Diverticulosis, the presence of small outpouchings of the intestinal wall (diverticula), occurs in 10% of people over the age of 45 years and 65% of those aged over 70 years. It affects men and women equally and increases with age.1 Diverticulosis is thought to develop when pressure-induced diverticula form in the intestinal wall. The sigmoid colon experiences the highest intracolonic pressures and is the most common site of diverticulosis. Any region of the colon can be affected, but diverticulosis is more prevalent in the right colon in Asian populations.2,3
Diverticular disease encompasses the spectrum of presentations and complications of diverticulosis. It is proposed that diverticular disease is related to a low intake of fibre.2 Among those affected, only 15–20% are symptomatic; of those who are symptomatic, one‑quarter develop inflammation of the colonic diverticula (diverticulitis) and, uncommonly, massive diverticular bleeding.3 The preferred modality for diagnosis of diverticulitis is computed tomography (CT) with intravenous contrast.3
Diverticulitis can be stratified as uncomplicated or complicated on the basis of whether complications such as fistula, perforation, obstruction or massive diverticular bleeding are present. In uncomplicated diverticulitis, severe disease is differentiated from moderate disease by evidence of systemic infection, peritonitis, inability to tolerate oral intake or failure of outpatient management. Other signs of severe disease include persistent fever or leukocytosis, or worsening pain after two to three days. The mainstay of management for patients with uncomplicated severe diverticulitis includes bowel rest and broad-spectrum antibiotics (Figure 1).
Following an acute presentation of diverticulitis, colonoscopy is generally undertaken to exclude neoplasia.4 Involvement of a dietitian and advice regarding a high-fibre diet and avoidance of nuts, seeds and corn is employed to reduce symptoms and prevent recurrence.1,4 In this article we review the evidence regarding the utility of a high-fibre diet, avoidance of nuts, seeds and corn, the necessity of colonoscopy following CT-diagnosed diverticulitis, and the utility of antibiotics.
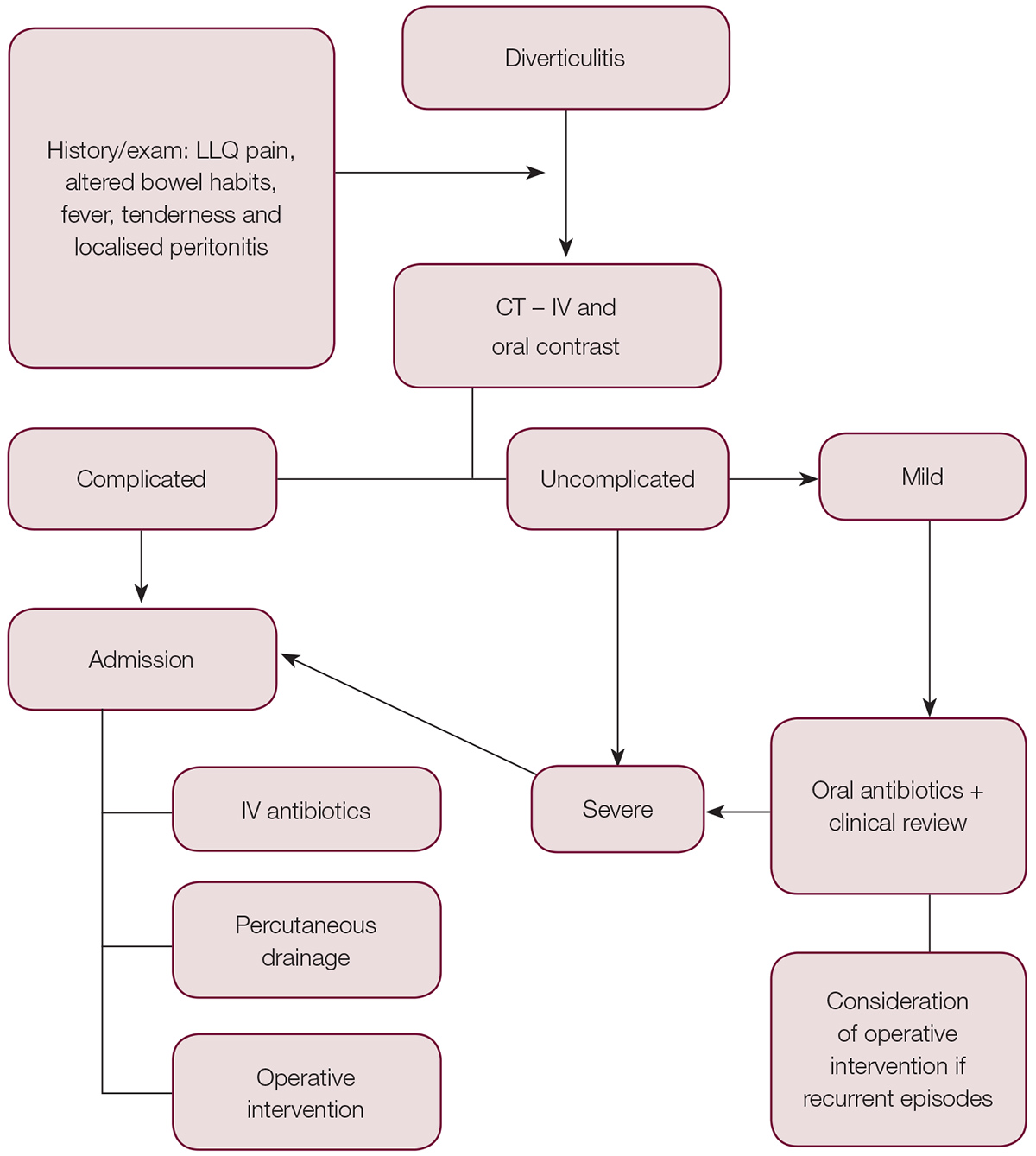
Figure 1. Algorithm of assessment, diagnosis and management of diverticulitis
CT, computed tomography; IV, intravenous; LLQ, left lower quadrant
Aetiology and presentation
The mechanism underlying diverticulosis is understood to involve pressure-induced formation of diverticula in the colonic mucosa at intrinsically weak points where arterioles penetrate the circular muscle layer to supply the mucosa. These arterioles arise as the inferior and superior mesenteric arteries form collaterals through the arc of Riolan and the marginal artery of Drummond and a series of arcades. The terminal arcades then penetrate the muscular layer as vasa recti to form the submucosal plexus.
