Dental trauma
Facial trauma that results in displaced, fractured, or lost teeth can have significant negative functional, aesthetic and psychological effects on patients. Initial management of all patients with trauma should include a primary survey at a minimum. Dental trauma is commonly caused by sporting injuries, falls, motor vehicle accidents or interpersonal violence. The practitioner should obtain relevant medical and dental history (including mechanism of injury), as this information will determine appropriate management.1
Dental anatomy
Adults generally have 32 permanent teeth, and children have up to 20 primary (deciduous) teeth. The first childhood tooth to erupt is the central incisor at about 8–12 months of age. Children generally have a full set of primary teeth by 30–36 months of age.2 Permanent teeth begin to erupt with the first molar at six years of age and all permanent teeth erupt by 13 years of age. The exception is the third molars, which usually erupt at 17–21 years of age, if at all.
In Australia, the Fédération Dentaire Internationale (FDI) notation is commonly used to denote a specific tooth. In permanent dentition, the teeth are numbered from the central incisor as 1, laterally to the third molar as 8, with the mouth separated into four equal quadrants divided in the midline.3 Looking at the patient, the patient’s upper right quadrant is numbered 1 and progresses clockwise to 4 in the lower right (Table 1, Figure 1).
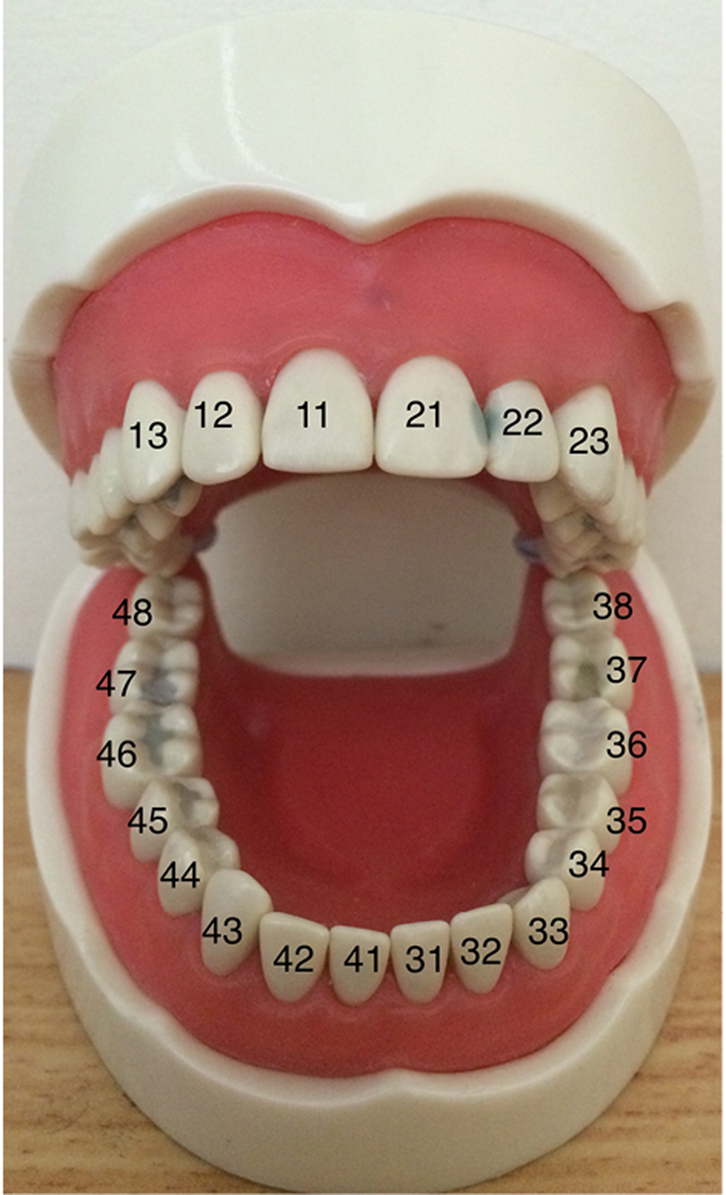 |
| Figure 1. Tooth numbering |
Table 1. Tooth numbering system used in Australia for adult/permanent dentition
|
|
18
|
17
|
16
|
15
|
14
|
13
|
12
|
11
|
21
|
22
|
23
|
24
|
25
|
26
|
27
|
28
|
|
48
|
47
|
46
|
45
|
44
|
43
|
42
|
41
|
31
|
32
|
33
|
34
|
35
|
36
|
37
|
38
|
Deciduous (primary) teeth are numbered in a similar way, where the sequence of quadrant numbers continues to 5, 6, 7 and 8, which represent the patient’s upper right, upper left, lower left and lower right, respectively. For example, when describing a particular tooth such as the permanent maxillary left central incisor, the notation would be ‘2, 1’.
