In 2009, Binkley and Buehring drew attention to a subgroup of frail, older patients with both osteoporosis and sarcopenia,1 and described these patients as being at higher risk of falls, fractures, disability and frailty. This new syndrome, originally denominated by the authors as sarco-osteopenia, has evolved into the term osteosarcopenia. Since then, the association between osteosarcopenia and poor outcomes in older people has been well documented.2–4 Therefore, identification of this syndrome and implementation of an appropriate care plan for these patients in clinical practice is pivotal.
Osteosarcopenia: A definition
Osteoporosis is usually diagnosed with a bone density scan. According to World Health Organization (WHO) criteria, T-scores of bone mineral density (BMD) below –1 and –2.5 categorise the patient as osteopenic and osteoporotic respectively.5 By contrast, diagnosis of sarcopenia requires a combination of clinical and imaging parameters. The European Working Group on Sarcopenia in Older People (EWGSOP) defines sarcopenia as ‘a syndrome characterised by progressive and generalised loss of skeletal muscle mass and strength, with a risk of adverse outcomes such as physical disability, poor quality of life and high mortality’.6 The working group recommends using low muscle mass – measured by dual-energy X-ray absorptiometry (DXA) or bioelectrical impedance analysis (BIA) – and/or low muscle function/strength for the diagnosis of sarcopenia (Figure 1).
There are no further criteria to define osteosarcopenia, other than a combination of clinical and imaging criteria for low BMD (T-score <–1 standard deviation) and sarcopenia, as defined above. In other terms, osteosarcopenia has been defined as the presence of sarcopenia and osteopenia or osteoporosis.2,3
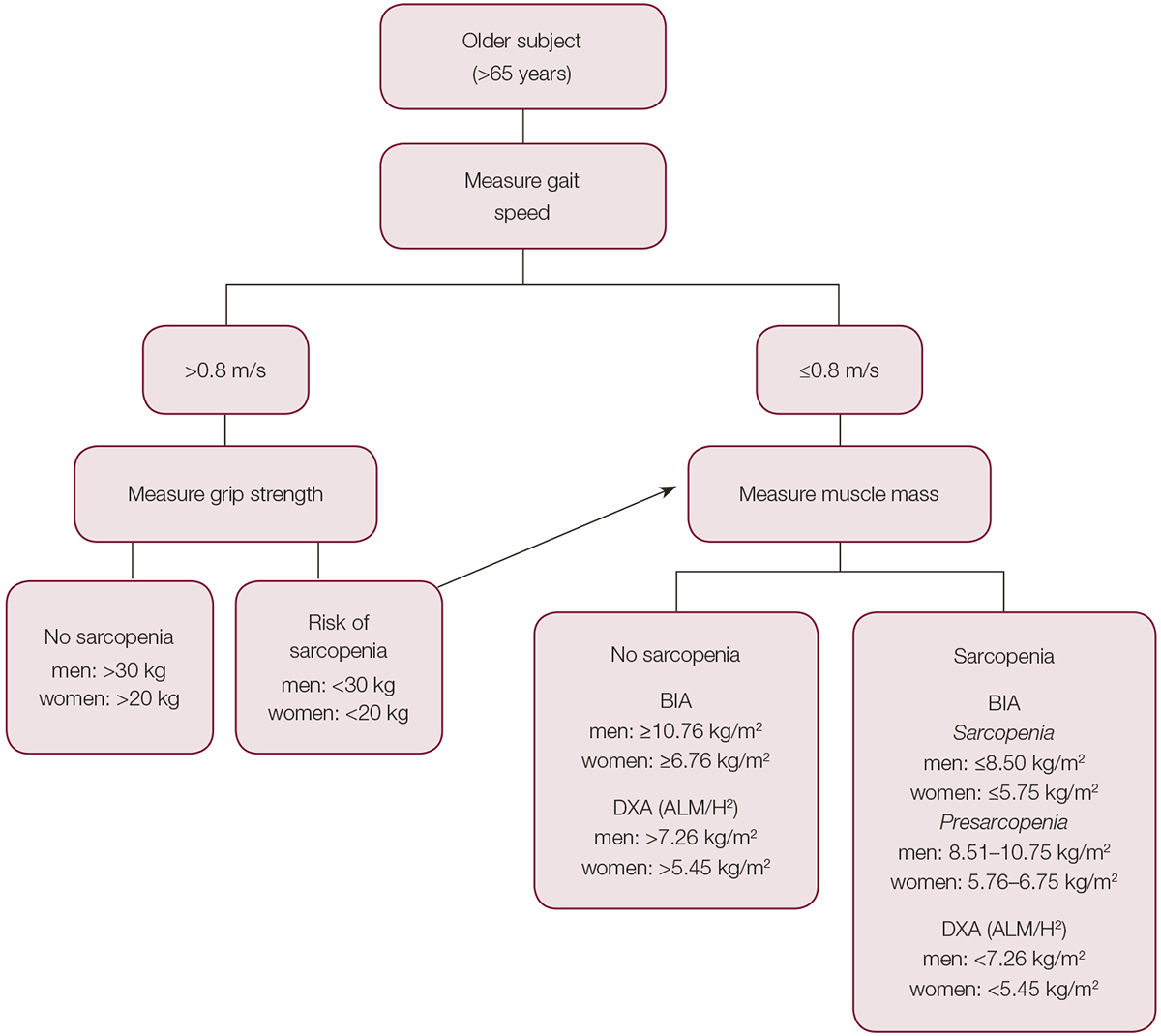
Figure 1. A suggested algorithm for the diagnosis of sarcopenia6,13
ALM/H2, appendicular lean muscle mass/height (derived from DXA whole body exam); BIA, bioelectrical impedance analysis; DXA, dual energy X-ray absorptiometry
Prevalence and importance
An estimated 66% of Australians over 50 years of age reportedly have osteoporosis or osteopenia.7 More than 5.9% of men and 22.8% of women aged 50 years and older, and 12.9% of men and 42.5% of women aged 70 years and older, have osteoporosis.7 In Australia, more than 144,000 osteoporotic fractures occur every year, and the average cost of osteoporosis-associated or osteopenia-associated fractures is estimated at $3.36 billion per year.
