Alcohol is one of the most widely used drugs in Australia. According to the 2013 National Drug Strategy Household Survey (NDSHS), about four out of five Australians aged ≥14 years consumed alcohol in the previous year, and 6.5% did so on a daily basis. Those most likely to drink daily were in the ≥70-year age group; this included both men (21%) and women (10%).1 The Bettering the Evaluation and Care of Health (BEACH) study has measured alcohol consumption by patients over several years, as recorded at general practice encounters, to estimate the proportion of patients who were ‘hazardous drinkers’. Between 2006–07 and 2015–-16, the prevalence of ‘hazardous’ drinking decreased from 27.0% to 22.7% in adult patients.2
However, there is less information about the prevalence of chronic alcohol abuse. One of the questions asked in the same BEACH sub-study was: ‘How often do you have six or more standard drinks on one occasion?’. In the past we have defined six or more standard drinks on a single occasion as ‘binge drinking’.3 One could consider those who drink six or more standard drinks ‘daily or almost daily’ to have ‘chronic excessive alcohol consumption’.
The first aim of this study was to estimate the prevalence of chronic excessive alcohol consumption among adult patients, as recorded at general practice encounters, by patient characteristics. In 2008, the New South Wales Department of Health published the Drug and alcohol withdrawal clinical practice guidelines.4 The recommended treatments for alcohol withdrawal were pharmacotherapies, including diazepam, thiamine (vitamin B1), naltrexone, acamprosate, disulfiram; counselling; advice about self-help groups; and referral to allied health services. The second aim of the study was to estimate the management rates of diagnosed chronic alcohol abuse in general practice by patient characteristics and compare them with the prevalence of chronic excessive alcohol consumption. The third aim was to examine whether general practice management of diagnosed chronic alcohol abuse matched the guidelines.
Method
We examined data from April 2010 to March 2015 from the BEACH study. BEACH is a continuous study of Australian general practice, the methods of which are described in detail elsewhere.5
We used a sub-study of BEACH to measure the prevalence of chronic excessive alcohol consumption among patients at general practice encounters. The sub-study asked 40% of adult (≥18 years) BEACH patients: ‘How often do you have six or more standard drinks on one occasion?’. Those who responded with ‘Daily’ or ‘Almost daily’ were considered to have chronic excessive alcohol consumption.
We used all adult (≥18 years) general practice encounters in the BEACH data to examine the management of diagnosed chronic alcohol abuse, which was defined as International Classification of Primary Care, 2nd edition, (ICPC-2) code ‘P15’.6 Some patients may appear in both samples.
The patient characteristics of interest were age, sex, Aboriginal and Torres Strait Islander status, and non–English speaking background. The patients’ postcodes were used to assign them to ‘Advantaged’ or ‘Disadvantaged’ groups on the basis of the Socio-Economic Indexes for Areas (SEIFA; 1–5 for ‘Disadvantaged’, 5–10 for ‘Advantaged’).7
BEACH is approved by the University of Sydney’s Human Research Ethics Committee (ref: 2012/130).
Results
Prevalence
From April 2010 to March 2015, 161,513 adult patients gave details of their alcohol consumption. Of these, 2303 (1.4%; 95% confidence interval [CI]: 1.4–1.5) recorded drinking six or more standard drinks daily or almost daily. Men were five times more likely to report chronic excessive alcohol consumption (2.4%; 95% CI: 2.7–3.0) than women (0.5%; 95% CI: 0.5–0.6). The prevalence of chronic excessive alcohol consumption among patients aged 45–64 years (2.3%) was significantly higher than in all other age groups (Figure 1). Patients who identified as Aboriginal and/or Torres Strait Islander peoples were more than twice as likely to report chronic excessive alcohol consumption (3.7%; 95% CI: 2.7–4.7) than non-Indigenous patients (1.4%; 95% CI: 1.3–1.5). Patients from an English-speaking background were significantly more likely (1.5%; 95% CI: 1.4–1.6) than those from a non–English speaking background (0.4%; 95% CI: 0.3–0.5) to report chronic excessive alcohol consumption. Patients from disadvantaged areas were significantly more likely to report chronic excessive alcohol consumption (1.7%; 95% CI: 1.6–1.8) than those from advantaged areas (1.3%; 95% CI: 1.2–1.4; Figure 1).
