Case
AP is a male, aged 20 years, who presents to your practice with chest pains that commenced the preceding night, now exceeding 12 hours in duration.
History taking
Chest pain is a common presenting symptom and the initial clinical assessment is vital in differentiating and triaging the direction of care. Important elements on history are the description of the pain and its associated symptoms. After elaborating on the presenting complaint, the history should focus on the presence of risk factors, such as history of cardiovascular disease, connective tissue or autoimmune diseases, renal impairment, diabetes, hypertension, dyslipidaemia, positive family history of cardiac disease and smoking history. The cardiovascular system is the main focus in patients who present with chest pain, but evaluation of the respiratory system, upper gastrointestinal system and focused musculoskeletal history, looking specifically for trauma in the area of pain, is also required.
Physical examination
Physical examination of a patient who presents with chest pain includes primarily a cardiovascular examination. Blood pressure should be measured in both arms and the patient assessed for presence of:
- acute changes in vital signs, with particular attention to signs of shock (ie diaphoresis, clamminess, tachycardia, decreased blood pressure)
- pulsus paradoxus
- elevated jugular venous pressure (JVP)
- changes in heart or lung sounds
- peripheral oedema.
As with the history taking, respiratory, abdominal and localised musculoskeletal examinations are also likely to be indicated. Common causes of chest pain are shown in Table 1.1
Table 1. Causes of chest pains presenting in general practice, compared with emergency departments1
|
|
Percentage in general practice (%)
|
Percentage in emergency departments (%)
|
|---|
|
Musculoskeletal conditions
|
29
|
7
|
|
Respiratory conditions,
including pneumonia,
pneumothorax and lung cancer
|
20
|
12
|
|
Psychosocial conditions
|
17
|
9
|
|
Serious cardiovascular conditions, including myocardial infarction, unstable angina, pulmonary embolism and heart failure
|
13
|
54
|
|
Gastrointestinal conditions
|
10
|
3
|
|
Stable coronary artery disease
|
8
|
13
|
|
Non-specific causes
|
11
|
15
|
Case continued
AP reports a pleuretic, sharp pain that is localised to his left thorax without any radiation. His breathing feels restricted because of the pain, but he is not overtly short of breath. AP had a terrible night’s sleep as the pain seemed to intensify when he lay flat in bed, so he slept mostly sitting upright in a chair. He has no classical cardiac risk factors and no previous medical illness of significance. AP mentions having a ‘terrible sore throat’ several days ago, but is now on the mend. His clinical examination is largely unremarkable, with stable vital signs (blood pressure: 120/80 mmHg; heart rate: 80 beats per minute; oxygen saturations: 99%) and he is afebrile.
Diagnosis and differentials
AP’s presentation is suggestive of pericarditis, a common condition seen in approximately 5% of chest pain presentations to an emergency department, without evidence of myocardial infarction.2 Typical symptoms include sharp, retrosternal pains (98.3% of cases) that may radiate to the patient’s neck or arm in a similar manner to angina at times.3 Aggravation of the pain with deep inspiration and supine positioning are hallmark features. A pericardial frictional rub is an important, yet uncommon, and often fleeting finding seen only in approximately 35% of cases.3 When present, pericardial frictional rub is a high-pitched scratching or ‘velcro-like’ sound heard most commonly at the left lower sternal border, best in expiration with the patient positioned leaning forward.
The differential diagnoses of AP’s presentation include pulmonary embolus, aortic dissection, pneumothorax, pneumonia and acute myocardial infarction. If the diagnosis remains unclear, the patient must be sent to the emergency department given the gravity of the above-listed differential diagnoses, which if missed, could be fatal. An electrocardiogram (ECG) and blood tests are essential for guiding management of these patients.
Typical viral pericarditis is frequently preceded by a self‑limiting respiratory or gastrointestinal illness. However, particular attention needs to be paid to non-viral pericarditis, such as bacterial pericarditis (often associated with high temperatures), uraemic pericarditis (in patients with comorbid renal failure), tuberculosis pericarditis (in high-risk subgroups), autoimmune pericarditis, and human immunodeficiency virus (HIV) pericarditis. If clinical concern of non-viral pericarditis or HIV pericarditis is present, referral to a cardiologist and other appropriate subspecialists should be made (Table 2).4,5
Case continued
AP’s ECG (Figure 1) shows widespread ST segment elevation and PR segment depression. His blood tests revealed a moderate rise in C-reactive protein (CRP) levels and mild leucocytosis, but were otherwise normal. Specifically, a normal cardiac-specific troponin level was noted. His chest radiograph was also unremarkable.