The prevalence of sarcopenia in Australians aged 65 years and older is estimated to be up to 6.4% in men and 9.3% in women.8 Patients with sarcopenia are at least three times more likely to have a fall in the next two years.9 Recent studies in Australian persons with previous history of falls reported that 40% of this high-risk population had osteosarcopenia.2,3 Being female; having a history of osteoarthritis, oophorectomy or cancer; and impaired mobility were risk factors for osteosarcopenia in the Australian cohort.3 Regarding poor outcomes, patients with osteosarcopenia have a higher prevalence of disability, falls and fractures (especially if they are obese),10,11 and higher mortality risk.4 Box 1 lists the most common risk factors for osteosarcopenia, which should be identified in clinical practice.
Pathophysiology and pathogenesis
Bone, muscle and associated tissues (eg tendons, ligaments) need weight‑bearing to avoid atrophy, and to gain or regain volume and strength. In addition to acting as an endocrine organ for bone mass maintenance, strong musculature minimises the risk of fractures by sustaining better balance and minimising falls, while also partially absorbing/dissipating forces associated with falls.
In addition, these tissues not only react to endocrine stimulation, they produce hormones that affect the metabolism and activities of the other tissues.12 Bone, muscle and adipose tissues are known to communicate with each other, and help sustain homeostasis through a hormonal and possibly nervous crosstalk. Any alterations in this crosstalk could affect all three tissues simultaneously.13
Furthermore, atrophied muscle and bone are usually replaced by adipose tissue.13,14 Significant fat infiltration into the muscles and bone marrow in patients with osteosarcopenia highlights the possible involvement of lipotoxicity and local inflammation in age-associated osteosarcopenia.13,14 This further complicates the crosstalk between muscle, bone and fat, which are the three most abundant components of the connective tissue.
How to diagnose osteosarcopenia?
