Chest pain is a common presentation in general practices and emergency departments. The cause of chest pain presentations can vary from benign and self-limiting (eg musculoskeletal, chest wall pain) to potentially life-threatening conditions, such as acute coronary syndrome (ACS), aortic dissection or pulmonary embolism. Primary care data estimate that 1–4% of chest pain presentations to general practitioners (GPs) are secondary to the effects of ACS.1,2 In addition, 15% of patients diagnosed with ACS have had an initial review with their primary care physician.3
Ischaemic heart disease (IHD) continues to be a significant public health burden. In Australia in 2014–15, 643,000 adults (aged 18 years and older) had IHD. This number represents approximately 4% of the population.4 Acute admission of patients with ACS to hospital contributes significantly to this burden. In 2009–10, there were 55,219 and 34,037 hospitalisations for acute myocardial infarction (AMI) and unstable angina respectively.5
Appropriate clinical assessment of chest pain includes history (including cardiovascular risk factor assessment), physical examination and performance of 12-lead electrocardiogram (ECG). The advent of troponin testing over the past 20 years and, more recently, high-sensitive troponin (Hs-Tn) has added an important diagnostic tool in the assessment of patients with chest pain. It is imperative that primary care physicians have a diagnostic framework for assessing chest pain and understand the role of troponin testing.
What is troponin?
Troponins are protein molecules that regulate the contraction and excitation of striated cardiac muscle. Myocardial injury and necrosis can lead to the release of troponin into the circulation, which can also be secondary to inflammation and apoptosis.6 Levels become elevated after a few hours and may remain elevated for seven to 10 days (Figure 1). The two most common types of troponin that are measured in clinical practice are troponin I and troponin T.
Troponin testing is primarily used by clinicians in the evaluation of patients who present with symptoms that are suggestive of ACS. However, it is important to recognise that the causes of elevated troponin levels are varied. Appropriate interpretation of an elevated troponin level requires clinical equipoise in deciding appropriate further investigation and management.
Troponin testing in primary care patients in whom there is suspicion of ACS may lead to a delay in referral to a hospital with cardiology facilities for further evaluation and definitive treatment. This delay could result in complications of ACS, and increased morbidity and mortality (eg significant myocardial infarction or lethal ventricular arrhythmia). It is reasonable for a GP to order a troponin test to exclude ACS in a patient who is low-risk and asymptomatic, and in whom the symptoms have completely resolved 24 hours prior to presentation.7
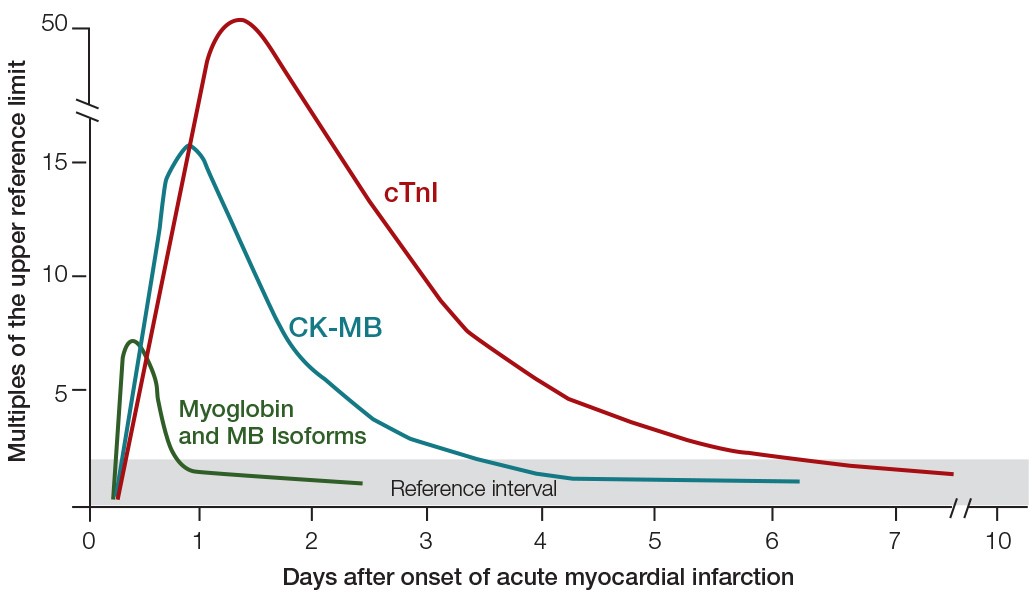
Figure 1. Troponin rise and fall
CK, creatine kinase; MB, myocardial band; cTnI, cardiac troponin I
High-sensitive troponin
Over the past 10 years, improvements in laboratory technology have resulted in the development and use of Hs-Tn assays. Hs-Tn has superior analytical performance, compared with standard assays, leading to improved risk stratification and earlier diagnosis of patients with suspected AMI.8 The benefit of Hs-Tn assay is the timely detection or exclusion of AMI. This can allow early implementation of treatment or facilitate early discharge from the emergency department, where appropriate.9
Hs-Tn enhances risk assessment, compared with standard assays, and may detect an additional 4% (representing a 20% relative increase) of patients with chest pain who are at increased risk of death or recurrent ischaemia from AMI.10 Hs-Tn use has also resulted in a reciprocal decrease in the diagnosis rates of unstable angina in patients presenting with chest pain to the emergency department.11 Unstable angina represents chest pain occurring with myocardial ischaemia at rest or with minimal exertion without myocardial necrosis (and therefore without consequent troponin release). If available, Hs-Tn use is recommended by the Cardiac Society of Australia and New Zealand and the European Society of Cardiology in preference to standard assays.11,12
