the wide variation in sleep duration in Australian children.3 If a child is having less sleep than the average but appears to be happy and healthy, they may be getting enough sleep for them.
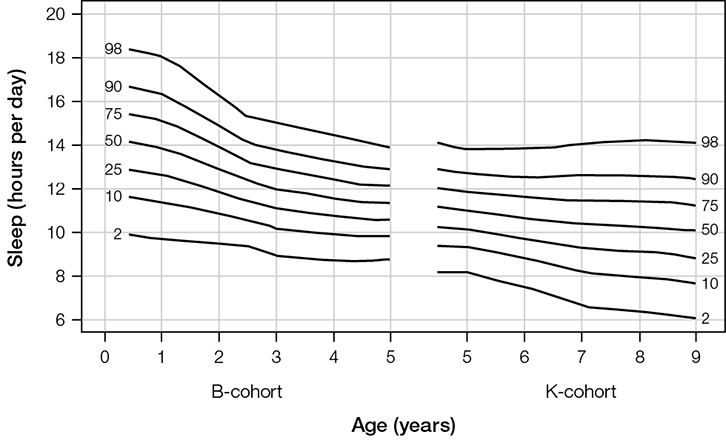 |
| Figure 2. Centiles for total sleep duration per 24 h by age in two Australian cohorts |
Common sleep problems
Sleep problems can be medical (eg obstructive sleep apnoea, night waking due to ear infections) or behavioural in origin, the latter being the most common in children.4
Behavioural sleep problems include difficulties falling asleep at the start of the night, frequent night waking, early morning waking or a combination of these. The way a child falls asleep at the start of the night is the way they expect to go back to sleep when they naturally wake up overnight. Thus, if the last thing a child remembers is being rocked or fed to sleep, they will want to be rocked or fed back to sleep when they wake naturally overnight. This ‘sleep association’ forms the basis of a very common sleep problem in children – behavioural insomnia of childhood, sleep-onset-association type.5
Other common problems include:5
- behavioural insomnia of childhood, limit-setting type – parents have problems setting limits around bedtime and the child repeatedly comes out of their room or protests
- delayed sleep phase – the child goes to bed late and sleeps in during the morning unless woken by their parents
- anxiety-related insomnia – the child takes 30 minutes or more to fall asleep, worrying about something as they do so
- physiological insomnia – the child takes 30 minutes or more to fall asleep but is not worried or coming in and out of their room.
Obstructive sleep apnoea (OSA) can also affect infants and children, particularly preschoolers, when the tonsillar and adenoid tissue is relatively large, compared with the airway. OSA presents as persistent snoring with a period of apnoea followed by gasping, and may be associated with daytime tiredness, mouth breathing and behavioural difficulties.6
Taking a history
A detailed sleep history is essential to determine the most appropriate interventions. A 24-hour sleep history, starting from dinner time, is a useful approach (Box 1).
Box 1. Key sleep history points
|
|
Pre-bedtime
Is a routine present or not, and if so, what is it (eg bath at 6.00 pm, dinner at 6.30 pm etc)?
Is the child exposed to electronic screens, especially before bedtime?
Bedtime
Are particular circumstances or objects required to fall asleep (eg parent or TV)?
Sleeping environment (ie is the room dark, quiet and not too cold or hot?)
Time of lights out and time of sleep onset
Child’s behaviour until sleep onset
Night-time behaviour
Timing and frequency of wakings
Behaviours associated with wakings
Carer’s response: Which strategies have they tried and are they consistent?
Signs of obstructive sleep apnoea
Morning awakening
Timing: Is this consistent?
Does the child seem refreshed?
Daytime behaviour
Sleepiness or hyperactivity
Timing and duration of naps
Difficulty falling asleep during the day
General concerns
Duration of problem
Does the sleep routine/disturbance differ on weekends or holidays?
Who is concerned (child, family or school)
Pharmacological causes of sleep disturbance (eg caffeine-containing beverages or stimulating medications)
Are chronic medical conditions optimally controlled (eg eczema or asthma)?
How are the parents coping?
|
Management of behavioural sleep problems
First, ensure a consistent bedtime routine and good sleep hygiene. The latter includes:
- setting a regular bedtime
- keeping the bedroom dark and quiet
- avoiding caffeine-containing foods and drinks after 3.00 pm
- ensuring a regular morning wake time.
