The burden of chronic illness
More than seven million Australians have a chronic disease. This costs the healthcare system more than $60 billion per year.1 The losses to the economy through reduced workforce participation and productivity are over $8 billion per year.2,3
Suboptimal management of chronically ill patients leads to serious complications and loss of quality life years. In Australia, it has been estimated that more than 500 000 hospital admissions could be avoided by more effective primary care.4 Almost two-thirds of these admissions are attributable to chronic conditions. In this context, the role of primary care providers, particularly general practice, is becoming increasingly important.
New models of care
Improving the health of people with chronic illness requires not only determining what care is needed, but spelling out roles and tasks for ensuring the patient gets care using structured, planned interactions. And it requires making follow-up a part of standard procedure so that patients are not on their own once they leave the doctors’ surgery.5
The Chronic Care Model6 is a well-established framework for chronic care management and practice improvement. There is considerable evidence showing that this model leads to more effective care and improved patient outcomes for people with chronic disease.7–9 Key elements of the model include better integrated and coordinated care, collaboration across a multidisciplinary team of care providers, planned care with regular follow-up and review, and support for patient self-management.10
However, although most practices believe they are following best practice, the evidence suggests that many are not doing so effectively.11–14 For example, in Australia, less than 20% of Medicare-rebated care plans (eg GP management plans) are regularly reviewed.15
The question is: how can a busy general practice, in which chronic conditions make up 40% of all problems managed,16 deliver such a model of care to all their chronically ill patients?
What are the barriers to optimal chronic disease management?
The biggest barriers to the delivery of this model of coordinated care include:17–19
- The complexity of communication among the care team, resulting in large amounts of faxing, scanning and telephone tag. Much of this arises from the need to get team care arrangements accepted (including those outside of Medicare requirements), as well as reporting results of treatments and interventions.
- The complexity of putting together meaningful care plans that are up-to-date, evidence-based and personalised for the patient.
- The difficulty in keeping track of what everyone on the care team is doing and ensuring that duty-of-care responsibilities are properly discharged. While the care team may report back to the GP, keeping track of who is doing what and sharing with the care team is an onerous undertaking.
- The burden of regular review and follow-up, partly because of the issues mentioned above and partly because of the difficulty of getting patients back for a visit they may perceive to be unnecessary.
- The limited means of providing support for patient self-management, given the high investment of time and resources usually required.
- The administrative overheads and red tape associated with meeting Medicare requirements and the corresponding documentation and paperwork. Associated with this is the possibility of misunderstanding the Medicare rules and failing a Medicare compliance audit.
How can digital healthcare technologies help today?
Healthcare practice supported by digital technologies (electronic processes and communications, the internet, and other information technologies) usually comes under the broad name of ‘eHealth’ or, if involving mobile devices, ‘mHealth’.
GPs have identified the following areas where they would see most benefit from these technologies:20
- Improved quality-of-care and better health outcomes (36%)
- Easier access to care for existing patients (32%)
- Reduction in administrative time, allowing greater time for patients (32%)
- More efficient processes and communication (29%)
There are many digital technologies available today that have the potential to deliver these benefits.21 We indicate below how purpose-specific digital technologies can reduce the roadblocks to best-practice care, resulting in better patient outcomes, less time on administration, more streamlined practice management, and increased practice revenues.
Simpler collaboration and communication
Shared electronic health records are an obvious solution for sharing information across the care team. However, they must be easy to use and contain the information necessary for effective clinical management. The Commonwealth’s Personally Controlled e-Health Record System (PCEHR), while an important part of Australia’s eHealth system, does not of itself provide sufficient clinical information for managing care.22
e-Referral systems can streamline conventional ‘point-to-point’ referrals. However, point-to-point referrals are not well suited to team collaboration: they position the GP at the centre of a ‘hub and spoke’ system, increasing workload and limiting communication with the rest of the care team. For team care, electronically shared progress notes, automatically posted to the entire care team, are usually a better solution.