The predominant disadvantage of Hs-Tn is the detection of myocardial damage that is unrelated to acute myocardial ischaemia. This results in reduced specificity as more patients with non-ACS causes of myocardial injury have an elevated Hs-Tn, compared with standard assays. Non-ACS detection of an elevated Hs-Tn is more common than with standard assays because of the ability of Hs-Tn assays to detect small changes in levels that may have no, or be of little, clinical significance. This has the potential for misdiagnosis of an ACS with increased ‘downstream testing’, such as unnecessary invasive coronary angiography.
Point-of-care troponin
Point-of-care troponin testing has emerged as a clinical tool that can be used to provide a rapid result when access to hospital or laboratory services may be limited. There are a number of commercial assays available; however, these tests traditionally have lower diagnostic accuracy, compared with laboratory-based results. As these assays improve, they are likely to have an emerging role in analysing chest pain in primary care.
What does elevated troponin mean?
The most likely diagnosis in a patient presenting with symptoms suggestive of ACS, and in whom troponin is elevated, is ACS secondary to AMI. The definition of AMI is outlined in Box 1. A clinical classification of AMI has also emerged as a useful clinical tool in differentiating the clinical–pathological aetiology of AMI, which is outlined in Box 2.
Elevated troponin can also be present in a number of non-ACS conditions.13 Careful clinical evaluation, measuring serial troponin values to assess the rise and fall in concentration, and the absolute concentration of troponin are used to make an assessment regarding the cause of cardiac injury.14 The causes of an elevated troponin are listed in Box 3.
Box 1. Definition of acute myocardial infarction17
|
Acute myocardial infarction is diagnosed when there is evidence of myocardial necrosis in the setting of a clinical presentation that is consistent with acute myocardial ischaemia
Detection of a rise (and fall) of a cardiac biomarker with one value >99th percentile of the upper reference limit, and with at least one of the following:
- Symptoms of myocardial ischaemia
- New or presumed new ST-segment/T-wave changes or new left bundle branch block
- Development of pathological Q waves on 12-lead electrocardiogram
- Imaging evidence of new loss of viable myocardium or a new regional wall motion abnormality
- Identification of intracoronary thrombus by angiography or autopsy
|
|
Adapted with permission from Oxford University Press from Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J 2012;33(20):2551–67.
|
Box 2. Types of acute myocardial infarction
|
Type 1: Myocardial infarction secondary to plaque rupture and thrombus formation
Type 2: Myocardial infarction secondary to ischaemic imbalance
(ie reduced oxygen supply with secondary ischaemia and infarction)
Type 3: Myocardial infarction resulting in sudden death when serum biomarkers are unavailable
Type 4: Myocardial infarction related to percutaneous coronary intervention
Type 5: Myocardial infarction related to coronary artery bypass surgery
|
Box 3. Causes of elevated troponin in the absence of an acute coronary syndrome
|
Cardiac aetiology:
- Cardiac contusion/cardiac surgery
- Post-electrophysiological procedure (ablation) or PPM implantation
- Aortic dissection
- Aortic valve disease
- Hypertrophic cardiomyopathy
- Tachyarrhythmias
- Takostubo cardiomyopathy
- Infiltrative disease (eg amyloidosis, haemochromatosis, sarcoidosis, scleroderma)
- Inflammatory diseases (eg myocarditis)
Non-cardiac aetiology:
- Rhabdomyolysis (with cardiac injury)
- Pulmonary embolism; severe pulmonary hypertension
- Renal failure
- Acute neurological disease (including cerebrovascular accident, sub-arachnoid hemorrhage)
- Critically ill patients (especially with respiratory failure or sepsis)
- Extreme exertion
|
When might it be appropriate to order a troponin test in general practice?