Limiting screen time is also important as light, especially blue light emitted from LED-lit devices (eg smartphones, electronic tablets, computer and television screens), can suppress endogenous melatonin and hinder sleep onset and quality.7,8 In the setting of a typical sleep–wake schedule, endogenous melatonin levels tend to rise two hours prior to sleep onset.9 As such, guidelines often recommend limiting exposure to screens for at least one hour before bedtime.10,11
After ensuring good sleep hygiene, parents can choose from a number of evidence-based behaviour management techniques that aim to teach children to fall asleep without parental help. These techniques are suitable for children older than six months, as younger infants may still be establishing a mature sleep–wake rhythm and require night feeds.2 Techniques should be used at the start of the night and overnight to ensure consistency. It is preferable if the parents have no important commitments for the first few days after starting any intervention. Parents can reward older children (eg with praise, stickers or stamps) if they comply with the techniques.
Behavioural insomnia, sleep-association type
Effective treatment requires substitution of parent-dependent associations with new habits or circumstances that are parent-independent.5 This could include a transitional object (eg a comforting blanket) that can remain with the child overnight. Infants older than eight months who depend on a dummy to fall asleep can be taught to replace it themselves by securing the dummy to their night attire with a short chain.
ln term, healthy infants older than six months, night time feeding is likely to represent a learned behaviour leading to more feeding during the night time than the day time. If this is disruptive, parents can gradually wean the volume (if bottle-fed) or duration (if breastfed) of feeding over 7–10 nights. If a child is used to falling asleep at the start of the night while feeding, then the last feed should be given outside the bedroom, at least 20 minutes before bedtime, in order for the sleep–feed association to be broken.
To encourage the child to settle independently, parents can choose between two management strategies: ‘controlled comforting’ (graduated extinction) and ‘camping out’ (adult fading).
Controlled comforting
‘Controlled comforting’ involves the parents settling the child in the cot or bed by patting or stroking them until they are quiet but not asleep, and then leaving the room.5 The parents respond to crying by checking on the child at set intervals and comforting them in the cot or bed as needed. Checking intervals are gradually increased. For example, start at two minutes, then increasing in two-minute increments. If the child is still crying after each interval, the parents return, settle them, then leave. The process is continued until the child falls asleep without intervention. The effects are typically achieved within about one week, but may take a little longer.5
Camping out
‘Camping out’ involves the parents placing a chair or camp bed next to their child’s cot or bed; initially the parents stay with them as they fall asleep at the start of the night, then gradually withdraw their presence from the child’s room over one to three weeks.5 Children might protest less with this method compared with controlled comforting. For the first few nights, the parents pat their child to sleep. When the child is settling with being patted, the parents spend the next few nights by the cot but not touching the child. When the child becomes used to this (usually after three nights), the parents move the chair or bed a foot away and stay until the child falls asleep. After this point, the bed or chair is gradually moved to the doorway and out of the room.5
Do behavioural strategies cause harm?
While the above strategies are associated with infant crying, follow-up of more than 400 children from randomised controlled trials of controlled comforting and camping out found reduced symptoms of maternal depression two years post-intervention, and no impact on child behaviour, parent–child relationships or parenting style two and five years on.12–14 To encourage adherence, clinicians should discuss parents’ concerns about potential strategies and explore ‘best fit’ strategies for the family.
Behavioural insomnia, limit-setting type
Bedtime bargaining and battles often emerge as children gain language and mobility. The child’s repetitive stalling, calling out and getting up can lead to a consistent delay in sleep onset, and household disruption. For these behaviours to subside, parents must consistently enforce a predictable bedtime and clear limits, usually for days to weeks.5 Improvement is often preceded by a transient worsening of the unwanted behaviours, making the initial couple of days of treatment most challenging. Before embarking on management, it is advisable for parents to set clear expectations for night-time behaviour (‘You need to stay in your bed overnight’) and do a quick check for needs (eg toilet or drink) prior to lights out. Parents can then choose between ‘controlled comforting’ (see above), ‘extinction’ or ‘bedtime pass’ method.
Extinction occurs when the child is placed in bed and inappropriate behaviours are systematically ignored. Parents do not respond or go into the child’s room during this period unless there is a legitimate concern such as an illness. It is important that parents do not ‘give in’, as responding when the child becomes more demanding can reinforce and worsen the behaviours. If the child gets up and comes out of the bedroom, parents can calmly and gently lead them back to or place them in bed, reminding them of the expectations with minimal interaction. Parents can erect a gate to keep their child in the bedroom.