A previous history of falls and/or fractures in older people should alert general practitioners (GPs) to the presence of osteosarcopenia. Common clinical signs of osteoporosis include kyphosis and decreased height because of pathological fractures of the vertebrae after middle age. Muscle weakness, falls and decreasing function could indicate sarcopenia. However, in many cases, osteosarcopenia is asymptomatic until a catastrophic fracture occurs, which is the rationale for regular assessment of bone and muscle mass and function in older people with risk factors for this disease (Box 1).
Box 1. Risk factors for osteosarcopenia13,20
|
Osteoporosis
|
|
Maternal history of hip fracture
|
|
Sarcopenia
|
|
Low albumin
Stroke
Hyperlipidaemia
|
|
Osteoporosis and sarcopenia
|
|
Older age
Female
High alcohol intake
Oral glucocorticoids
Menopause (females)
Low protein intake
Low BMI
Current smoking
Low dietary calcium
Low serum vitamin D
Hypogonadism (in men)
Hyperparathyroidism
Obesity
Rheumatoid arthritis
Living in residential aged-care facilities
Chronic kidney disease
Low mobility and function
|
For economic and logistic reasons, the most cost-effective diagnostic method for sarcopenia is DXA, which already has clear indications for diagnosis of osteoporosis in Australia.15 Most DXA machines in Australia include a body composition analysis function. However, GPs should specify this request when referring the patient for a DXA test. This additional analysis could incur an extra charge, which is not covered by Medicare Australia.
Muscle function, however, is measured by estimation of strength and function using a combination of techniques, such as gait speed – which can be easily measured in general practice – and grip strength using a dynamometer, following well established protocols and cut-off values (Figure 1).6 In some instances, people who are frail, older and have poor mobility cannot ambulate or attend a DXA facility. In those cases, BIA might be a useful, low-cost alternative, which can be combined with grip strength to make the diagnosis of sarcopenia. Although less accurate than high-quality BIA machines, but as a very low-cost and accessible alternative, body composition is also included in many commonly available weighing scales that show percentages of fat, muscle and water. Nevertheless, the European Consensus agreed that, even in the absence of imaging or BIA, clinical parameters (gait velocity and grip strength) are reliable enough to diagnose sarcopenia in clinical practice.6
Prevention and treatment recommendations
Regarding primary prevention, no study has looked at interventions with a combined impact on bone and muscle that could be implemented prior to the development of osteosarcopenia. After identification of osteosarcopenia, secondary causes of sarcopenia and osteoporosis should be identified and treated (Box 2). This should be followed by implementation of evidence-based preventive and therapeutic interventions that are effective for osteoporosis and sarcopenia (Table 1).15,16
Box 2. Recommended tests to identify secondary causes of osteosarcopenia21
|
25(OH) vitamin D
Calcium
Parathyroid hormone
Creatinine/estimated glomerular filtration rate
Albumin
Serum testosterone in men
|
Table 1. Preventive and therapeutic interventions for osteosarcopenia15,16,22,23
|
Intervention
|
Recommendation
|
|
Healthy lifestyle
|
Smoking cessation, alcohol restriction
|
|
Physical activity
|
Resistance and balance training at least twice a week for not less than 30 minutes per session
|
|
Vitamin D and calcium
|
Particularly in those with low vitamin D levels (ie <50 ng/mL). The target is to maintain it above 75 ng/ml to assure anti-fall and anti‑fracture efficacy22
Dietary calcium should be encouraged, with a target of 1.2 g/day
|
|
Pharmacological treatment for osteoporosis
|
Should be initiated in all patients with bone mineral density (BMD) T‑score <–2.5 standard deviation (SD) or in patients on corticosteroids (7.5 mg/day for longer than three months and a BMD T‑score <–1.5 SD).15,16 This includes first-line treatments such as bisphosphonates (alendronate, risedronate and zoledronic acid), or RANKL antagonist (denosumab). Teriparatide (bone anabolic) should be considered in high-risk patients who fracture while on anti-resorptives for longer than 12 months, and have a history of a BMD T‑score <–3 SD15
|
|
Protein intake
|
In addition to dietary protein, high-quality protein supplementation (up to 2 g/kg/day in patients with normal renal function and a maximum of 1.2 g/kg/day in patients with renal impairment), especially combined with exercise, consistently improves muscle function and strength23
|
Regarding pharmacological treatment for osteosarcopenia, the effectiveness of osteoporosis drugs in preventing fractures is well documented. By contrast, there is no pharmacological therapy that has been proven to be of benefit in patients with sarcopenia. Angiotensin converting enzyme inhibitors (eg enalapril), which might work by preventing mitochondrial decline and improving endothelial function and muscle metabolism, are still in the experimental phase.17 Anti-myostatin therapies, which target myostatin – a potent inhibitor of skeletal muscle growth – and prevent muscle loss due to ageing have shown limited efficacy;18 however, new modalities of these drugs are under clinical trial and are expected to be available in a few years’ time.
