Increasing numbers of people are travelling to places at high altitude. In 2013, more than 100 million people visited altitudes that could lead to altitude illness.1 Since the first scaling of Mount Everest in 1953, the number of trekkers annually in the surrounding Sagarmatha National Park has increased from about 1400 in 1972–73 to more than 20,000 in 2004.2 Each year, more than 20,000 people attempt to climb Mount Kilimanjaro (5895 m) in Tanzania.3 Trekkers are generally well prepared and usually have good support from the companies they trek with; however, recent deaths on Mount Everest remind us of the dangers of altitude illness.
Adventurous travellers are not the only ones at risk; high-altitude cities are becoming popular tourist destinations for travellers of all ages and with varying severity of chronic illness. Although not always recognised by travellers, cities such as Cusco (3400 m), La Paz (3700 m) and Lhasa (3600 m) are at altitudes where altitude illness is likely to develop.
General practitioners (GPs) are still the most frequented source of information for travellers, and are well positioned to help empower travellers to care for themselves overseas.4 The aims of this paper are to understand the conditions that constitute altitude illness, provide guidelines to evaluate the risks of altitude illness, and offer evidence-based advice to prevent travellers from developing altitude illness. The management of altitude illness is not covered, as treatment is usually provided by expedition doctors or clinics at high altitude.
Physiology at altitude
High altitude is used in this article to mean altitudes higher than 2500 m at which a traveller sleeps; significant altitude illness is unlikely below this height. As altitude increases, barometric pressure decreases and, consequently, the amount of oxygen in each breath decreases (Figure 1).5 The decreased oxygen in inspired air in places at high altitude, hypobaric hypoxia, is the central causative factor for the development of altitude illness.6
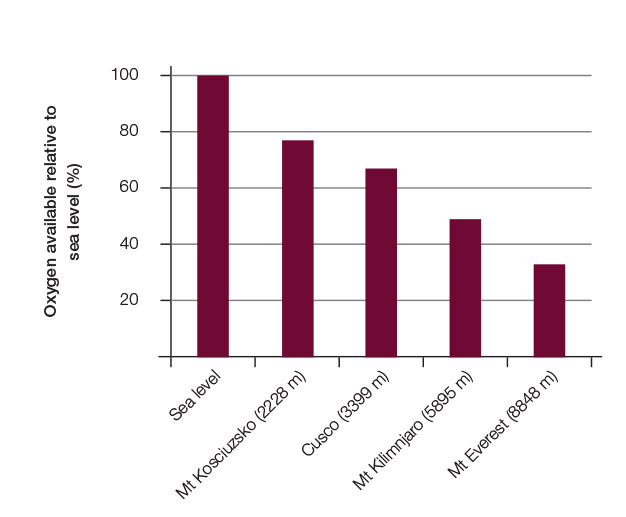
Figure 1. Decreasing oxygen availability due to altitude 5
The body responds (acclimatisation) to low oxygen within minutes of the traveller arriving at a place of high altitude and this process continues for weeks. The important initial changes are:
- hyperventilation
- increased sympathetic tone causing increased heart rate, blood pressure and cardiac output
- vasoconstriction of the pulmonary vasculature, which in the extreme situation is responsible for high-altitude pulmonary oedema (HAPE)
- cerebral vasodilation caused by hypoxia, which can lead to cerebral oedema.
Later changes include:6
- increased erythropoietin secretion, increased haemoglobin production within three days and diuresis, causing increased haematocrit
- decreased muscle mass
- increased vascularity.
Individual and genetic variances exist in this acclimatisation response,7 and inadequate responses lead to the pathological changes of altitude illness. Although the exact pathogenesis remains unclear, increased capillary leakage causing cerebral oedema in acute mountain sickness (AMS) and high-altitude cerebral oedema (HACE),8 and similar pulmonary changes in HAPE,9 have been consistently described. The likely causes for this are hypoxia-induced blood flow and pressure increases, and capillary leakage mediated by chemicals such as bradykinin, nitric oxide, arachidonic acid and vascular endothelial growth factor.6
Clinical conditions found at high altitude
Altitude illness is a collection of different conditions that occur at high altitude: high-altitude headaches (HAH), AMS, HACE, HAPE and other less common conditions such as retinal haemorrhage, high-altitude syncope, cerebral venous thrombosis and cortical blindness. Altitude illness varies in severity from being a nuisance and interfering with a traveller’s holiday (eg HAH and mild AMS), through to more severe AMS, and possibly fatal progression to HACE. HAPE, also potentially fatal, can develop independently of the other conditions in places at high altitude.8 The main manifestations, clinical information, course and management are shown in Table 1.
