The development of a bent erection, usually for no obvious reason, causes real concern to men who develop Peyronie’s disease, and there is reluctance to talk about it. François Gigot de La Peyronie first described the condition in 1743,1 but despite generations of research and treatments, Peyronie’s disease is still not understood fully, and has proven resistant to a ‘cure’. No treatment can return the penis completely to its pre‑disease state.
Aetiology and clinical presentation
Up to 9% of men will have evidence of Peyronie’s disease if asked and examined, although the number of men presenting with symptoms of Peyronie’s disease are far fewer.2,3 The peak incidence of Peyronie’s disease is around 55–60 years of age, and penile curvature is the most common presentation, followed by feeling a nodule in the penis. Painful erection is reported by over half of the patients with Peyronie’s disease.3,4 A history of remembered penile trauma is reported by only about 10% of patients with Peyronie’s disease,5 generally younger patients.
Peyronie’s disease is known to be associated with erectile dysfunction, and approximately 30% of patients with Peyronie’s disease will also have diabetes.6 Peyronie’s disease has a significant association with obesity,7 hypertension, hyperlipidaemia,5 smoking and pelvic surgery.6 It has been noted to affect 16% of patients after radical prostatectomy.8 An association with Dupuytren’s disease is also well recognised.6 The increasing incidence of erectile dysfunction with age probably relates to the increasing prevalence of Peyronie’s disease with age, as the loss of ‘stiffness’ or axial rigidity of the penis causes minor flexion injury during normal sexual activity.
Peyronie’s disease can also cause significant emotional stress, in part as a result of the deformity and associated difficulties with sexual function, but often also because of the penile shortening that occurs in almost all patients. Up to 50% of patients with Peyronie’s disease may be diagnosed as being clinically depressed.5
Peyronie’s disease is an abnormal wound healing condition that occurs in genetically predisposed men, with ‘trauma’ to the structural layers of the penis (Figure 1).9 The abnormal healing leads to a fibrous inelastic scar that causes a palpable mass or plaque, which, with an erection, causes curvature, shortening, narrowing or a hinge effect. This occurs because the affected part of the penis will not ‘stretch’ with erection.10 In the early phase, there may also be an inflammatory component that causes pain.
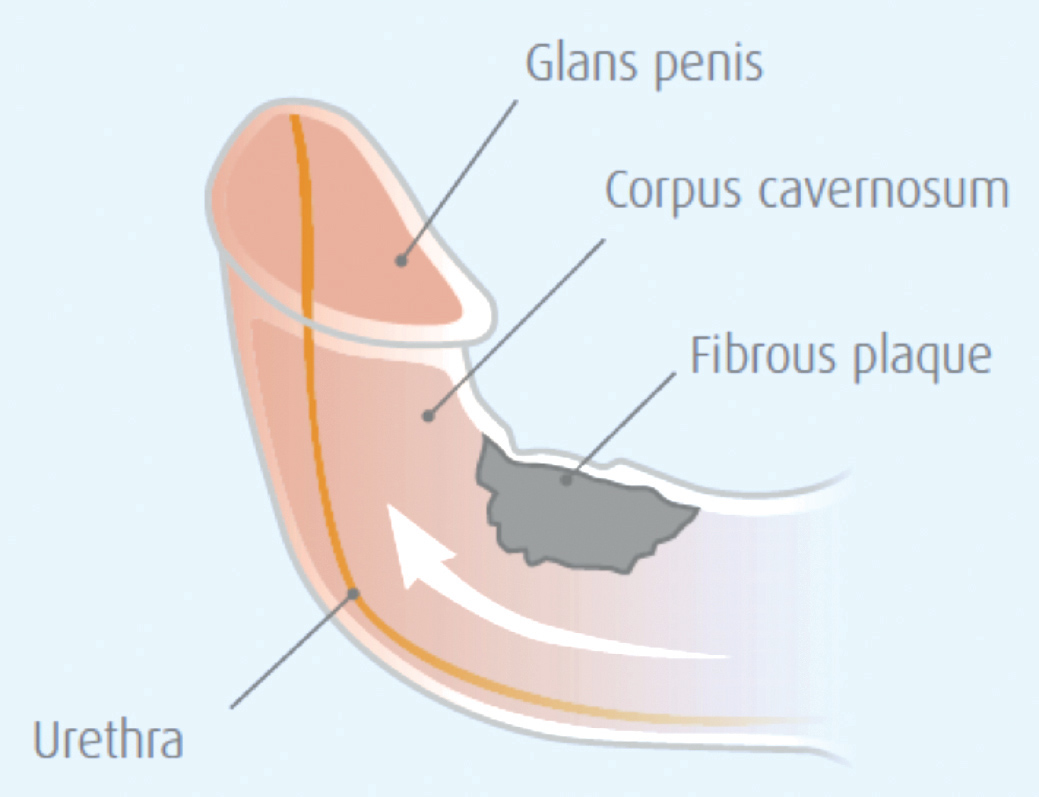
Figure 1. Anatomy of peyronie’s disease
Peyronie’s disease is a progressive process, with most men experiencing progression in the first few months after onset, which may not be influenced by early treatment.11 Peyronie’s disease is generally divided into two pathological and clinical phases. The first phase is an acute inflammatory phase where there may be penile pain and curvature progression, although the pain typically resolves spontaneously within 12 months and the curvature usually stabilises.11 The second phase is a chronic phase, commonly defined as resolution of pain, and stability of the curvature for longer than three months.