There are some situations where it may be appropriate for a GP to order a troponin test, and the position that a troponin test should never be ordered in the community setting is an oversimplification. Generally, there are two situations where it might be reasonable for a GP to order a troponin test in the community. The first is when a patient has had symptoms of ACS in the preceding days but, on presentation, the symptoms have completely resolved and the patient is clinically stable and deemed to be at low risk. The second is when a patient presents with atypical symptoms and has a low likelihood of ACS, and the clinician uses troponin testing to essentially ‘rule out’ ACS to cover clinical uncertainty. A 12-lead ECG contributes further to this risk assessment, albeit with the limitation that up to one-third of patients with non-ST elevation ACS may have a normal ECG.15 A positive troponin result in this setting may occasionally be detected, which will subsequently allow for appropriate management and specialist referral.7,13
If primary care Hs-Tn testing is performed in atypical, low-risk presentations with chest pain, it is important that a serial troponin test is performed three hours after the presentation if the symptoms have been present for <6 hours at the time of clinical review and the initial Hs-Tn test.11 Late increases in troponin have been described in about 1% of patients with recurrent chest pain.11 Therefore, clinical risk assessment should be ongoing, including consideration of alternative, non-ACS diagnoses.
Pitfalls when ordering a troponin test in general practice
Ordering a troponin test in the community setting should be done cautiously. Troponin testing should not delay referral of patients with suspected ACS to hospital, as this can lead to increased morbidity and mortality. It is not appropriate to measure serial troponin levels in the community, as the patient will not be monitored for possible worsening symptoms and potential complications. It is also not recommended to measure troponin in asymptomatic patients or to use troponin as a screening tool, as the result may be problematic, with no clear management strategy, and could lead to unnecessary investigations.
If a troponin test is ordered in the community, it should be clearly marked as urgent, and there should be a mechanism in place for the doctor and patient to be contacted with the results. If these logistics are not in place, this could lead to potential delays with follow-up of positive results. The patient could potentially be in the community with an elevated troponin level without adequate follow-up and not receiving appropriate clinical care. As a consequence, the degree of myocardial infarction may extend and the patient could experience serious ventricular arrhythmias.7,16 If there is a lack of capacity to receive troponin results and arrange appropriate clinical follow-up when performed in the community on low-risk patients (eg late in the day, weekends), then referral to an emergency department is appropriate.
It is widely acceptable clinical practice to promptly refer patients who present with symptoms suggestive of ACS to hospital without first undertaking community troponin testing.
Conclusion
Cardiac troponin is a serum biomarker used as a diagnostic tool to detect myocardial damage. Patients should be referred immediately to hospital when presenting with symptoms suggestive of ACS. Primary care physicians should take care when ordering a troponin test to ensure the result is communicated promptly and there is a mechanism in place for the patient to be contacted if required.
Key points
- Patients presenting with possible ACS and symptoms occurring within the previous 24 hours should be promptly referred and transported to a hospital emergency department.
- Absence of an elevated troponin does not exclude unstable angina, and urgent cardiac assessment is still appropriate if the presenting symptoms are highly suggestive of ACS.
- Troponin testing should not be ordered unless there is a mechanism to review the result as soon as it is available.
- Troponin testing may have a limited role in primary care in the following scenarios:
- low-risk patients in whom symptoms have completely resolved 24 hours prior to presentation
- atypical symptoms with a low likelihood of ACS, where troponin testing may essentially ‘exclude’ ACS to cover clinical uncertainty
- recent symptoms of an ACS where the patient can be appropriately monitored in a general practice setting while waiting for the result.
Authors
Manuela S Mauro MBBS, FRACGP, General Practitioner, ProHealth Care, Kidman Park, SA
Adam J Nelson MBBS, BMedSc (Hons), Cardiology Registrar, Clinical Lecturer, Department of Cardiology, Royal Adelaide Hospital, University of Adelaide, SA
Michael B Stokes MBBS, FRACP, Cardiologist, Department of Cardiology, Royal Adelaide Hospital, Centre for Heart Rhythm Disorders, South Australian Health and Medical Research Institute, University of Adelaide, SA. mbstokes83@gmail.com
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.