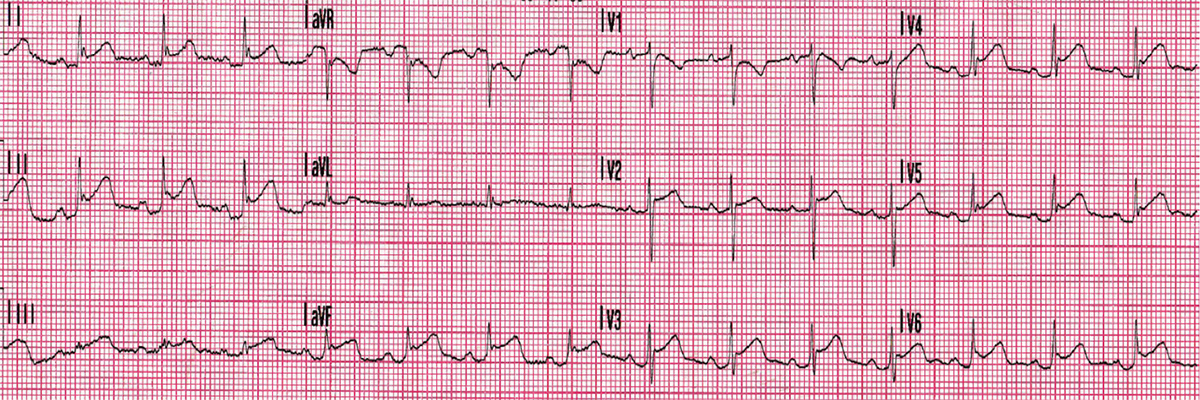
Figure 1. AP’s electrocardiogram
ECG in pericarditis
The ECG in pericarditis is quite typical (Figure 2).6–8 It mainly differs from acute myocardial infarction as the ST segment elevation is not localised to a coronary vascular territory and there is usually absence of reciprocal ST segment depression. This is evident in AP’s ECG (Figure 1). A chest X-ray is done mainly to exclude other important differential diagnoses, such as pneumothorax, or to rule out certain complications of pericarditis, such as large pericardial effusions. A predominantly ‘globular‑shaped’ cardiac silhouette with an increased cardiothoracic ratio >0.5 is a feature of large pericardial effusion on a chest X-ray. Alternative causes of this finding would include dilated cardiomyopathy. It is also important to note that a chest X-ray may appear normal despite the patient having small or moderate-sized effusions. A negative, cardiac-specific troponin level is an important finding. However, an elevated cardiac-specific troponin level may occur in pericarditis, as inflammation of the epicardium without involvement of myocardium can still elevate cardiac-specific troponin levels in approximately 30% of cases.9
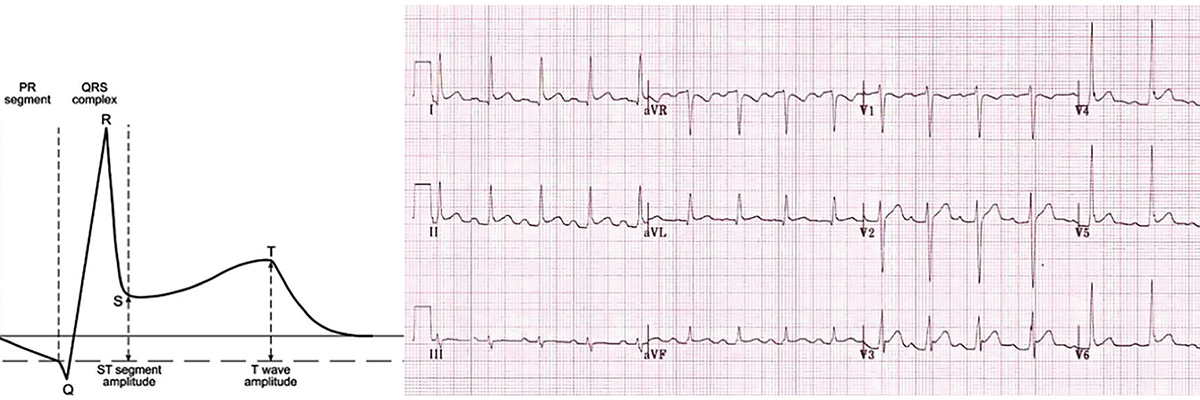
Figure 2. Changes seen on an electrocardiogram from a patient with acute pericarditis
Case continued
AP was diagnosed with viral pericarditis on the basis of the findings described above, and was prescribed ibuprofen 400 mg three times a day with food for one week and colchicine 0.5 mg twice a day for three months. AP was referred for a transthoracic echocardiogram. He was also advised to refrain from strenuous activity until his symptoms had completely resolved. He noted clinical improvement in his symptoms later that night and slept very well in his bed.
