Hyponatraemia, a common electrolyte abnormality seen in general practice, can have a multitude of underlying causes.1 The most common causes include medication effects, fluid retention and syndrome of inappropriate antidiuretic hormone secretion (SIADH).1 Low serum sodium levels have been linked to increased mortality in some patient groups, including hospitalised patients, older people, and those with heart failure, liver failure or pneumonia.2 Hyponatraemia increases falls and osteoporosis risks and, in severe cases, can be associated with mental state changes, including risk of coma and seizures.2,3 SIADH accounts for about one-third of all hyponatraemia presentations,2 yet remains commonly under-diagnosed and, therefore, under-managed.4 This article will focus on the diagnosis, investigation and management of hyponatraemia secondary to SIADH.
Case study
Mrs SP, 86 years of age, is a nursing home resident who was admitted to hospital following an unwitnessed fall. She had been feeling unsteady on her feet for the past week, but her mental state and vital signs were normal, and there were no neurological deficits on examination. Her past medical history included osteoporosis, hypertension, gastro-oesophageal reflux disorder (GORD) and depression. Mrs SP was on multiple medications, including escitalopram for depression, telmisartan for hypertension, controlled‑release oxycodone/naloxone for chronic back pain, oxybutynin for urinary urge incontinence, simvastatin, pregabalin for sciatica, esomeprazole for GORD and six-monthly denosumab injections for osteoporosis. Investigations in hospital showed severe hyponatraemia with low serum osmolality, and raised urine osmolality and sodium. All other tests were normal (Table 1).
A diagnosis of hyponatraemia secondary to SIADH was made, and serum sodium improved to 120 mmol following fluid restriction of 1000 mL/24 hours. The most likely precipitants for her SIADH were thought to be escitalopram and telmisartan. Mrs SP was discharged back to the nursing home with these two medications ceased.
Repeat blood tests one week post-hospital admission showed improvement with serum sodium (127 mmol), creatinine: 40 µmol/L and estimated glomerular filtration rate (90 mL/min/1.73 m2). Blood pressure remained stable at around 130/80 mmHg. Mrs SP’s fluid restriction was relaxed to 1400 mL/24 hours and serum sodium remained stable at 130–135 mmol over the following two months.
Table 1. Mrs SP’s investigation results
|
Investigations
|
Results
|
Reference range
|
|---|
|
Serum sodium
|
108 mmol (‘)
|
135–145 mmol
|
|
Potassium
|
4.5 mmol
|
3.5–5.0 mmol
|
|
Creatinine
|
40 µmol/L
|
40–90 µmol/L
|
|
Estimated glomerular filtration rate
|
90 mL/min/1.73 m2
|
>90 mL/min/1.73 m2
|
|
Serum osmolality
|
254 mOsm/kg (‘)
|
>275 mOsm/kg
|
|
Urine osmolality
|
140 mOsm/kg (”)
|
<100 mOsm/kg
|
|
Urine sodium
|
39 mmol/L (”)
|
<20 mmol/L
|
|
Thyroid function tests
|
Normal
|
|
|
Chest X-ray
|
Normal
|
|
|
Computed tomography of the head
|
Normal
|
|
Definitions and pathophysiology
Hyponatraemia occurs when a patient’s serum sodium level falls below 135 mmol/L; severe hyponatraemia is defined as serum sodium level below 120 mmol/L.1,2 Causes of hyponatraemia can be divided according to fluid status: hypovolaemic, euvolemic and hypervolaemic.1
- Hypovolaemic hyponatraemia involves reduced extracellular fluid volume with concurrent reduction in serum sodium, as seen in conditions of gastrointestinal losses.1
- Euvolaemic hyponatraemia accounts for the majority of hyponatraemia cases and is defined when the extracellular fluid volume is normal. SIADH, medications (Box 1), hypothyroidism and primary polydipsia are all potential causes of euvolaemic hyponatraemia.1,2
- Hypervolaemic hyponatraemia secondary to cardiac and renal failures or liver cirrhosis occurs when fluid retention is greater than sodium retention, and is associated with increased extracellular volume.1
It is also important to consider hyperglycaemia, which can cause a hypertonic hyponatraemia, and causes of pseudohyponatraemia, such as severe hyperlipidaemia or hyperproteinaemia. In cases of hyperglycaemia, corrected sodium can be calculated taking into account the glucose level.3,5,6
In SIADH, hyponatraemia is due to inappropriate secretion of antidiuretic hormone (ADH). In a normal physiological state, ADH is released in response to increased serum osmolality, whereas in SIADH, ADH secretion is unregulated. Increased production, ectopic production or increased sensitivity to ADH results in increased water permeability of the renal distal tubule and collecting duct through aquaporin insertion. The subsequent dilutional hyponatraemia activates volume-sensitive natriuretic mechanisms, causing salt excretion and maintaining euvolaemic hyponatraemia.3,7
Box 1. Medications associated with hyponatraemia1,2
|
‘CAR DISH’
Chemotherapy
Antidepressants, antipsychotics, anticonvulsants, anti-inflammatory drugs (cyclooxygenase-2 inhibitors)
Recreational drugs (eg ecstasy)
Diuretics
Inhibitors – angiotensin converting enzyme inhibitors, selective serotonin reuptake inhibitors
Sulfonylureas
Hormones (eg desmopressin, oxytocin), hypnotics (eg temazepam)
|
Diagnosis of SIADH
Barrter and Schwartz describe the following criteria for the diagnosis of SIADH:1,3,7
- decreased serum osmolality (<275 mOsm/kg)
- increased urine osmolality (>100 mOsm/kg)
- euvolaemia
- increased urine sodium (>20 mmol/L)
- no other cause for hyponatraemia (no diuretic use and no suspicion of hypothyroidism, cortisol deficiency, marked hyperproteinaemia, hyperlipidaemia or hyperglycaemia).