Patient evaluation
Diagnosis of Peyronie’s disease is readily made by a typical history and penile examination. Clinically important information includes:
- stage of the disease (ie active versus chronic)
- curvature features (ie direction, degree)
- penile length and other associated penile deformities (eg hourglass deformity)
- presence of pre-existing or co-existing erectile dysfunction.
Short disease duration (<12 months), ongoing penile pain and continuing changes in penile deformity are likely indications of the acute phase. Physical examination in the flaccid state will often disclose an indurated area or an obvious penile plaque, even though patients may be unaware of it.12 However, evaluation of a flaccid penis is inadequate when evaluating Peyronie’s disease deformity – the degree of angulation is not fully appreciated and patients tend to overestimate the degree of angulation. Commonly, the curvature direction corresponds with the location of the plaque. In two-thirds of patients, the plaque is positioned on the dorsal surface of the penis. Lateral and ventral plaques are less common but are more likely to impair penetration. Multiple plaques located on opposite sides of the penis, or plaques appearing in the septum, may result in penile shortening with a relatively straight penis.13
Investigations in Peyronie’s disease
Generally, diagnosis of Peyronie’s disease is based on clinical findings. When referred to a specialist, the urologist may undertake a duplex Doppler ultrasound combined with an intracavernosal vasoactive agent. This allows the urologist to objectively measure the patient’s penile blood flow parameters, the penile curvature and other deformities, and plaque characteristic (eg calcification). These parameters can help direct treatment options.14 Magnetic resonance imaging (MRI) is very rarely indicated and should only be organised by a specialist.
Nonsurgical management of Peyronie’s disease
Observation
Patients should be advised that if pain and curvature are minimal and normal sexual function is maintained, or if the patient is not sexually active, pursuing medical or surgical intervention may not be warranted. At times, the patient seeks only reassurance rather than intervention.
Oral therapy
There is no oral agent that cures Peyronie’s disease and most of the commonly used treatments that patients ‘source’ from, or investigate on the internet, have had no efficacy in proper clinical trials. If oral agents are to have any benefit, these probably need to be instituted very early in the disease process, but there is significant doubt that any offer real benefit. In addition, these oral agents are ‘off-label’ when treating Peyronie’s disease exclusively.
Pentoxifylline
Pentoxifylline is a nonspecific phosphodiesterase inhibitor that may increase penile levels of nitric oxide and may prevent, or reverse, calcification of the Peyronie’s plaque.15 However, this drug is usually taken three times per day and has gastrointestinal side effects, which limits its use.