Treatment for acute pericarditis
The mainstay of treatment for acute pericarditis is pain relief and resolution of inflammation. When no contraindications exist, nonsteroidal anti-inflammatory drugs (NSAIDs) are recommended. Clinicians should aim to use safer NSAIDs at their lowest effective dose for the shortest duration required.10 The use of a proton pump inhibitor (PPI) is recommended for patients at high risk of gastrointestinal toxicity from NSAIDs. Such patients include those who are over the age 65 years, have a prior history of peptic ulcers, or who are taking concurrent aspirin, corticosteroids or anticoagulants.11
Low-dose colchicine is usually well tolerated and has infrequent side effects, mainly of gastrointestinal nature, although high doses, specifically with prolonged use, can lead to irreversible toxicity. On the basis of large systematic reviews and meta-analyses published between 2012 and 2014, the European Society of Cardiology’s (ESC’s) 2015 Guidelines for the diagnosis and management of pericardial diseases supports the concurrent use of colchicine with NSAIDs to prevent recurrent pericarditis. It is now common practice to use colchicine for the first episode of pericarditis, unless there are specific contraindications.12 Patients should also be counselled on the correct storage of medications to avoid accidental overdoses for medications prescribed for prolonged durations.
The use of glucocorticoids is controversial. The ESC’s 2015 guidelines recommend cautious use of prednisone in patients with pericarditis refractory to NSAIDs, uraemic pericarditis and pericarditis secondary to connective tissue disease. It is recommended that high doses (ie prednisone 1 mg/kg/day) be used, with tapering down over two to four weeks. Concomitant standard therapy with NSAIDs and colchicine with PPI cover is not to be forgotten.12
A simple lifestyle factor such as activity restriction, especially in cases of athletes, is important as well. Refraining from strenuous activity until symptom resolution is recommended for all patients, and for at least three months after resolution of symptoms for competitive athletes.12,13
Case continued
When AP presented for the transthoracic echocardiogram, he seemed diaphoretic, clammy and tachypnoeic. Assessment of his vital signs revealed tachycardia and hypotension. AP had an elevated JVP, difficult-to-hear heart sounds on auscultation and a pulsus paradoxus of 30 mmHg. An ambulance was called to take him the emergency department. A bedside transthoracic echocardiogram was performed in the emergency department and revealed a large circumferential pericardial effusion.
Cardiac tamponade
Pericardial effusion is seen in approximately 60% of acute pericarditis cases, but cardiac tamponade is more uncommon and occurs in approximately 5% of cases.2 Cardiac tamponade occurs when the abnormal accumulation of pericardial fluid creates pressure and causes impairment in diastolic filling of the heart. The development of cardiac tamponade is not dependent on the quantity of fluid accumulated, but rather on the rate of fluid accumulation in the pericardium. A classical clinical feature is ‘Beck’s triad’ – hypotension, elevated JVP and muffled heart sounds. Other features include tachypnoea, tachycardia and atrial arrhythmias, such as atrial fibrillation, Kussmaul sign (a paradoxical rise in JVP on inspiration), positive hepatojugular reflux, weakened peripheral pulses, peripheral oedema and cyanosis.