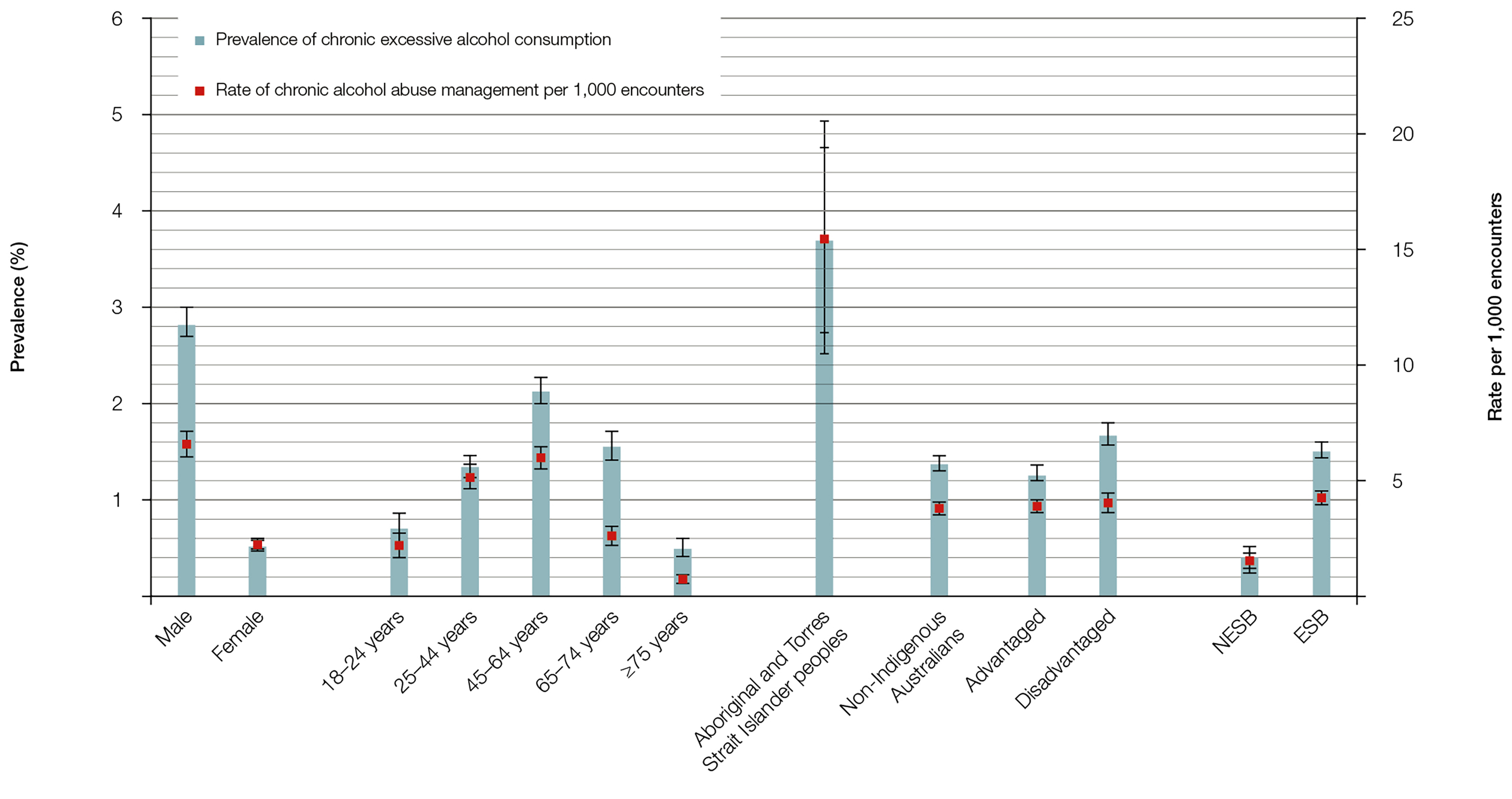
Figure 1. Patient characteristic – Specific prevalence of chronic excessive alcohol consumption among an adult subsample and management rate of chronic alcohol abuse at all BEACH adult encounters 2010–15 (95% confidence intervals)
ESB, English-speaking background; NESB, non–English speaking background
Treatment
Over the same period, in a sample of 418,438 adult patient encounters, diagnosed chronic alcohol abuse was managed at 1658 encounters, an average of 4.0 times per 1000 encounters. The management rate at encounters with men was significantly higher than at those with women (6.6 versus 2.3 per 1000 encounters). Patients aged 25–64 years had a significantly higher management rate than those aged 18–24 years and ≥65 years. Diagnosed chronic alcohol abuse was managed at about four times the rate at encounters with Aboriginal and Torres Strait Islander patients than at those with non-Indigenous patients (15.6 versus 3.8 per 1000 encounters). Management rates were significantly higher at encounters with patients from an English-speaking background than at those with a non–English speaking background (4.3 versus 1.4 per 1000 encounters). There was no significant difference in the rate of management between advantaged and disadvantaged patients (Figure 1).
Medications were recorded at a rate of 37 per 100 diagnosed chronic alcohol problems managed (about half the rate of all medications recorded at BEACH encounters). The most common medications were diazepam (31.8%), acamprosate (16.0%), vitamin B1 (14.9%) and naltrexone (10.6%). Clinical treatments, mainly counselling, were provided at the high rate of 63.5 per 100 chronic alcohol abuse problems. Specialist referral rates were low, but referrals to allied health professionals were provided at more than three times the BEACH average (11.4 versus 3.1 per 100 problems), and were mainly to drug and alcohol services. Pathology tests were ordered at significantly higher than average rates, with liver function tests and full blood counts the most common (Table 1).
