Cardiac imaging
A number of imaging modalities are used by clinicians in the assessment and care of patients with cardiovascular disease. Echocardiography is the first-line cardiac imaging investigation for many cardiac conditions. It is widely available, provides structural and functional information, and reliably reports the required clinical information in the majority of cases. However, the limitations of echocardiography include difficulty obtaining ultrasound images in specific patients and differentiating specific pathologies (eg cardiac infiltration versus hypertrophy). Delineation of the endocardial border can also be challenging with echocardiography when measuring ventricular volumes used to calculate ejection fraction.1 Cardiac computed tomography (CT) and nuclear cardiac perfusion studies are modalities used predominantly in the investigation of ischaemic heart disease.
Cardiac magnetic resonance imaging (CMR) has grown as an imaging modality to provide additive and complementary information to echocardiography.It provides high-quality, cross-sectional images that enable accurate anatomical delineation. It also enables highly reproducible measurement of ventricular volumes and myocardial mass, and quantifies flow across heart valves.1,2 CMR can assess myocardial structure and assist in the diagnosis of cardiac masses. Sophisticated electrocardiogram (ECG) gating and respiratory motion suppression methods are used to ensure the acquisition of high-quality images. CMR can overcome patient-specific limitations, such as obesity, presence of respiratory disease, or presence of soft tissue, lungs and/or scar tissue following cardiac surgery, which can limit the ability to obtain high-quality echocardiographic images.3,4
Advantages and disadvantages of CMR
Box 1 summarises the advantages and disadvantages of CMR.
Box 1. Advantages and disadvantages of CMR compared with imaging modalities
Advantages
- Improved image quality
- No ionising radiation
- Accurate ejection fraction measurement
- Investigation for suspected myocarditis that cannot be confirmed on echocardiography
- Assessment of newly diagnosed cardiomyopathy with diagnostic and prognostic advantages over echocardiography
- Assessment of myocardial viability and perfusion in work-up for coronary artery bypass surgery
- Assessment of congenital heart disease
Disadvantages
- Cost and accessibility
- Contraindicated in patients with metallic implants (eg aneurysm clips, neurostimulators, implanted pacemakers/defibrillators), metal retained fragments in eyes or gunshot injuries
- May be unsuitable for patients with claustrophobia
- A specific cut-off weight for patients varies among individual MRI scanners. Large abdominal and shoulder girths may limit the physical ability of patients to fit in an MRI scanner
- Gadolinium is contraindicated in significant renal disease (eGFR <30 mL/minute)
|
|
CMR, cardiac magnetic resonance imaging; eGFR, estimated glomerular filtration rate; MRI, magnetic resonance imaging
|
There is now an increasing number of cardiac devices that are considered MRI-conditional. Patients in whom these devices have been implanted can have CMR performed with appropriate safety precautions and device checks.5
Techniques in CMR
A number of MRI sequences are used in CMR studies. These are tailored in each individual study for a particular pathology or the assessment of a specific aspect of cardiac function:
- still-frame images that delineate cardiac structures and great vessels in the assessment of congenital heart disease
- high-quality moving images that measure cardiac volumes and myocardial mass, and visualise regional wall motion abnormalities, which may indicate underlying ischaemic heart disease (Figure 1)
- velocity flow imaging that directly measures blood flow in assessment of valvular abnormalities, such as calculation of regurgitant volumes in aortic regurgitation6
- others
- quantification of myocardial iron content: used in patients with beta-thalassemia major, where iron chelation therapy is introduced or intensified to prevent the development of heart failure7
- myocardial fibrosis estimates in cardiomyopathy8
- myocardial oedema detection: indicative of myocarditis or recent myocardial injury.9
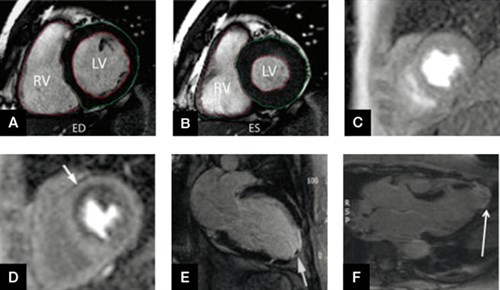