Phosphodiesterase type-5 inhibitors
Phosphodiesterase type-5 (PDE5) inhibitors that are available in Australia are sildenafil, tadalafil and vardenafil. Animal studies have found that these drugs, which are designed to augment erections, can reduce the collagen or smooth muscle and collagen III–I ratios in the Peyronie’s disease-like plaque.16 In a retrospective controlled study, daily tadalafil (5 mg) resulted in statistically significant resolution of septal scar in 69% of patients, compared with 10% in the control group.17 As there is often co-existing erectile dysfunction in patients with Peyronie’s disease, we usually recommend low-dose PDE5 inhibitors for acute-stage Peyronie’s disease, although we advise patients that evidence for the use of these agents, purely for their ‘antibrotic effects’, is poor.
Intralesional injections
Agents that are injected into the plaque have more promise for improvement, and are now widely studied and accepted as worthwhile treatments.18 While used primarily in the chronic or stable phase of the disease, intralesional injections may have a role earlier in the process.
Collagenase
The use of intralesional injections of collagenase, plus physical modelling of the penis, have been reported to cause decreases in curvature.19 In two large prospective randomised, placebo‑controlled, double-blind studies, the overall response was an average improvement of 37% in curvature, compared with 17% (P <0.05) in the placebo arm.20 It is important to note that with a curvature of 60°, a 37% improvement actually equates to curvature improvement of 22°; this should be conferred clearly to the patient. Results may be unsatisfactory for patients with a calcified plaque, a high-degree curvature, or associated hinging or hourglass deformity. Although approved by the Therapeutic Goods Administration in Australia in 2016, collagenase is not listed on the Pharmaceutical Benefits Scheme and is very costly. Multiple injections are required through multiple cycles and, between cycles, patients are required to undergo penile modelling exercises. Patients need to be properly evaluated and informed before starting collagenase injections. Ideally, collagenase injections should only be administered by a specialist or a general practitioner specialising in men’s health.
Verapamil
Verapamil has been found to affect fibroblast cellular activity. Some studies have found that intralesional verapamil injection induces a significant reduction in penile curvature.21 However, verapamil is not an approved treatment for Peyronie’s disease, but has been used off-label.
Other noninvasive therapy
Low-intensity shockwave therapy
Low-intensity shockwave therapy for the treatment of Peyronie’s disease has been found to have only very minor benefit.22
Penile traction devices and vacuum pumps
In several tissue models, including Dupuytren’s scar, gradual expansion of tissue by traction has been found to result in the formation of new connective tissue by cellular proliferation.23 For patients who are very motivated, a six-month trial of regular, everyday use of a vacuum erection device, or penile traction device, may result in up to 25% improvement in curvature.24 These devices are also used in conjunction with medical therapy, and may help to improve results, compared with medical therapy alone.
Surgical treatments for Peyronie’s disease
Surgery remains the gold standard for correcting penile deformity. Surgery is indicated when the patient has:25
- stable disease
- minimal-to-no pain
- difficulty with or inability to engage in sex because of the deformity
- desire for the most rapid and reliable result.
Various authorities have different recommendations on the minimum time for stable disease before surgery. We believe an absolute minimum of three months of stable, pain-free disease is required before surgery.
The aim of surgery is to correct curvature to allow a ‘functionally’ straight erection. This equates to a curvature of <20°, which is usually sufficient to allow for satisfactory intercourse. Some patients may request surgery for psychological or body image reasons, even with lesser curvatures. In the pre‑operative consultation, it is very important to be sure that the patient understands this aim (ie a functionally straight erection), and that the penis cannot be restored to its previous state. As some men have minor deformities that are functionally not significant, they need to fully understand the risks and realistic outcomes of surgery versus the minor deformity they may have and, in many cases, be dissuaded from surgery.