Diverticular formation is primarily due to raised intracolonic pressures, most commonly in the sigmoid colon. Low-fibre Western diets predispose to prolonged colonic transit, increased water resorption and low stool bulk, thereby increasing colonic pressures.5,6 The natural history of diverticula ranges from asymptomatic to symptomatic diverticular disease and, finally, complications such as diverticulitis or diverticular bleeding.
Symptomatic diverticular disease is typified by abdominal pain and irregular bowel habits. Diverticulitis is hypothesised to be due to obstruction of the diverticula neck by faecolith, which causes localised bacterial overgrowth and inflammation. The ensuing oedema and inflammatory infiltrate then lead to localised perforation, which can be contained by adjacent bowel or omentum, or can progress to generalised peritonitis.1
A typical presentation of diverticulitis includes left lower quadrant pain, diarrhoea, fever and localised peritonitis. Diagnosis is typically made with intravenous contrast-enhanced CT; however, interval colonoscopy is recommended because neoplasia can present with similar features clinically and radiographically.7 Non-contrast CT is suboptimal and may result in further imaging being required.
Colonoscopy after diverticulitis
Most gastroenterology and colorectal surgical publications recommend that patients presenting with CT-diagnosed diverticulitis should undergo colonoscopy to exclude malignancy. However, data to support such a recommendation are scarce.8 This recommendation is primarily based on expert opinion, with the rationale of excluding malignancy that mimics acute diverticulitis. It stems from a time when less sensitive and specific techniques were used, including physical examination and barium enema.
With the use of contrast-enhanced CT, the recommendation for colonoscopy may no longer be valid.7,9 Systematic reviews and meta-analyses suggest that the risk of colorectal malignancy is low in patients with uncomplicated CT-diagnosed acute diverticulitis.10 A large case-control study found that diverticulitis did not increase the risk of being diagnosed with colorectal cancer in the long term, and that the increased risk within 12 months of diverticulitis may be due to misclassification and increased surveillance. Furthermore, colon cancer mortality was unaffected by a history of diverticular disease.11 A systematic review found that the prevalence of colon cancer in those with CT-diagnosed diverticulitis was low and more closely approximates the prevalence in the asymptomatic general population. With the diagnostic accuracy of CT for acute diverticulitis, the recommendation of follow-up colonoscopy may not be justified.7
Two further systematic reviews found that the risk of malignancy after radiologically proven diverticulitis is low, and proposed that in the absence of other indications, routine colonoscopy may not be necessary. A more selective approach based on higher risk features should be used. Such features include abscess, localised lymphadenopathy, relative absence of diverticula, focal mass effect or more than one site of inflammation (‘fat stranding’) on CT.10,12 Several retrospective studies had similar findings, suggesting that those with diverticular complications, such as abscess or fistula, are at higher risk of malignancy than those with uncomplicated diverticulitis, and should undergo colonoscopy.8,13
It should be noted, however, that age-appropriate colonoscopic screening should occur in patients with risk factors who present after uncomplicated diverticulitis. This includes patients who have had a positive faecal occult blood test or those with an elevated risk of colorectal cancer because they have a first-degree relative diagnosed with colorectal cancer before 55 years of age or two first-degree or one first-degree and one second-degree relative diagnosed with colorectal cancer on the same side of the family.7
Overall, the available evidence suggests that while malignancy cannot be entirely excluded in all cases of uncomplicated CT-diagnosed diverticulitis, the risk of malignancy is low and routine interval colonoscopy in all patients is potentially not justified. In one systematic review and meta-analysis, the proportional estimate of malignancy risk in uncomplicated diverticulitis was only 0.7%, compared with 10.8% in those with complicated diverticulitis.10
We recommend that colonoscopy is not necessarily required in patients who are being followed up after uncomplicated diverticulitis. A more selective approach to the use of colonoscopy, such as for those with high-risk features, personal preference or family history, is more appropriate.