Investigations for underlying causes
There is an increasing amount of research into causes of SIADH, including hypothalamic or hypophyseal ADH secretion (eg subarachnoid haemorrhage, meningitis, antidepressants, tuberculosis, Guillain-Barré syndrome), and malignancy-related ectopic production (Box 2).1,3 The following investigations should be considered in a patient with euvolaemic hyponatraemia:1,3
- biochemistry looking at serum sodium level
- serum osmolality
- urine osmolality (random sample collected at same time as serum sample)
- thyroid function tests
- morning cortisol level if hyponatraemia is potentially related to Addison’s disease
- computed tomography (CT) of the head if a neurosurgical condition is suspected (eg subarachnoid haemorrhage, subdural haematoma)8
- chest X-ray if pulmonary causes of SIADH are suspected.
Physical examination, including measurement of pulse and blood pressure and assessment of hydration, should also be performed to determine whether the patient is clinically hypovolaemic, hypervolaemic or euvolaemic.
A suggested approach would be to assess the severity of the patient’s hyponatraemia and conduct further investigations accordingly. In mild, asymptomatic cases, review of medications and correction of any suspected underlying causes could be done before repeating the serum sodium level measurement. In cases where the cause of hyponatraemia is not clear and SIADH is suspected, urine sodium and osmolality should be assessed. In severe hyponatraemia where the patient is symptomatic, referral to hospital should be made for further investigation and management.1,3
Box 2. Underlying causes of SIADH2,3,9
|
Neurosurgical or neurological – increased ADH release:
- Guillain-Barré syndrome
- Subarachnoid haemorrhage
- Subdural haemorrhage
|
|
Infective – increased ADH release:
- Meningitis
- Encephalitis
- Abscesses
- Human immunodeficiency virus
- Sarcoidosis
|
|
Respiratory – increased ADH release:
- Tuberculosis
- Pneumonia
- Pneumothorax
- Atelectasis
- Asthma
|
|
Medications – increased ADH release:
- Antidepressants (eg sertraline)
- Anticonvulsants (eg carbamazepine, leveteiracetam)
- Antipsychotics (eg haloperidol)
- Anti-inflammatory drugs
- Ecstasy
- Cyclophosphomide
|
|
Malignancy – ectopic ADH production:
- Nasopharyngeal
- Mesothelioma
- Pancreatic
- Gastrointestinal
- Lymphoma
- Sarcoma
|
|
Non-ADH antidiuretic peptide release:
- Prolactinoma
- Waldenstrom macroglobulinemia
|
|
ADH, antidiuretic hormone; SIADH, syndrome of inappropriate secretion of antidiuretic hormone
|
Management