Figure 1. Utility of CMR in ischaemic heart disease and measurement of ventricular volumes on short axis CMR images
A and B. Short axis imaging allowing LV and RV end diastolic, and end systolic volume measurement. C and D. A positive adenosine stress perfusion study with no rest perfusion defect at rest (image C), while the stress image (image D) shows a subendocardial perfusion defect in the anterior and anteroseptal walls (arrowed). This corresponded to a significant left anterior descending (LAD) artery stenosis at coronary angiography. E and F. Detection of LV apical thrombus and transmural late gadolinium enhancement indicative of full thickness apical infarction
CMR, cardiac magnetic resonance imaging; LV, left ventricle; RV, right ventricle
Gadolinium use in CMR
Gadolinium is an intravenous contrast agent used in CMR. It is a useful adjunct in CMR to aid the diagnosis of specific cardiac pathologies. Delayed or late myocardial enhancement imaging (where images are acquired 10–20 minutes after gadolinium administration), allows assessment for specific patterns of uptake (Figure 2).10 Gadolinium is contraindicated in patients with significant renal disease (estimated glomerular filtration rate <30 mL/minute) as it increases the risk of developing the rare, progressive skin condition called nephrogenic systemic fibrosis.11

Figure 2. Patterns of late gadolinium enhancement
A. LGE image showing subendocardial enhancement of the anterior and anteroseptal walls (marked with *)corresponding to a LAD territory myocardial infarction. B. Mid-wall LGE in dilated cardiomyopathy. C. Sub-epicardial LGE in myocarditis or sarcoidosis
LAD, left anterior descending; LGE, late gadolinium enhancement
Pathologies where CMR can be considered
Aortic and valvular disease
CMR visualises the aortic course and precisely measures aortic dimensions. It is advantageous in patients who require repeated interval imaging, avoiding the repeated exposure to ionising radiation that occurs with CT. Aortic coarctation, bicuspid aortic valve disease and aortopathies (eg Marfan syndrome) may result in progressive aortic enlargement and the severity may influence the timing of surgical intervention. Flow velocity–encoded mapping enables more accurate quantification of the severity of valvular lesions.6
Pericardial constriction or pericarditis
Assessment of the pericardium on CMR by measuring pericardial thickness, detection of pericardial inflammation and/or masses, and assessment of pericardial effusion can provide important additive information to echocardiography. Interventricular interdependence (indicative of constrictive physiology) can be detected by visualising movement of the interventricular septum during respiration.12
Cardiomyopathy
CMR is important in the diagnostic work-up and management of newly diagnosed cardiomyopathy because it can accurately measure ejection fraction, calculate myocardial mass, and detect scar tissue, fibrosis and oedema.10
In hypertrophic cardiomyopathy (HCM), CMR-measured septal wall thickness is a prognostic indicator of sudden death. The burden of myocardial fibrosis on CMR is also an emerging marker of risk in HCM. Information obtained through a CMR study in a patient with HCM may directly impact upon the decision for a patient to undergo placement of an implantable cardiac defibrillator (Figure 3).13
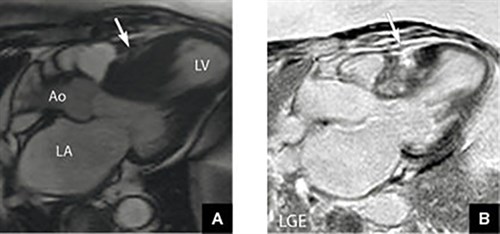
Figure 3. Hypertrophic cardiomyopathy on CMR
A. Significant septal hypertrophy
B. Corresponding patchy mid-wall myocardial fibrosis (indicated by LGE) post-gadolinium administration in a patient with hypertrophic cardiomyopathy
Ao, aorta; CMR, cardiac magnetic resonance imaging; LA, left atrium; LGE, late gadolinium enhancement;LV, left ventricle
Variable patterns of late gadolinium uptake can indicate myocardial infiltration (eg cardiac amyloidosis, sarcoidosis), myocardial scar and viability (in ischaemic heart disease), and myocardial fibrosis (in non-ischaemic cardiomyopathy).10
ARVC is a rare but important cause of sudden cardiac death in athletes and young people.14 It is characterised by ventricular arrhythmias and fibrous or fibro-fatty replacement of the myocardium that typically involves the right ventricle (RV). There are complex diagnostic criteria for the diagnosis of ARVC, which includes cardiac imaging. CMR has significant benefits over echocardiography in the assessment of the right heart in this condition and is therefore the imaging modality of choice, and in the screening of relatives of those diagnosed with ARVC.15