There is a general agreement that for men with adequate pre-operative erectile function and rigidity, and with a curvature of <60°, some form of procedure to shorten the ‘long’ (convex) side of the curved penis, such as a tunica albuginea plication, (often called a Nesbit plication; Figure 2), is indicated. For those with more severe deformity but still good pre-operative rigidity, plaque incision or excision and grafting (lengthen the ‘short’ side; Figure 3) is recommended.26 For patients with poor erectile function or rigidity that cannot be improved pharmacologically, and a significant curvature, penile prosthesis implantation with or without ancillary procedures is recommended,27 even penile disassembly and re-assembly techniques.28
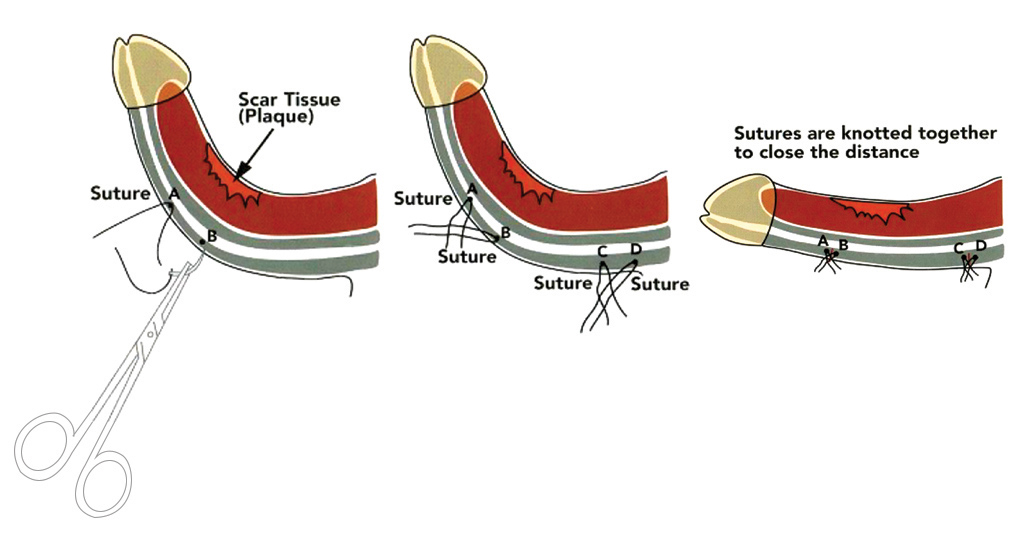
Figure 2. Penile plication procedure
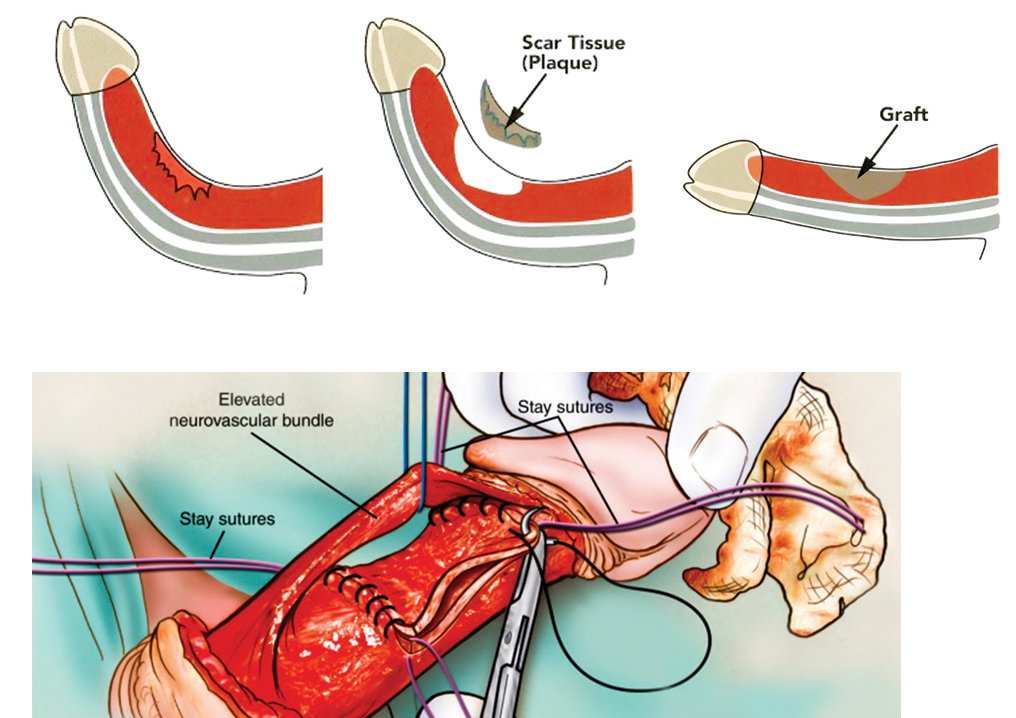
Figure 3. Plaque incision and graft
Conclusion
The most important part of treatment for Peyronie’s disease is to set appropriate expectations. Peyronie’s disease is a clinical diagnosis and definitive treatment is reserved for the stable phase of the condition. Intralesional collagense is the only nonsurgical treatment that has good evidence to suggest that it may offer modest improvement in penile curvature.
Surgical correction of Peyronie’s disease remains the only treatment that will give a functionally straight penis in the majority of patients. Changes and improvements in surgical techniques, ancillary therapies and the availability of better grafting materials have helped to make surgery for Peyronie’s disease a viable and successful treatment option for properly selected patients. Surgical therapy is beneficial for properly selected and counselled patients, and can greatly improve their quality of life.
Key practice points
- Penile bend, palpable lump in the penis and some discomfort are common presenting features of Peyronie’s disease; however, it should be noted that Peyronie’s disease can have a variable onset, and this variability and unpredictability are features of this condition.