The first considerations in the management of SIADH are treatment of underlying causes and assessment of whether the patient is symptomatic or asymptomatic. Fluid restriction is first-line therapy in all cases of SIADH.3,7,9 Where hyponatraemia has persisted for longer than 48 hours and is asymptomatic, initial fluid restriction could start at 800–1200 mL per 24 hours, and be subsequently titrated to 500 mL below the daily urine output volume.3
Acute and severe hyponatraemia with an onset less than 48 hours, serum sodium <120 mmol/L and symptoms, including altered mental state and seizures, requires hospital admission. Cerebral demyelination can occur if serum sodium is increased too quickly. Therefore, the increase in serum sodium should not exceed a rate of 10 mmol/L in 24 hours, or 18 mmol/L in 48 hours.1,3 The aim of treatment is to improve symptoms (Figure 1) and obtain a safe sodium level >120–125 mmol/L.1,3,9 While fluid restriction remains the mainstay of therapy in these cases, hypertonic saline may also be considered and would require admission to the intensive care unit.1,3,9
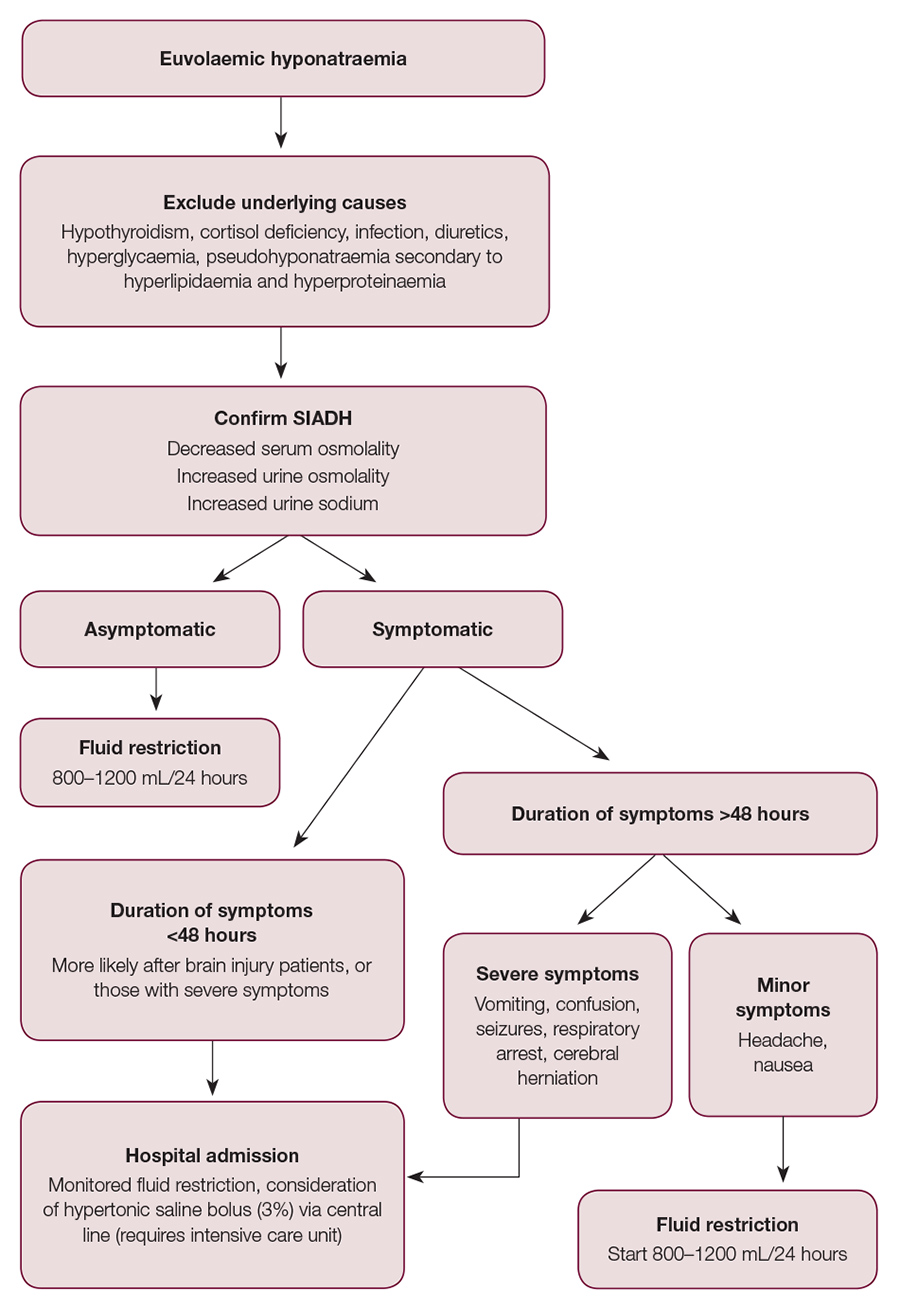
Figure 1. SIADH symptom severity and management flowchart2
Conclusion
Hyponatraemia is one of the most common electrolyte abnormalities to present in general practice, with SIADH being an important but often under-recognised cause. It contributes to increased morbidity and mortality in a range of conditions, and has been associated with increased falls risk and osteoporosis, and altered mental state. Euvolaemic hyponatraemia with low serum sodium and osmolality, and raised urine osmolality in the absence of diuretic use or pseudohyponatraemia, are diagnostic of SIADH.
Medication use should be reviewed, with consideration of further investigations if there is suspicion of malignancy or neurosurgical conditions. Underlying causes should be treated and patients should commence fluid restriction of 800–1200 mL/24 hours. Severe hyponatraemia with altered mental state warrants hospital admission for fluid monitoring and possible infusion of hypertonic saline. Care should be taken to increase serum sodium at appropriate rates to avoid cerebral demyelination.
General practitioners have a crucial role in preventing the development of severe, symptomatic hyponatraemia, and this begins with the simple suspicion of SIADH as an underlying cause.
Authors
Kristen Tee MBBS, DCH, CWH, General Practice Registrar with ProHealth Care, Kidman Park, SA. k.tee@prohealthcare.com.au
Jerry Dang MBBS, Basic Physician Trainee, Lyell McEwin Hospital, Elizabeth Vale, SA
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.