Table 1. Common conditions occurring at altitude
|
Condition
|
Clinical features
|
Course and management
|
|---|
|
High-altitude headache (HAH)
|
Most common symptom at high altitude
- 25% of travellers at 1920–2956 m35
- up to 90% of unacclimatised people who travel to 5000 m36
Thought to be due to activation of pain fibres in the trigeminal nerve in response to vasodilation, which in turn is caused by the brain’s vulnerability to hypoxia, with some contribution by vascular mediators such as arachidonic acid8
|
HAH settles with oxygen after 10–15 minutes, and resolves with decrease in altitude and a non-steroidal anti-inflammatory drug (NSAID) such as ibuprofen 600 mg three times a day35
|
|
Acute mountain sickness (AMS)
|
Headache after a rise in altitude in the past four days, and at least one of the following symptoms: 10
- gastrointestinal upset (eg anorexia, nausea, vomiting)
- fatigue or weakness
- dizziness or light-headedness
- difficulty sleeping
|
Presents within six to 36 hours of high-altitude exposure, is usually benign and commonly resolves in two to four days with simple rest and ceasing further rise in altitude
Severe AMS is best treated with oxygen and medical care, including dexamethasone, otherwise progression to HACE is possible
|
|
High-altitude cerebral oedema (HACE)
|
Rapidly progressing, life-threatening marked elevation of intracranial pressure and cerebral oedema
Considered a progression from severe AMS, and is usually preceded by a further decrease in oxygenation in a person with severe AMS
- patients with AMS advised not to continue to ascend until symptoms have settled19
|
Usually develops later than AMS, 24–36 hours after arrival at a place of high altitude.
Rare in travellers at altitudes <3500 m,
Affects 0.5–1% of travellers at altitudes >3500 m8,17
Characterised by symptoms of severe AMS and cerebral symptoms, signs of impaired mental state, and the cardinal symptom and signs of ataxia
Rapidly leads to coma and death if untreated
- medical emergency requiring immediate reduction in altitude (300 m or more), oxygen and intravenous dexamethasone
|
|
High-altitude pulmonary oedema (HAPE)
|
Non-cardiogenic form of pulmonary oedema
Occurs 0.5–4% of predisposed previously healthy individuals who ascend higher than 3000 m37
People with HAPE report dyspnoea, cough, decreased exercise tolerance, or chest tightness, and exhibit signs of pulmonary oedema: pulmonary crepitations, tachypnoea, tachycardia or cyanosis
|
Usually commences two to four days after arrival at a place of high altitude, Can develop independently of AMS
Accounts for most of the deaths related to altitude illness38
Urgent treatment by trained medical staff requires rapid descent of about 1000 m, oxygen, and nifedipine with adjunctive drugs
|
Risk of developing altitude illness
Because there is a lack of standardisation in altitude, ascent rate, outcome and populations, the reported prevalence of AMS varies in different studies. AMS has been reported to affect 40% of visitors at high-altitude ski resorts and vacation destinations,10 and up to 80% of people who rapidly reach moderate heights (eg those who fly to La Paz).11 About half of the trekkers who ascend to 5000 m will develop AMS.12 There are no reports of AMS in mainland Australia as the highest peak, Mount Kosciuszko, is only 2228 m; however, cases of AMS have been reported in scientists who have flown to the geographic south pole (2835 m).13
The most important risk factors identified in the literature are how high and how quickly one ascends, and whether travellers previously developed altitude illness.12,14–16 The risk of developing severe AMS, HACE and HAPE is more than 12 times as likely in travellers with a previous history of these conditions.17 AMS is also related to exercise at altitude,18 and one small study suggests the oral contraceptive pill may be associated with an increased risk.13 The incidence of AMS is unrelated to the level of physical fitness, gender, previous altitude experience, load carried, recent respiratory infections, alcohol intake or cigarette smoking.15,16 Box 1 provides information to assist GPs in assessing the risk of altitude illness in travellers. This information is based on guidelines developed by the Wilderness Medical Society.19
Prevention of altitude illness
Slow ascent and allowing ample time for acclimatisation are widely advocated and shown in practice to effectively prevent AMS,10 although the actual rate of ascent recommended varies from 300 to 500 m a day at higher than 3000 m. One meta-analysis reported AMS incidences of 50−75% when ascending more than 500 m a day at higher than 4000 m.20 The Wilderness Medical Society developed the guideline that ascent should not be higher than 500 m a day at altitudes of more than 3000 m, and a day’s rest every three to four days should be included.19 Spending two or more nights at places of high altitude 30 days before ascending has been found to be protective against altitude illness.16 Additionally, resting in the first 48 hours after arriving at places of high altitude is advisable to prevent altitude illness.18
Medication used to prevent altitude illness
Medications are a useful adjunct to prevent altitude illness in travellers who are not able to follow the recommendations for prevention, or who may have had altitude illness before (Table 2).