The outer layer of the crown of a tooth is made up of hard, mostly inorganic and insensate enamel. The outer layer of the root is cementum, a softer mixture of inorganic and organic materials that provides attachment for the periodontal ligament to hold the tooth firmly in the alveolar bone. Underlying the enamel is the sensate dentine, which is a mineralised connective tissue substance. This supports the enamel and cementum, which separates them from the pulp chamber. The pulp chamber is the neurovascular nest of the tooth. This is where nerves and vessels enter the tooth through the roots. Covering the bone is the gingiva (gum), which acts to protect and surround the necks of erupted teeth and cover the crowns of un-erupted teeth. The periodontal ligament, cementum, alveolar bone and gingiva encircle the tooth and provide it with strength and stability. These are collectively referred to as periodontal tissues.
Assessment of the dental injury
A relevant history should be taken after the primary survey has been completed and other injuries managed. Tetanus status should be elicited and the vaccine administered if indicated. The dental history should include missing teeth, history of trauma, previous orthodontics, root canal therapy and fillings. Reported dental pain or sensitivity can guide the examination.
The practitioner should ask the patient to bite down and assess any occlusal disturbances, and enquire if these changes are new.4 An altered occlusion can be a sign of maxillofacial injuries (eg mandibular or midface fractures). This must be followed by appropriate imaging (eg orthopantomogram and computed tomograph) if indicated. The oral cavity should be examined using a light source to look for any abnormalities of the lips and intraoral structures. It is not uncommon for teeth, or fragments of teeth, to be imbedded in the lips and cheeks. Lacerations of the vestibule (eg degloving injuries) may contain gravel or dirt.5
A complete tooth-by-tooth examination should be conducted using FDI notation and the findings documented. These may be important for follow-up care, medico-legal or insurance purposes.1 Clinical photographs should also be taken for the medical record as they offer a precise documentation of the extent of the injury. These can also be used later for planning treatment, legal claims and transfer of care purposes. This must be done with the patient’s consent following relevant privacy procedures.
Classification and treatment of dental injuries
A common descriptive language to describe dental injuries is important as management often extends to several specialties. General practitioners (GPs), emergency physicians, oral and maxillofacial surgeons, and dentists may all be involved in the management of a single patient. Each member of the treating team should therefore be able to communicate the nature and extent of the dental injuries. It is also important to understand what the expected management and likely outcome of treatment would be. This ensures continuity and consistency across all aspects of the patient’s management plan.6
Andreasen developed a classification system in 1972 that encompassed primary and permanent dentition.6 A comprehensive, easy-to-use website was also created by the Rigshospitalet, Denmark and the International Association of Dental Trauma (www.dentaltraumaguide.org). The injuries are divided into the following categories, and have been summarised by the authors to make them relevant to the general practice setting.
Injuries to the dental hard tissues and pulp
Dental hard tissues include the enamel, dentine and cementum (Figure 2).
 |
| Figure 2. Enamel dentine fracture of 11 |
Fractures limited to the crown and root can be difficult to view without transilluminating light or special equipment. These may not be available to GPs. It is therefore best to assess these injuries based on the following clinical features:
- pain
- mobility of the fractured tooth segments
- the presence of infection in advanced cases.
Fractures that involve the pulp may result in red soft tissue being visible in the area of the fracture. These injuries require referral to a general dentist who will take intra-oral radiographs to visualise the fracture.