Dietary factors
Avoidance
Once the acute episode of diverticulitis is treated, the mainstay of advice on discharge is to increase the intake of dietary fibre and avoid foods that could predispose to a further episode of diverticulitis, mainly corn, nuts and seeds. This stems from the theory that luminal trauma is a causal mechanism that relates to diverticulitis and diverticular bleeding. The assumption is that foods such as nuts, seeds or corn can obstruct the neck of a diverticulum and precipitate diverticulitis.4 The Health Professional Follow-up Study (HPFS) is the first major study to assess the effect of these foods on the occurrence of diverticulitis. This study, involving more than 47,000 health professionals in a prospective cohort design, found no increased risk of diverticulosis or diverticular complications in those consuming these foods.4 Since the HPFS, there have not been any further reliable data addressing this issue.
Given the paucity of evidence surrounding the dietary claims about avoidance of foods such as nuts, seeds and corn, and the numerous health benefits of some of these foods, this standard dietary advice should be considered carefully. We recommend that patients should not be instructed to avoid these foods to reduce risk.
Fibre
Dietary advice also includes introducing a high-fibre intake into the diet, attempting to reduce intracolonic pressures and colonic transit time, thereby reducing the formation of diverticula and their complications. The evidence for dietary fibre supplementation comes predominantly from large observational and cohort studies, with very little higher level evidence. However, randomised controlled trials are generally not feasible at these population-level associations. The European Prospective Investigation into Cancer and Nutrition (EPIC)-Oxford study, using a cohort design, followed more than 47,000 men and women. This study found that a higher intake of dietary fibre was associated with lower rates of diverticular disease (including diverticulitis and bleeding) and lower rates of hospitalisation.14
The HPFS also found a strong inverse relationship between dietary fibre intake and symptomatic diverticular disease.4,15 There is also evidence for significantly fewer complications and a lower requirement for surgery in patients who are on a high-fibre diet.16 It seems reasonable, therefore, to continue to recommend a high-fibre diet for patients who have had an episode of diverticular complications.
Given the large economic cost of diverticular disease and its associated hospital admissions, as well as the high prevalence in Westernised countries, reductions in the occurrence of diverticulitis can have far-reaching implications for the healthcare system. With respect to reducing the occurrence of diverticulosis in the first instance, the evidence is less clear. Early observational data found lower rates of diverticulosis in populations with a higher intake of fibre.17,18 However, a cross-sectional study in 2012 found that a high-fibre diet actually increased the risk of asymptomatic diverticulosis.19 It seems that evidence is lacking to suggest that a high intake of dietary fibre actually reduces the development of diverticulosis.
Although a correlation exists between a low-fibre diet and the development of diverticular disease and its complications, a causal link has not been demonstrated conclusively. Given the health benefits of a high-fibre diet, however, this should still be recommended despite weak evidence.
Antibiotics in diverticulitis
The most recent point of contention concerns the utility of antibiotics in treating diverticulitis. With the rise of antibiotic resistance and the potential healthcare budget savings of treating uncomplicated diverticulitis with only bowel rest, studies have begun to address this issue.
Uncomplicated diverticulitis refers to the absence of complications, such as perforation or fistula, as defined earlier in this article. Early trials suggested that acute uncomplicated diverticulitis can be safely treated without antibiotics and that this management does not increase further events of diverticulitis.20 However, international guidelines include the recommendation of oral or intravenous antibiotics, which is largely based on expert opinion.21 Recently, studies have found that management without antibiotics is indeed safe and not associated with an increased risk of adverse events, which tend to be more prevalent in patients with high-risk complicated diverticulitis.22,23
There have been two major randomised clinical trials addressing the issue of whether to use antibiotics. A large multicentre trial found that observational management alone did not prolong recovery or increase mortality, re-admission or complications.24 Another landmark trial (the Multicenter Randomized Clinical Trial Investigating the Cost-effectiveness of Treatment Strategies With or Without Antibiotics for Uncomplicated Acute Diverticulitis [DIABOLO]) further supports this. DIABOLO found that in selected patients with uncomplicated acute diverticulitis, treatment without antibiotics did not alter those same primary endpoints.25
While the available data suggest that observational management may be safe and effective, they are insufficient to change current practice, as the specific population groups to which this approach should be applied have not been identified. Incorrect classification of patients as having moderate or uncomplicated diverticulitis without a defined population group could result in these data being applied to patients who require inpatient care.
Although data suggest that patients with acute uncomplicated diverticulitis may be able to be safely treated without antibiotics, this assumes appropriate selection of patients and an uncomplicated clinical course. Ongoing randomised controlled trials and evidence emerging in this area will provide further guidance. Before practice can change at the level of the general practitioner, further evidence is required to support any changes, and to identify the population group for whom antibiotic treatment is appropriate.
Authors
William McSweeney MD, BMedSci, Intern, Ipswich Hospital, Ipswich, Qld. mcsweenw@gmail.com
Havish Srinath MBBS, BCom-ACST, BAppFin, Surgical Trainee (Registrar), Ipswich Hospital, Ipswich, Qld
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.