- There is often a history of some erectile dysfunction, usually based on vascular risk factors, preceding the development of Peyronie’s disease.
- Peyronie’s disease is a wound healing disorder, the injury or trauma that initiates it often being subclinical, and the symptoms usually develop and change over some 6–12 months before the chronic phase ensues.
- Diagnosis of Peyronie’s disease is largely based on history and examination, and specific investigation, at the general practice level, is not usually indicated.
- Referral to a specialist urologist should be considered if Peyronie’s disease is causing sexual difficulties or patient anxiety, curvature continues to progress or the diagnosis is not clear.
- The goal of surgery is to achieve a functionally straight erection. There is no treatment that can reverse Peyronie’s disease and thereby restore the penis back to the pre-disease state.
- Surgical treatments for the curvature of Peyronie’s disease remain the gold standard, but should only be performed in the stable or chronic phase, and patients must have realistic expectations about outcome.
Authors
Christopher Love MBBS, FRACS (Urology), Urological and Prosthetic Surgeon, Men’s Health Melbourne, Melbourne and Urology South, Moorabbin, Vic; Senior Urological Surgeon, Department of Urology, Monash Medical Centre, Clayton, Vic; Bayside Urology, Melbourne, Vic chris@drlove.com.au
Darren J Katz MBBS, FRACS (Urology), Urologist and Prosthetic Surgeon, Men’s Health Melbourne; and Urology Consultant, Western Health, Vic
Eric Chung Eric Chung MBBS, FRACS (Urology), Associate Professor of Surgery and Consultant Urological Surgeon, Androrology Centre, Brisbane, Qld; University of Queensland, Department of Urology, Princess Alexandra Hospital, Brisbane, Qld
Ohad Shoshany MD, Andrology and Sexual Health Fellow, Men’s Health Melbourne and Western Health, Vic
Competing interests: Dr Love, Dr Katz and Dr Chung are advisory consultants for Actelion, which manufactures drugs for the treatment of Peyronie’s disease, and have received personal fees from Actelion.
Provenance and peer review: Commissioned, externally peer reviewed