Since the early 2000s, there has been a worsening epidemic of infectious syphilis among men who have sex with men (MSM) in most high income countries.1 In Victoria, notifications for infectious syphilis rose from 5.5 per 100,000 in 2010 to 15.8 per 100,000 cases in 2015.2 The estimated prevalence of ocular syphilis among all syphilis cases reported in the US was recently found to be 0.6%.3 In this report, we present case descriptions of ocular syphilis cases diagnosed at the Royal Victorian Eye and Ear Hospital (RVEEH) to highlight recent increases in ocular syphilis and its varied manifestations.
Method
A retrospective review of all ocular syphilis cases diagnosed at the RVEEH between January 2015 to August 2016 was undertaken. These cases were identified through a database search for reactive serological tests for syphilis performed by the hospital’s pathology providers, St Vincent’s Pathology and Melbourne Pathology. For patients who might have had syphilis serology performed externally, these tests were repeated on admission to RVEEH as routine to confirm the diagnosis. After the cases were identified, two researchers reviewed the hospital files to extract relevant clinical details and images, using Digital Health Record (Australia) and IFA system software (Germany) respectively. Ethical approval was obtained from the RVEEH’s Human Research and Ethics Committee (reference number 16/1298HS).
All identified cases had infectious syphilis serologically confirmed using a combination of the following tests: Treponema pallidum haemagglutination assay (TPHA), enzyme immunoassay (EIA), rapid plasma reagin (RPR) and the fluorescent treponemal antibody (FTA). Lumbar puncture was performed at the discretion of the treating infectious disease physician. All patients were screened for human immunodeficiency virus (HIV).
Results
Twelve patients (19 eyes) were identified within the study period. The majority (11/12) of the patients were male, with a mean age of 35 years (range: 30–55 years of age). Seven men were identified as MSM and two were diagnosed with HIV at presentation.
The most commonly reported visual complaint was blurred vision, which was reported by 10 patients, followed by floaters, which were reported by nine patients. Redness was not a prominent feature and was only reported in three cases, while only two patients reported eye pain. Eleven patients reported symptoms in one eye; however, on further assessment, seven of the 11 cases had subclinical involvement in the other eye, reducing the number of the unilateral cases to four. Six patients presented acutely, with ocular symptoms of less than a week’s duration. Delayed presentation occurred with three cases, where subacute symptoms of increasing floaters and blurred vision without pain or injection were present for longer than one month prior to presentation. The remaining cases presented between one and four weeks.
With regards to the referral sources, six patients were referred by primary healthcare providers, including general practitioners (GPs) or optometrists. Five patients self-referred to the RVEEH emergency department, and one was referred by an ophthalmologist.
Vision was only mildly affected, with less than two lines of vision loss, in 10/19 eyes. The overall median presenting visual acuity (VA) was 6/9 (interquartile range [IQR]: 6/6, 6/36). However, three men had poor vision, with a VA of less than 6/60; the severity of the visual decline was not related to the duration of the symptoms. Regardless of pre-treatment VA, all 12 patients had excellent visual recovery, with a median post-treatment VA of 6/5 (IQR: 6/5, 6/6) after a mean follow-up period of 12 weeks (standard deviation [SD]: 8 weeks).
On ophthalmic examination at presentation, a wide spectrum of signs (uveitis) was evident. Most pathology involved the retina and optic nerve (posterior uveitis), including:
- posterior placoid chorioretinitis
- retinal arteriolar occlusion
- bilateral optic disc swelling
- punctate inner retinitis.
An iris nodule with anterior uveitis was identified in one case (Figure 1 A–E).
Two patients had genital ulcers at presentation or shortly preceding the ocular diagnosis, probably representing primary syphilis at the time of ocular involvement, with RPR titres ranging from 16 to 128. A further four patients had a rash consistent with secondary syphilis at the time of ocular presentation, with RPR titres ranging from 128 to 512. The remaining six patients were serologically positive for syphilis without recorded concurrent mucocutaneous lesions. We classified these cases as latent syphilis of indeterminate duration, as none had had syphilis serology performed within the preceding two years; therefore, we could not confirm whether they were early cases or not. The RPR titres in these latent cases ranged from 16 to 512.
All patients were treated with intravenous penicillin 2.4 g four times a day as per the local hospital infectious disease department protocol (St Vincent’s Hospital). Seven patients also received high-dose oral prednisolone to prevent an intraocular Jarisch–Herxheimer reaction, based on the degree of intraocular inflammation present at the time of presentation.