Improved care planning
Care plan templates provided in most GP clinical systems can be used to generate text-based care plans. However, such free-text care plans are not readable by computers and therefore undercut the potential benefits of digital technologies.
More powerful care planning systems use rules to generate structured care plans (ie care plans with identified goals, targets, actions and providers that fill particular ‘slots’ in a structured plan of action). These structured care plans can be personalised to the patient, include comorbidities, and allow automated support for ongoing care management.
More effective care management
Ongoing management requires that each member of the care team knows what the rest of the care team is doing, all the time. Currently, this knowledge is almost entirely contained within the general practice (even here, relying for much of the time on patient recollection of who did what when).
Digital systems can track appointments and progress across the entire care team, compare these with the care plan, and generate an instant snapshot of what has been planned, done, and not done. Existing digital systems can also automate time-consuming collaborative processes, such as team agreements and follow-up reports, which in turn can reduce phone tag, fax follow-up, and document scanning.
More regular follow-up
Better outcomes in chronic illness care are due to proactive follow-up by the healthcare team. In real estate, they say, Location, Location, Location. In chronic illness, it is Follow-up, Follow-up, Follow-up.23
One of the most serious failings in the management of chronically ill patients is lack of follow-up and review. Even a well-organised practice can find it difficult to manage follow-up for all chronically ill patients through manual reminders. Digital technologies can help by automatically tracking the care plan and making sure every action is followed up, every time. Ensuring follow-up of health assessments is equally important, particularly for indigenous communities.24
Given that an IT system can record what has and has not been done, it can automatically generate reviews of care plan status. Moreover, by enabling reviews to be completed more efficiently, GPs and practice nurses can undertake reviews opportunistically on every patient visit rather than require a patient recall.
Support for patient self-management
There is an explosion of digital products and services for supporting patient self-management, including targeted reminders to help patients adhere to their plan, mobile applications for monitoring patient metrics, and social networks for sharing patient experiences and providing peer support.
Today, most of these systems do not connect or share information with care providers. However, some cloud-based chronic disease management services integrate with these applications. These systems have the potential to improve quality of care and revolutionise home care, allowing many patients to be cared for in a home setting instead of institutions.
Reduced red tape and administration
Chronic disease management involves considerable administrative overheads, often exacerbated by the requirements of payers such as Medicare. Existing digital products and services can help alleviate this administrative burden, automating administrative tasks, ensuring Medicare requirements are met, reducing the risk of negative compliance audits, and automating the creation and distribution of documentation.
Evidence for improved quality of care and patient outcomes
Overall, the evidence for improved quality of care and patient outcomes through the general use of digital technologies is patchy.25 The list of failures of major eHealth initiatives is also well known.26 However, this paucity of general evidence does not mean that purpose-specific digital products and services are not effective if used appropriately. Various studies indicate improved quality of care and better patient outcomes from the use of specific digital technologies27–32 and mobile applications.33,34 A recent Australian study35 shows improved quality of care, increased follow-up and review, and better patient outcomes from the use of a comprehensive chronic disease management system.
Improved financial benefits
Practices can also achieve significant financial benefits by adopting digital technologies. These benefits arise both from cost reductions (eg e-referrals, less wasted time in telephone tag and administration) and revenue increases (eg higher efficiencies, more effective use of Medicare Benefits Schedule items). The potential financial benefits need to be balanced against the cost of the technologies and justified by appropriate evidence-based business cases.
However, technologies alone will not produce these benefits. To achieve greatest benefit, practices must also consider improving their practice processes and eliminating activities that add no value either to patients or the practice.21,36
Barriers to adoption
Despite evidence that particular products and services give real benefit to GPs and other healthcare providers, adoption of digital technologies in healthcare is far slower than in most other professions.37 Evidence indicates that, although patients are strongly supportive of more digital technologies in healthcare (60% support), doctors are more conservative (23%).20
There are many reasons for poor adoption, including lack of clear evidence for improved outcomes, insufficient time to rethink practice workflows for chronic care, and the difficulty in implementing change in a busy practice environment.38
However, the rewards can be substantial. Leading corporate general practice organisations such as IPN and Healthscope, private insurers such as Medibank Private, and consumer bodies such as Movember are already investing in and using these technologies with the objectives of facilitating care coordination, delivering care more efficiently, and improving patient outcomes.