Treatment may require root canal therapy and restoration of the tooth.7 The role of the medical practitioner is to manage the patient’s pain and ensure attendance at a dental practice as early as possible.8
Injuries to periodontal tissues
Concussion
History of trauma that is tooth or area specific.
Clinical features – Pain to percussion in both horizontal and vertical directions. There may be no signs of tooth movement, which includes no bleeding, mobility or displacement.
Treatment – Refer to the general dentist as no further treatment is required from the GP. Simple analgesia may be prescribed depending on the severity of the injury.8 Advise a soft diet until review by the dental officer.
Subluxation
Abnormally mobile tooth within the socket.
Clinical features – Pain and mobility.
Treatment – Stabilise the tooth if required, then urgently refer to a general dentist (as early as possible). Apply a splint if materials are available (discussed later in the article). Simple analgesia may be prescribed depending on the severity of the injury.8 Advise a soft diet until review by the dental officer.
Intrusion
Partial or complete displacement of tooth inside the socket.
Clinical features – Pain and displacement of the tooth into the socket. It is more commonly seen in the maxilla because of the thinner bone surrounding the tooth root. The intruded tooth may injure the underlying developing tooth bud in primary dentition, causing abnormalities in tooth eruption and possible defects affecting the enamel or other vital structures of permanent teeth.9
Treatment – Urgently refer to a general dentist (as early as possible) as no further treatment is required from the GP. Simple analgesia may be prescribed depending on the severity of the injury.8 Advise a soft diet until review by the dental officer.
Extrusion
Partial tooth displacement out of the socket.
Clinical features – Pain. The tooth is displaced towards the occlusion (away from the socket) but remains within the tooth socket.
Treatment – Administer a local anaesthetic nerve block if the GP is appropriately trained, and reposition the tooth. Apply a splint if materials are available and urgently refer to a general dentist (as early as possible). Simple analgesia may be prescribed depending on the severity of the injury.8 Advise a soft diet until review by the dental officer.
Lateral luxation
Lateral movement of tooth, part of the root may be visible (Figure 3).
 |
| Figure 3. Lateral luxation |
Clinical features – Pain. This type of injury is often associated with alveolar bone fracture of the bone that surrounds the tooth root. It has been shown to be the most frequent injury affecting primary dentition.2 These can be unstable and may affect the bone at different levels depending on the nature of the injury.
Treatment – Administer a local anaesthetic nerve block if the GP is appropriately trained and reposition the tooth. Apply a splint if materials are available and urgently refer to a general dentist (as early as possible). Simple analgesia may be prescribed depending on the severity of the injury.8 Advise a soft diet until review by the dental officer.
Avulsion
Complete disarticulation of the tooth from its bone socket.
Clinical features – Pain. The tooth is completely displaced out of the socket but may occasionally still be in the mouth. There may be bleeding on presentation, and depending on the time passed, there may be a clot in the tooth socket. The most frequently avulsed tooth in the permanent dentition is the maxillary central incisor, which predominantly presents in the 7–10 years age group.10 It is essential to assess if the patient has inhaled the tooth if it appears to be missing and has not been found at the site of the accident. This requires chest imaging. The patient will need to visit a dentist to discuss possible restorative options for the space created by the missing tooth if no tooth is found.
Treatment – Success of replanting avulsed teeth depends on:
- Time since injury: less than two hours is ideal as replantation success is limited after this time.11
- Storage material: Storage of the avulsed tooth in a compatible solution will prevent the periodontal ligament from drying out and increases the possibility of successful replantation. In order of preference, the tooth should be placed in a commercial dental storage medium (Hank’s solution), contact lens saline (available at pharmacies), milk, or held inside the patient’s cheek respectively.11 This is critical and should be done upon presentation to the GP’s office or at the emergency department triage desk. The tooth should not be dried or exposed to the air, and should be gently rinsed with saline. Water should be avoided as its osmotic effect causes cell death in the periodontal ligament.