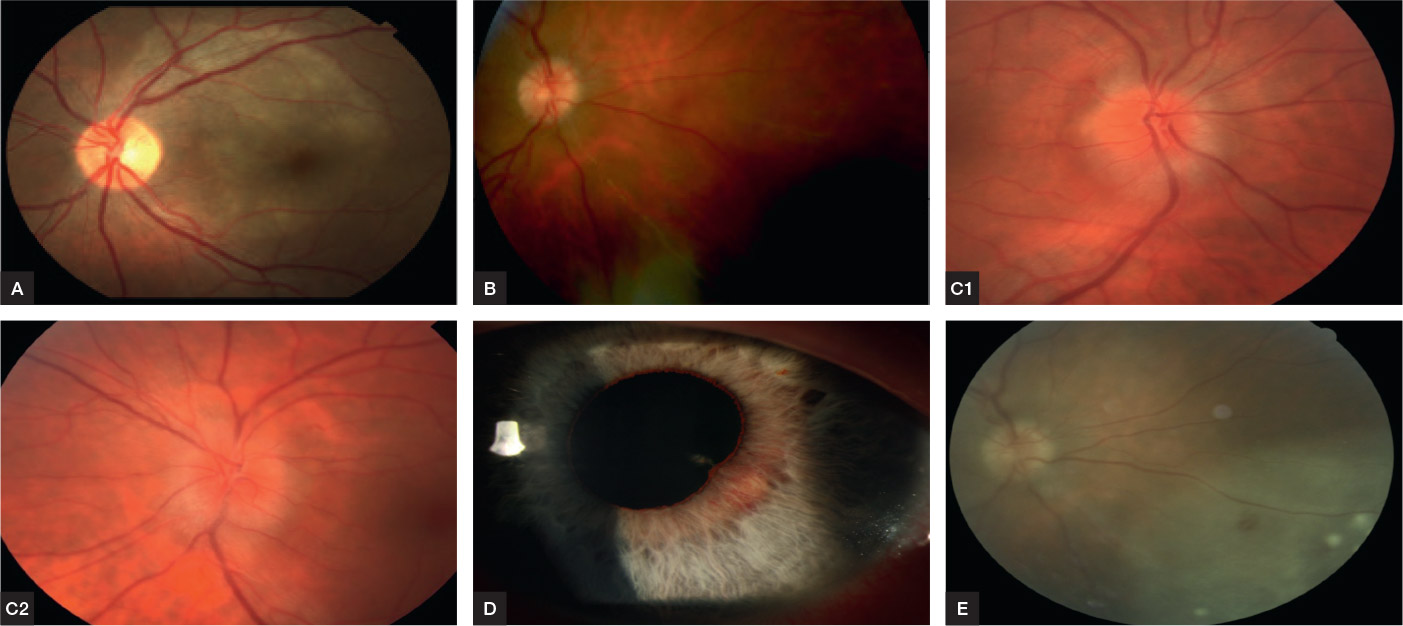
Figure 1. Presentations of ocular syphilis in four individuals
A, posterior placoid chorioretinitis (Case 1); B, arterial sheathing (Case 8); C, bilateral swollen discs (Case 2); D, iris nodules (Case 4); E, syphilitic punctate inner retinitis (case 8)
Discussion
In this article, we described the clinical presentations of a consecutive series of ocular syphilis cases that occurred in the context of a worsening syphilis epidemic in Victoria. Seven patients were referred by GPs or optometrists, which indicates the need for primary care providers to be aware of the possibility of syphilis infection among MSM and the need to consider ocular involvement at presentation. Five other patients self-referred to the specialist hospital. The extrapolation from the results is that in a place where direct access to specialists is not available, the first port of contact would mostly fall on GPs and optometrists.
At least half of the ocular syphilis cases occurred in patients with early syphilis infection, including cases with primary and secondary syphilis. These cases underscore the need for a high level of clinical suspicion for the possibility of ocular infection at the time of syphilis diagnosis, given VA in the affected eyes was often normal on presentation, and other symptoms such as redness or pain often absent.
The most common presenting ocular symptoms were blurred vision and the presence of new-onset floaters. Patients diagnosed with syphilis should be routinely asked about ocular symptoms, particularly if they have had a recent reduction of vision or new ‘spots’ in their vision. A basic ophthalmic examination would include the measurement of their VA (with their spectacles) and an external ocular examination for redness. Patients with any of these clinical ocular features need an urgent referral to an ophthalmologist to confirm the diagnosis of ocular syphilis, with treatment using intravenous penicillin rather than intramuscular benzathine penicillin. Further information about the management of syphilis can be found in the Australian STI management guidelines for use in primary care.4
As syphilis infections are overrepresented among MSM with HIV,5–7 HIV testing should also be performed in MSM who are diagnosed with syphilis, including ocular syphilis. Recent US data from eight jurisdictions found that 93% of ocular syphilis occurred in males, of whom half were HIV-positive.3 A report from the Sydney Eye Hospital of 25 ocular syphilis cases found 23 were in males and eight had HIV, three of whom were new HIV diagnoses.8
Similar to our experience, the Sydney case series reported significant visual improvement after appropriate treatment. It should be noted, however, that although visual prognosis of ocular syphilis is generally good, severe, irreversible vision loss has been reported, mostly due to delays in presentation.9 Furthermore, all of our cases of ocular syphilis that could be staged occurred in people with early syphilis, which is also in line with recent reports from elsewhere.10
One of the strengths of this study is the number of cases collected over a 20-month period from a number of referral sources. This has been possible because the RVEEH is the only specialty ophthalmology hospital in Victoria with a dedicated 24-hour emergency department that accepts referrals and self-presentations. Limitations of the study include its retrospective nature, and its single-centre design that precludes the ability to determine the incidence of ocular syphilis in Victoria.