Ischaemic heart disease
CMR is useful in ischaemic heart disease (IHD) in the following settings:
- distinguishing ischaemic versus non-ischaemic aetiology of a newly diagnosed cardiomyopathy16
- detection of complications following myocardial infarction, such as detection of left ventricular (LV) thrombus (when suspected in large left anterior descending artery territory myocardial infarction)
- assessment of myocardial viability prior to potential revascularisation16
- detection of ischaemia: CMR imaging is combined with dobutamine or a vasodilator such as adenosine, which allows the detection of LV wall segments that become ischaemic (with reduced wall motion) with stress or define a myocardium ‘at risk.’17,18
Myocarditis
In suspected myocarditis, CMR is extremely useful. It allows detection of inflammatory hyperaemia, oedema and myocyte necrosis. Clinically, this may have an impact on the decision to perform endomyocardial biopsy or the indication for corticosteroid therapy.9 CMR may identify myocarditis in more than 30% of patients with chest pain, elevated troponin levels and normal coronary arteries. This has important long-term therapeutic implications.19
Congenital heart disease and pulmonary hypertension
The ability of CMR to calculate accurate right ventricular volumes and provide optimal imaging planes for the assessment of RV size has a growing role in assessment, prognostication and for monitoring treatment efficacy in pulmonary arterial hypertension.20 Congenital heart disease encompasses a broad range of cardiac pathologies, and CMR can provide accurate data regarding ventricular size and function, the follow-up of previous surgery, and the assessment and quantification of shunts. CMR overcomes many of the limitations of a transthoracic echocardiogram (TTE) in this setting. Three-dimensional magnetic resonance angiography (3D MRA) provides excellent anatomical assessment of the great vessels, vascular abnormalities and vascular shunts.
Accessibility of CMR
CMR is generally accessed through a cardiologist and it is normal practice for echocardiography to be performed first. In each major Australian city, there are a small number of CMR services that are usually attached to the cardiology department of major public hospitals. A Medicare rebate for CMR can be accessed for congenital heart disease, aortic disease and for the assessment of cardiac masses in Australia.21 When a patient does not meet the Medicare requirements, the individual CMR service may fund the scan or patients may pay an out-of-pocket fee, which may vary between departments. Some private health insurance companies may provide a rebate for inpatient CMR testing.
Future directions
New CMR techniques are constantly undergoing research and validation that includes further development of sequences that characterise myocardial tissue content. Techniques that allow for single acquisition based measurements of ventricular volumes, and evaluation of valvular and aortic disease, may assist in reducing the scan times required for CMR studies.22,23
Conclusion
CMR is primarily used as a complementary tool to other imaging modalities, such as echocardiography, in the investigation and diagnosis of specific cardiac diseases. Current availability of CMR is limited by the expense of the study, a limited number of indications with a Medicare rebate, and the time and resources required for an individual CMR study. However, the number of CMR studies being performed in Australia will inevitably increase with improved MRI techniques, increased clinical utility and wider availability.
Authors
Michael B Stokes MBBS FRACP, Cardiac Imaging Fellow, Department of Cardiology, Royal Adelaide Hospital, North Terrace, Adelaide, SA. mbstokes83@gmail.com
Nitesh Nerlekar MBBS FRACP, Cardiac Imaging Fellow and PhD Student, Monash Heart, Monash Health, Clayton, Vic
Stuart Moir MBBS PhD FRACP, Consultant Cardiologist and Lead of Cardiac MRI, Monash Heart, Monash Health, Clayton, Vic
Karen S Teo MBBS PhD FRACP, Consultant Cardiologist, Department of Cardiology, Royal Adelaide Hospital, North Terrace, Adelaide, SA
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
References