A useful resource for identifying appropriate products and services is the Royal Australian College of General Practitioners’ list of endorsed products and services for quality improvement.39
The future: a network of healthcare services
Complex systems evolve from the bottom up – from their parts.40
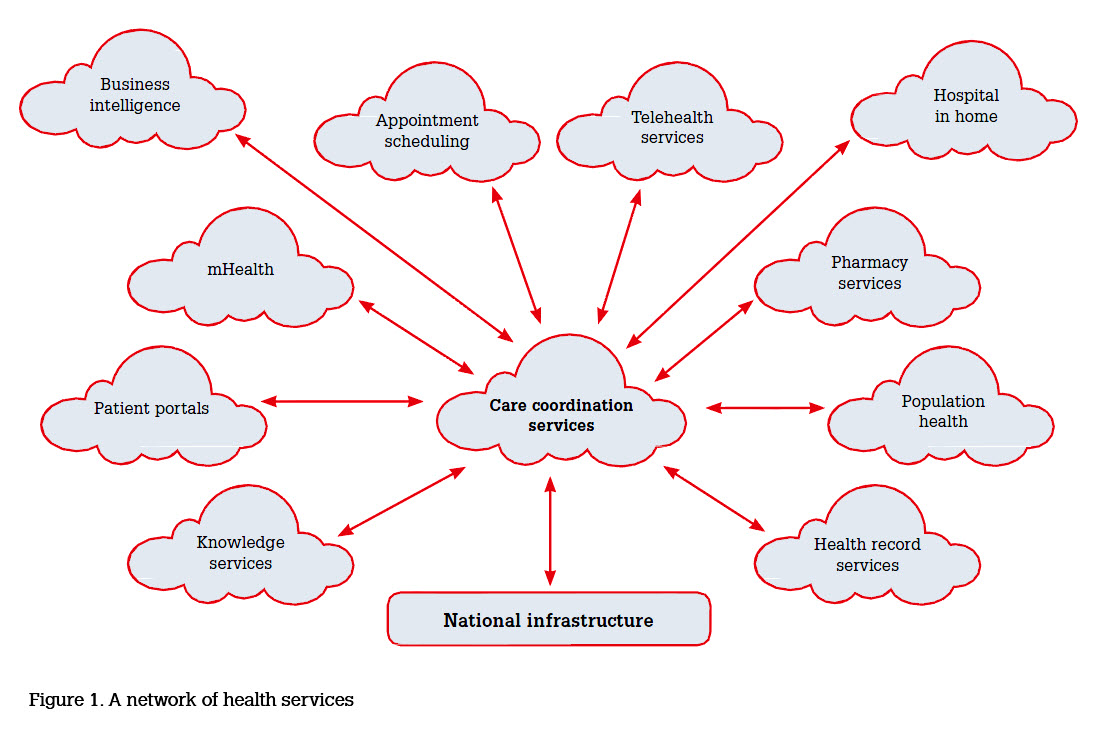
Given the complexity of healthcare, monolithic approaches to ehealth are likely to be largely replaced with more networked systems of smaller, more specialised applications and services driven by specific practical needs. The key to success is to ensure that the products and services created in this ‘bottom-up’ manner are connected in a unified network of health services, rather than ‘stand-alone’.
This vision for the future places GPs and their patients at the centre of an electronically connected care network (Figure 1), with an array of digital technologies supporting what doctors do best and eliminating the administration and red tape that consume too much of their time.
Competing interests: Michael Georgeff is the CEO of Precedence Health Care, which has developed a cloud-based chronic disease management service called cdmNet.
Provenance and peer review: Commissioned, externally peer reviewed.