- Whether the permanent tooth has an open or closed apex: Children with immature, developing adult teeth with an open apex have a greater chance of re-establishing the blood and nerve supply to the teeth than adult teeth with closed apices.12
- Tooth type: Primary teeth should not be replanted or repositioned as this may damage the adult tooth that is developing in the bone.
It is appropriate to place the tooth in a plastic wrap and ask the patient to spit some saliva (which may contain some blood, which is desirable) into the plastic before wrapping the tooth if it is not safe for the patient to hold the avulsed tooth inside their cheek (eg risk of aspiration).
Replantation can be attempted if it does not delay presentation to a general dentist. The medical practitioner can administer a local anaesthetic nerve block if they are appropriately trained. Gently irrigate the tooth and socket before inserting the tooth. Ensure that the correct tooth is in the correct socket and it is in the correct orientation. Apply a splint if materials are available. Prescribe an appropriate antibiotic such as amoxicillin 500 mg orally every 8 hours for 7 days and chlorhexidine 0.2% mouthwash 10 ml rinsed for 1 minute every 8 hours for 14 days. Urgently refer to a general dentist (as early as possible). Immobilising teeth in their correct anatomical position as soon as possible provides the best chance of replantation and prevents further damage from occurring.14 Advise a soft diet until review by the dental officer.
Injuries to supporting bone
Clinical features – Pain. The supporting bone is visible on the avulsed tooth or in the tooth socket. Segment mobility and dislocation are also common findings.13
Treatment – Fractures involving the alveolar bone are managed with an urgent referral to a general dentist or maxillofacial surgeon (as early as possible). Fractures involving the maxilla or mandible require referral to an emergency department, or directly to an oral and maxillofacial surgeon. Advise a soft diet until review by the dental officer.
Injuries to gingival or oral mucosal areas
Clinical features – Visible breach of the oral mucosal areas with varying degrees of bleeding. The oral mucosa is well vascularised and bleeding may be brisk from a small laceration.
Treatment – Haemostasis can be achieved with digital pressure, with or without adrenaline-soaked gauze, to the injury site. The laceration will heal without further intervention if it is small and not gaping, while a larger laceration may require sutures. Referral to an emergency department, or directly to an oral and maxillofacial surgeon, is also appropriate.
Creating a dental splint
General practices and emergency departments generally have access to simple materials to fashion a splint. The simplest splints can be made with moulding blu-tack (Figure 4) or aluminium foil (Figure 5) to bridge the loose teeth. A more stable splint can be made by drying the teeth and applying a pre-moulded piece of malleable metal from a Hudson mask with skin glue.16
 |
 |
| Figure 4. Blu Tack splint in place |
Figure 5. Aluminium foil splint in place |
Conclusion
Dental trauma can occur in people of all ages. GPs are often the first to see these patients, and should be equipped with the knowledge and means to manage them appropriately.
Key points
- Patients with dental trauma may present to a GP and should be redirected to a dentist as soon as possible.
- In all instances, the sooner a dental opinion is sought, the better. If that is not possible, a panoramic radiograph (also known as an orthopantomogram) can be helpful in excluding serious pathologies such as gross caries, jaw fractures and jaw lesions such as cysts.
- Medical professionals at emergency departments and general practices should be equipped and trained to create a dental splint, if required.
- Time is of utmost importance when managing avulsed teeth. Teeth replanted within 15 minutes of the injury have the best chance of healing without complication.
Authors
Nicholas Beech MBBS, BSc, Medical Officer, Oral and Maxillofacial Surgery, Gold Coast University Hospital, Southport, QLD. nicholasbeech@gmail.com
Eileen Tan-Gore, Dental student, Oral and Maxillofacial Surgery, Gold Coast University Hospital, Southport, QLD
Karrar Bohreh MBBS, BDSc, Oral and Maxillofacial Surgery Registrar, Griffith University Dental School, Gold Coast, QLD
Dimitrios Nikolarakos MBBS, BDSc, FRACDS (OMS), FRCS, Consultant Oral and Maxillofacial Surgeon, Oral and Maxillofacial Surgery, Gold Coast University Hospital, Southport, QLD
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.