Table 1 Summary of clinical features of ocular syphilis
|
Case
|
Age (years)
|
Presenting ocular
|
Sex
|
Symptoms of syphilis
|
Pre-
treatment
|
Post-
treatment
|
MSM
|
RPR
|
|---|
|
1
|
45
|
M
|
Blurred central vision
|
Mouth ulcer
|
6/9
|
6/6
|
No
|
16
|
|
2
|
30
|
M
|
Blurred and transient loss of vision
Decrease in colour vision
|
Generalised rash
|
6/4, 6/4
|
6/4, 6/4
|
Yes
|
128
|
|
3
|
55
|
M
|
Blurred central vision
|
Nil
|
3/60, 6/6
|
6/9, 6/9
|
Yes
|
256
|
|
4
|
47
|
M
|
Eye pain
|
Nil
|
6/9
|
6/6
|
NKN
|
16
|
|
5
|
45
|
M
|
Blurred vision
|
Nil
|
6/9, 6/9
|
6/5, 6/5
|
NKN
|
256
|
|
6
|
31
|
M
|
Blurred vision
|
Generalised rash
|
6/5
|
6/5
|
Yes
|
>512
|
|
7
|
45
|
M
|
Floaters, blurry vision
|
Generalised rash
|
6/60, 6/18
|
6/9, 6/6
|
NKN
|
128
|
|
8
|
45
|
M
|
Painful red eye
|
Palmar rash
|
6/9
|
6/5
|
Yes
|
512
|
|
9
|
42
|
M
|
Blurred vision
|
Nil
|
6/12, 6/36
|
6/6, 6/5
|
Yes
|
128
|
|
10
|
41
|
F
|
Central blurred vision, floaters
|
Nil
|
6/60, 6/5
|
6/6, 6/5
|
No
|
256
|
|
11
|
44
|
M
|
Central blurred vision
|
Genital ulcer
|
CF
|
6/9
|
Yes
|
128
|
|
12
|
39
|
M
|
Blurred vision with floaters
|
Genital ulcer
|
6/6, 6/12
|
6/4, 6/4
|
No
|
128
|
|
CF, counting fingers; F, female; M, male; MSM, men who have sex with men; Neg, negative; NKN, not known; RPR, rapid plasma regain
|
Implications for general practice
Although ocular syphilis cases have been reported in Australia previously,5,11 the occurrence of ocular and neurosyphilis in the early stages of syphilis is not widely appreciated. Neurological complications of syphilis have traditionally been considered as being a late manifestation of syphilis. With cases of syphilis continuing to increase among MSM, more cases of ocular syphilis are anticipated. As the symptoms of ocular syphilis are often mild and subacute, patients may initially present to GPs and other primary healthcare providers with other manifestations of their syphilis infection, rather than an eye care professional. Awareness and vigilance is therefore required in the primary care setting to diagnose syphilis cases, and should involve identifying MSM as a particularly high-risk group, in addition to a routine enquiry regarding relevant ocular symptoms that require an urgent ophthalmic referral and intravenous penicillin treatment.
Authors
Daini Ong, MBBS (Hons), BMedSci (Hons),Medical Retina Fellow, Centre for Eye Research Australia; Royal Victorian Eye and Ear Hospital, Vic; Ophthalmology, Department of Surgery, University of Melbourne, Melbourne, Vic. drdainiong@gmail.com
Gaurav Bhardwaj, FRANZCO, PhD, MBBS, Vitreal Retinal Fellow, Royal Victorian Eye and Ear Hospital, Vic
Jason Ong, PhD, MMed (Hons), MBBS, FRACGP, FAChSHM, Postdoctoral Research Fellow, Melbourne Sexual Health Centre, Alfred Health, Vic
Marcus Chen, PhD, FAChSHM, FRACGP, MRCP, MBBS, Sexual Health Physician, Melbourne Sexual Health Centre, Alfred Health, Vic
Lyndell L Lim, FRANZCO, DMedSci, MBBS, Head, Uveitis Unit, Centre for Eye Research Australia; Royal Victorian Eye and Ear Hospital, Vic; Ophthalmology, Department of Surgery, University of Melbourne, Melbourne, Vic
Competing interest: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgement
We would like to thank Miss Lauren Hodgson for her help with formatting the images.