Osteosarcopenia in clinical practice
Osteoporosis and sarcopenia are chronically deteriorating conditions. Therefore, regular follow-up and education of patients are paramount for successful management. Falls and bone metabolic clinics, which are run by geriatricians and endocrinologists respectively, have the limitations of being fragmented models of care that evaluate and treat bone health and sarcopenia separately. Therefore, an important part of the osteosarcopenia follow-up involves referring high-risk patients – those with multiple risk factors for osteoporosis and sarcopenia, or patients who have suffered falls and fractures – to specialised multidisciplinary clinics, such as falls and fractures clinics, which are usually run by geriatricians together with a multidisciplinary team. These specialised clinics, which offer a combined model of bone health and falls prevention, may constitute the future gold standard of care in this population.19 In cases where specialised clinics and services are not available, the patient could still benefit from being assessed by a physiotherapist or exercise physiologist, while also attending community health centres, which are widely available in Australia and often run exercise programs specifically designed for people who are frail and older.
In addition, follow-up with DXA scans is recommended every two years for low-risk patients and once a year for high-risk patients.15 As changes in muscle mass occur more rapidly than changes in BMD, annual evaluation of lean mass by DXA, combined with a regular clinical assessment of muscle strength and function, is recommended.
Discussion and conclusion
Osteosarcopenia is an ever-increasing global health concern. Similarly to most medical conditions, the primary aim should be to prevent the occurrence of osteosarcopenia rather than treat it. Its complex and multifactorial nature requires multifaceted treatment and prevention strategies.
A healthy lifestyle and regular exercise (ie strength, balance) are the first-line prevention and treatment choices for osteosarcopenia; however, although essential, second-line and third-line measures are commonly required. Parallel to pharmacological intervention, patients should receive pragmatic instructions about adjunct therapy and prevention of falls and fractures. In summary, GPs are encouraged to:
- assess for sarcopenia and osteoporosis in older people
- document low bone/muscle mass by DXA and low muscle function/strength
- consider patients with osteosarcopenia to be at much greater risk for falls, fractures, disability and frailty, compared with patients with osteoporosis or sarcopenia alone
- exclude secondary causes
- initiate evidence-based interventions (ie exercise, nutritional supplements, pharmacotherapy)
- refer high-risk patients to specialised clinics, where available.
In conclusion, it is vital to increase the general knowledge about osteosarcopenia among patients and medical professionals, particularly GPs as the sentinels of disease prevention, control, and treatment.
Authors
Ebrahim Bani Hassan DVM, DVSc, PhD, Research Fellow, Australian Institute for Musculoskeletal Science (AIMSS), the University of Melbourne and Western Health, St. Albans, Vic; Department of Medicine, Western Health, the University of Melbourne, St Albans, Vic
Gustavo Duque MD, PhD, FRACP, Geriatrician, Professor and Chair of Medicine, Department of Medicine, Melbourne Medical School and Western Health; Director, Australian Institute for Musculoskeletal Science (AIMSS), St Albans, Vic. gustavo.duque@unimelb.edu.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The authors are grateful to Dr Hossein Kalantar and Dr Aida Karimpour for proofreading this manuscript, and for bringing their GP perspective of its content.