Table 2. Medications for prevention of altitude illness19
|
Indication
|
Medication
|
Side effects or precautions
|
|---|
|
HAH
|
Ibuprofen 600 mg tds*
|
Fluid retention, hypertension, gastro-oesophageal irritation
|
|
AMS
|
Acetazolamide 125 mg bd
Paediatric dose: 2.5 mg/kg every 12 hours†
|
Paraesthesia (up to 45%), polyuria (2–5%), rash (3%) and dysgeusia (similar to placebo)11
Contraindications include allergies or previous anaphylactic reactions to sulphur drugs,§ pregnancy, significant renal|| and hepatic dysfunction, severe chronic ventilatory limitation
Drug interactions with loop diuretics, topiramate,certain ophthalmic medications39 and possibly the oral contraceptive pill
|
|
HACE
|
Dexamethasone 2 mg every six hours or 4 mg every 12 hours‡
|
Insomnia, unmasking of diabetes, mood disorder and
peptic ulceration with possible gastrointestinal bleeding
Avoid long-term use (>2 weeks) because of Cushingoid’s effects and potential suppression of the adrenal glands with possible crisis if the drug is stopped suddenly
|
|
HAPE
|
Nifedipine, sustained release 30 mg every 12 hours or 20 mg every eight hours
|
Headache, swollen ankles and constipation (AMS-like symptoms) Many significant interactions, especially with drugs that are metabolised via the cytochrome P450 3A4 pathway
|
|
*Also for treatment, including the headache in AMS35
†For children old enough to travel to altitude, refer to section on fitness to travel
‡Not be used for prophylaxis in children
§Risk of cross-sensitivity is low in people with other sulphur allergies (up to 10%), so a supervised trial could be considered prior to travelling39
||Estimated glomerular filtration rate <10 mL/min/1.73 m2
AMS, acute mountain sickness; bd, twice a day; HACE, high-altitude cerebral oedema; HAH, high-altitude headache; HAPE, high-altitude pulmonary oedema; tds, three times a day
|
Acetazolamide
Acetazolamide, commonly prescribed off-label in Australia to prevent AMS, is the only drug currently shown to facilitate acclimatisation.19 Although the exact mechanism remains unclear, it inhibits carbonic anhydrase, an enzyme found in many tissues. Acetazolamide decreases the resorption of bicarbonate in the proximal renal tubule and binds carbon dioxide in the peripheral tissues, resulting in metabolic acidosis. By reducing the metabolic alkalosis of hypocapnia, which normally inhibits the central respiratory drive, hyperventilation can continue for longer. Acetazolamide also acts as a mild diuretic, decreasing oedema. An interesting side effect, not mentioned in Table 2, is decreased effervescence of carbonated beverages because of carbonic anhydrase inhibition in the saliva.