Pulsus paradoxus is one of the key clinical features of cardiac tamponade, when measured correctly. To measure pulsus paradoxus, the sphygmomanometer cuff is inflated above systolic pressure. Korotkoff sounds are sought over the brachial artery while the cuff is slowly deflated. Initial Korotkoff sounds are heard only intermittently during expiration. The cuff is then deflated slowly to the pressure at which Korotkoff sounds become audible continuously during inspiration and expiration. When the difference between these two levels exceeds 10 mmHg during quiet respiration, pulsus paradoxus is present.14
Electrical alternans is an alternation in the amplitude of QRS complexes. It is thought to be due to the swinging movement of the heart within the pericardial cavity, which creates changes in the vectors measured on surface ECG. However, low-amplitude QRS complexes and tachycardia are more commonly seen on ECGs and should raise suspicion of possible cardiac tamponade.
Case continued
Urgent pericardiocentesis was performed, and about 1 L of fluid was drained. AP improved clinically and was monitored in hospital for the next 48 hours. On repeat transthoracic echocardiograpy, there was only mild re-accumulation of the pericardial effusion. AP was discharged home with plans to repeat the transthoracic echocardiogram in seven to 10 days for monitoring.
Draining pericardial effusions
Moderate-to-large pericardial effusions that result in symptoms should be drained if medical management has failed. Another indication for drainage is for diagnostic purposes, such as evaluation of malignant cells, cytology for tuberculosis or cultures for bacteria. Pericardial effusion can recur and repeat imaging is important to prevent another cardiac tamponade. In the case of recurrence, an alternative diagnosis of the pericardial effusion should be considered (Table 2).15
Table 2. Causes of pericarditis and pericardial effusions4,5
|
Cause
|
Prevalence
|
Investigation
|
|---|
|
Idiopathic
|
Most common
|
Diagnosis of exclusion
|
|
Viral
|
Most common cause of infectious pericardial disease
|
Not routine to perform serological testing. Diagnosis is mainly based on history and examination. Do not forget human immunodeficiency virus in high-risk patients
|
|
Bacterial
|
Uncommon – can occur concurrently with pneumonias
|
Blood cultures and pericardial fluid cultures to identify organisms and direct treatment
|
|
Tuberculosis
|
Uncommon – consider patient demographic and exposure status
|
Chest X-ray, tuberculin testing, Quantiferon Gold, sputum cultures
|
|
Fungal and parasitic
|
Rare in Australia
|
|
|
Autoimmune
|
Uncommon – consider in patients with concurrent rheumatoid arthritis, systemic lupus erythematosus, etc
|
Target testing to likely underlying disease
|
|
Neoplastic
|
Consider in patients with cancer – lung, breast or haematological malignancies are more common
|
Pericardial fluid cytology and pericardial biopsy
|
|
Post-procedural
|
Common after cardiac or thoracic surgery
|
History
|
|
Post-myocardial infarction
|
Delayed presentation post-myocardial infarction, usually by several weeks – more common in large anterior infarcts
|
|
|
Uraemic
|
Suspect in patients with chronic renal impairment, especially peri-dialysis periods
|
Urea and creatinine
|
|
Radiation
|
Consider in patients undergoing chest irradiation
|
|
|
Drugs
|
Rare
|
|
Key points
- Pericarditis is a common condition seen in primary care, with clinical diagnosis largely made through history, physical examination and ECG features.
- All differential diagnoses should be considered and, if the diagnosis is unclear, the patient should be referred to the emergency department.
- In Australia, the most common cause of acute pericarditis is idiopathic or viral with a largely mild and benign course of illness. However, high-risk subgroups should not be overlooked, and a full evaluation of uncommon causes should be completed.
- First-line treatment is a combination of NSAIDs for seven to 10 days and colchicine for three months with a PPI for patients at high risk of gastrointestinal toxicity.
- Development of pericardial effusion is a common complication of acute pericarditis with uncommon but serious consequences when it results in cardiac tamponade.
- Cardiac tamponade is a clinical diagnosis based on Beck’s triad and the finding of pulsus paradoxus on sphygmomanometery. An urgent referral to the emergency department is vital.
Authors
Atifur Rahman MBBS, FRACP, FCANZ, Interventional Cardiologist, Gold Coast University Hospital, Southport; and Griffith University School of Medicine, Qld. atifur@hotmail.com
Avadhesh Saraswat MBBS, Cardiology Advanced Trainee Gold Coast University Hospital, Southport, Qld
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.