Case
A boy, 12 years of age, was referred to the ophthalmology department in the state capital tertiary-referral paediatric hospital with bilateral vision loss and dull red reflexes. Two weeks earlier, he was diagnosed with type 1 diabetes mellitus (T1DM) after presenting to a regional centre base hospital, 150 km outside the nearest capital city, with a four-day history of lethargy, vomiting, polyuria and polydipsia. He was found to be in diabetic ketoacidosis (DKA), with a pH of 6.8, blood glucose of 37.3 mmol/L and glycated haemoglobin (HbA1c) of 9.2%. He had no significant past medical history, no regular medications and no known allergies, and was discharged after 48 hours on a regimen of insulin aspart 30 units twice daily.
The history of vision loss presented as a mild reduction in vision during his hospital admission, followed by rapid vision loss 10 days after discharge. There was no associated pain, floaters or photopsia. There was no family history of ophthalmic disorders, including cataract. On assessment, visual acuity was count fingers bilaterally and his eyes appeared as in Figure 1.
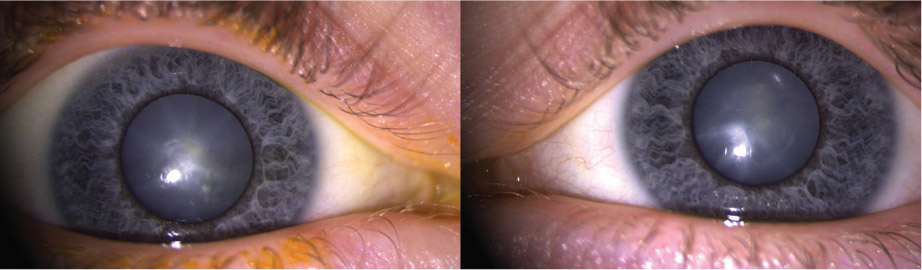
Figure 1. Appearance of the patient’s right and left eyes
A dull red reflex and lens opacification with spoke-like cortical opacities consistent with ‘snowflake cataracts’ is seen
Question 1
What is the most likely diagnosis and recommended management?
Question 2
How common is this diagnosis and what is the aetiology?
Question 3
What are the associated problems and who is at highest risk?
Question 4
What is the prognosis and are there any treatments?
Answer 1
The most likely diagnosis is bilateral, white intumescent cataracts. This child needs urgent assessment by an ophthalmologist as he may need expedited cataract surgery or face potential permanent vision loss.
Answer 2
Cataracts that develop rapidly in young patients shortly after1 or before2 the diagnosis of T1DM are uncommon.1 An incidence rate of 0.7% in the first six months after developing T1DM has been reported in a retrospective cohort study.1 The aetiology is believed to be related to the prompt correction of the hyperglycaemia and DKA.3 Oxidative stress caused by chronic hyperglycaemia is thought to be the pathway of cataractogenesis in these patients.4 A number of mechanisms induce oxidative stress in chronic hyperglycaemia:4
- upregulation of the polyol pathway and subsequent consumption of antioxidants
- increased superoxide production in the mitochondria
- increased advanced glycation end‑products.
The lens is overwhelmed by this oxidative stress and lens proteins are irreversibly damaged, inciting cataract. In keeping with this, the main risk factors for the development of these cataracts appear to be high blood glucose and glycated haemoglobin, and an episode of DKA.1,5
Answer 3
Cataract formation in children can lead to irreversible vision loss because of secondary angle closure glaucoma or sensory deprivation amblyopia. In this case, the patient’s crystalline lenses had enlarged, causing acute secondary angle closure, with a significant rise in intraocular pressure (IOP). This was previously reported in another patient.6 Symptoms and signs of acutely raised IOP include headache, eye pain, vomiting, photophobia, decreased vision, conjunctival injection and corneal oedema.7 Physicians should assess for these symptoms and signs in determining the urgency of referral to a paediatric ophthalmologist. If secondary angle closure glaucoma is present, urgent ophthalmological management is required. Patients with newly diagnosed T1DM, especially those who have had an episode of DKA, should be carefully assessed for the presence of cataract. At particular risk are patients who are non-verbal and unable to report the symptoms of cataract, and children younger than eight years of age who are at risk of amblyopia. A paediatric ophthalmologist should screen these patients.
Answer 4
Once formed, these cataracts can be stationary and have minimal impact on vision, or progress to white cataracts with significant vision loss.1 Ongoing research is assessing whether this process can be arrested prior to irreversible lens protein denaturation and development of white cataracts. Antioxidants, such as vitamin C and aldose reductase inhibitors, have been proposed as potential preventive agents;4 however, to date, there have been no studies to validate their role in prevention.8
Conclusion
After diagnosis, the patient was treated with topical anti-glaucoma medication and cycloplegia. Sequential cataract extraction and intraocular lens implantation surgeries were performed and he had uncomplicated postoperative courses. One week after the second operation, best-corrected visual acuity was 6/6 for distance and N5 for near in both eyes. Posterior segment examinations were normal.

Figure 2. Screening for cataract
The image demonstrates the appearance of a normal red reflex in the right eye and a dull red-reflex in the left eye, similar to that observed in the patient described in our case. Red-reflex testing can be performed by the bedside by use of a direct ophthalmoscope light or pen-torch and enhanced by use of mydriatic agents, such as tropicamide 0.5% before examination. If dull red reflex is observed, prompt referral to an ophthalmologist is indicated.
Key points
- Children diagnosed with T1DM are at risk of developing cataracts, which can potentially lead to irreversible vision loss because of angle closure glaucoma or amblyopia.
- Screening for cataract can be done by the bedside with a direct ophthalmoscope or a penlight (Figure 2).
- Urgent referral to a paediatric ophthalmologist should be made if there are symptoms or signs of raised IOP, if the patient is non-verbal or younger than eight years of age.
- High blood glucose and glycated haemoglobin at diagnosis, or an episode of DKA, increase the risk of developing cataracts.
- As always, it is paramount that patients newly diagnosed with diabetes have regular monitoring for associated ocular complications, including diabetic retinopathy.
Authors
Roderick Francis Justin O’Day, MBBS, LLB, BSc, Ophthalmology Registrar, Royal Victorian Eye and Ear Hospital, East Melbourne, Vic
John Ross Rocke MBBS, BSc, Ophthalmology Registrar, University Hospital Geelong, Department of Ophthalmology, Geelong, Vic
Janaka Tennakoon, MBBS, MD (Paediatrics), DCH, FRACP, Paediatric Consultant, Bendigo Health, Bendigo, Vic
Shivanand Sheth, MS, DOMS, FICO, FAICO, Ophthalmology Consultant, Royal Victorian Eye and Ear Hospital, East Melbourne, Vic
Christolyn Raj, MBBS (Hons), MMed, FRANZCO, Ophthalmology Consultant, Royal Children’s Hospital Melbourne, Parkville, Vic
Competing interest: None.
Provenance and peer review: Not commissioned, externally peer reviewed.