There is difficulty generalising from studies that use two different populations: climbers who are at places of high altitude and going higher, and general travellers who travel from sea level to lesser heights. However, a meta-analysis of 11 randomised control studies concluded that acetazolamide 250 mg daily was strongly associated with a decrease in AMS (combined odds ratio of 0.41; 95% confidence intervals: 0.26, 0.64).11
Dexamethasone
Multiple trials have shown dexamethasone to be of benefit in preventing AMS.20–22 However, unlike acetazolamide, it only masks the symptoms of AMS by reducing inflammation, has significant side effects and, if stopped early, may lead to rebound AMS. The key role of dexamethasone is in the treatment of altitude illness, with prevention being reserved for those who cannot tolerate acetazolamide.
A more recent trial found that a study group using budesonide 200 µg inhaled twice a day had an AMS incidence of 24%, which was significantly different from the placebo group in which the incidence was 60% (P = 0.0006). Budesonide also had fewer side effects than dexamethasone.23 This is promising if future studies support these results.
Nifedipine
Nifedipine 60 mg was shown to prevent HAPE,24 but not decrease AMS,25 and is currently the primary agent used for prevention and treatment for HAPE (Table 2).26 Nifedipine works by inhibiting the hypoxic pulmonary vasoconstriction, thus preventing or relieving pulmonary oedema.
Other medications
Sumatriptan and gabapentin have single studies to support effectiveness, but further research needs to be conducted before these medications can be recommended as prophylaxis for AMS.27 The use of phosphodiesterase inhibitors (eg tadalafil, sildenafil) as adjuncts to prevent and treat HAPE remains debatable.19,28 In a systematic review by Dumont et al, there was no evidence that codeine, aspirin, theophylline, spironolactone and antidiuretic hormone reduced the incidence of altitude illness.20
Natural remedies
Gingko biloba was claimed to have some benefits in preventing AMS; however, the research is inconsistent and conflicting on the association between gingko biloba and AMS.29,30 Consequently, it is not advisable to recommend gingko biloba to prevent AMS. Some have suggested coca tea, offered at hotels in Cusco, as a prevention against AMS; however, there are currently no systematic studies to support these claims.
Box 1. Travellers at risk of altitude illness19
|
Anyone ascending to 2800 m in one day
Anyone with prior history of acute mountain sickness ascending higher than 2800 m
Anyone ascending higher than 500 m/day at altitudes higher than 3000 m
Anyone with a prior history of severe acute mountain sickness, or high-altitude cerebral oedema or pulmonary oedema
|
Fitness to travel to high altitude
With no direct literature to consult, and individual variation and comorbidities, it is difficult to advise about the safety of travel to places at high altitude for people with pre-existing conditions. Generally, people with stable heart conditions, epilepsy and diabetes can safely travel up to 3000 m.31 Contraindications for travel to places at high altitude include severe chronic obstructive airways disease (COAD), unstable asthma, severe ischaemic heart disease, severe or uncontrolled heart failure, pulmonary hypertension and complicated pregnancy.
Relative contraindications include moderate COAD, stable angina, previous cerebrovascular disease, poorly controlled diabetes and recurrent arrhythmias. Risk for deep vein thrombosis is higher in places at high altitude and similar recommendations should be given as those for fitness for flying.
The recommendations for going to places at high altitude after diving is the same as that for air travel: at least 24 hours’ delay after an uncomplicated dive, and at least a week after recompression therapy.32
Women with uncomplicated pregnancies can safely travel up to 2500 m and, similarly to air travel, should do so before 36 weeks’ gestation. Older people without any of the above-mentioned comorbidities have no increased risk of altitude illness. There is minimal information about the incidence of altitude illness in children. One study suggests a higher incidence;33 however, most authorities agree that the incidence of altitude illness is similar to that in adults.34 Diagnosing altitude illness in children is more difficult, and the best advice would be to travel to altitude with children who can adequately communicate symptoms they are experiencing.
Conclusion
As clinicians, we are involved with the care of people who are increasingly entering the challenging environment of high altitude. This article provides scientific information for clinicians to assess the risk and provide information and interventions to prevent altitude illness as part of our role to facilitate a safe journey for our patients.
Author
Ivan Parise, MBBS, DRACOG, Dip Shared Care Psychiatry (eating disorders), Candidate for Master of Public Health and Tropical Medicine. ivan_parise@hotmail.com
Competing interest and funding: None.
Provenance and peer review: Not commissioned, externally peer reviewed.