The bedtime pass method is suitable for children three years and older. The child gets a ‘pass out’ at bedtime for one acceptable request (eg a drink or a kiss). Once the pass is used, parents do not respond to further requests.15
Anxiety-related insomnia
Anxiety is a common cause of difficulties falling asleep. It may present as a sleep-onset association disorder, requiring a parent to be present for the child to fall asleep. In addition to the strategies for sleep-onset association disorder outlined above, older children can try to reduce their anxiety by writing or drawing their worries in a book and then closing the book on their worries for the night, and/or using visual imagery and relaxation techniques around sleep onset. If these simple measures are unsuccessful, consider referring the child to a child psychologist.
Adolescents: Delayed sleep onset
Difficulty falling asleep until very late at night is particularly marked in delayed sleep phase disorder, which affects up to 7% of teenagers.16,17 If there is more than 30 minutes between bedtime and sleep onset, ‘bedtime fading’ is an effective strategy.5 This involves temporarily setting the bedtime to when the child or adolescent easily falls asleep (eg 11.00 pm). Bedtime is then moved earlier by approximately 15 minutes every few nights to the desired bedtime (eg 9.00 pm), allowing circadian rhythms to gradually re-adjust. Bedtime fading needs to be supplemented by:
- consistent early morning wake time
- elimination of daytime naps to encourage night-time sleepiness
- avoiding the use of technology with screens before bed
- increasing natural light exposure in the morning.
These measures will ideally continue on weekends and holidays. There is a limited role for pharmacological treatment (eg melatonin), which is generally only trialled if behavioural strategies and attempts at good sleep hygiene have failed. Compounding pharmacies dispense melatonin, and dosages of 3 mg and 6 mg are generally used for primary and secondary school-aged children, respectively.18 While widely prescribed by paediatricians, it should be noted that melatonin is currently not approved for use in children by the Therapeutic Goods Administration of Australia due to insufficient safety and efficacy data in paediatric populations.19
Sleep diary
Parents can complete a simple diary (see ‘Resources’) of their child’s sleep patterns during treatment. This can be reviewed at follow-up with the health practitioner to see how the child is responding to management and to aid parent recall in this often sleep-deprived time.
Extinction burst
The ‘extinction burst’ occurs when there is a burst of the unwanted behaviour some weeks after successfully extinguishing the behaviour. It is thought to affect 20–30% of children.19 Parents should be warned about this as they would otherwise think their approach has failed. Provided that the child is well, parents can reinforce the original behaviour management strategy when an extinction burst occurs. The child will usually return to their good sleep habits after two to three nights.20
Follow-up
Ideally, families will be seen by a health practitioner within two weeks of starting behaviour management. If sleep has improved, the clinician should discuss extinction burst with parents. If sleep has not improved, the clinician needs to consider why, including:
- inconsistency in applying techniques
- disagreement between parents
- parents finding the process overwhelming.
If parents are finding the process overwhelming, offer alternative strategies and consider breaking down the management into steps. For example, ensure good bedtime routine for one week, then camping out at the start of the night, then camping out when the child wakes overnight too.
Key points
- Sleep problems are common and have an impact on both children and families.
- Ask about sleep difficulties.
- Ensure good sleep hygiene and consistent bedtime routines.
- Offer evidence-based management strategies tailored to family choice and ability.
- Follow up with families and review their sleep diaries.
- Warn parents about the extinction burst.
Resources
The following resources are useful for parents and health professionals:
Authors
Katrina Hannan MBBS (Hons), Paediatric Trainee and Honorary Research Fellow, Centre for Community Child Health, The Royal Children’s Hospital, Parkville, VIC; Murdoch Childrens Research Institute, Parkville, VIC. katrina.hannan@rch.org.au
Harriet Hiscock MBBS, FRACP, MD, Grad Dip Epi & Biostats, Paediatrician and Senior Research Fellow, Centre for Community Child Health, The Royal Children’s Hospital, Parkville, VIC; Murdoch Childrens Research Institute, Parkville, VIC; Department of Paediatrics, University of Melbourne, Parkville, VIC
Competing interests: None
Provenance and peer review: Commissioned, externally peer reviewed.