Table 1. Management actions used per 100 chronic alcohol abuse management occasions (2010–15)
|
Management actions
|
Rate per 100 chronic alcohol abuse management occasions (95% CIs)
|
Rate per 100 problems managed in BEACH
overall (for comparison)
|
|---|
|
Medication
|
37.6 (34.0–41.2)
|
65.0 (64.4–65.5)
|
|
Diazepam
|
12.0 (10.3–13.7)
|
–
|
|
Acamprosate calcium
|
6.0 (4.8–7.3)
|
–
|
|
Vitamin B1
|
5.6 (4.4–6.8)
|
–
|
|
Naltrexone
|
4.0 (2.9–5.1)
|
–
|
|
Clinical treatments
|
63.5 (60.3–66.7)
|
23.8 (23.3–24.3)
|
|
Referral
|
14.2 (12.2–16.2)
|
10.1 (9.9–10.2)
|
|
Allied health professionals
|
11.4 (9.7–13.2)
|
3.2 (3.1–3.3)
|
|
Pathology tests
|
45.1 (39.2–51.0)
|
32.1 (31.6–32.6)
|
|
Liver function
|
10.2 (8.7–11.8)
|
–
|
|
Full blood count
|
8.7 (7.3–10.0)
|
–
|
Discussion
We found that in some demographic groups – men, patients aged 45–64 years, Aboriginal and Torres Strait Islander patients, and those from disadvantaged socioeconomic areas – the prevalence of chronic excessive alcohol consumption was higher than among their counterparts. While the pattern of treatment for demographic groups mostly followed prevalence in the groups, it was interesting to note that some patients – female, younger, those who identify as Aboriginal and Torres Strait Islander, advantaged, or from a non–English speaking background – had higher management rates of chronic alcohol abuse relative to their prevalence of chronic excessive alcohol consumption. However, we should be cautious when interpreting this comparison. The main limitation to this study is that those who had chronic excessive alcohol consumption are not necessarily the same patients managed for chronic alcohol abuse. There would be many patients who would be diagnosed with chronic alcohol abuse who do not drink six or more standard drinks per day.
Treatments recorded for chronic alcohol abuse problems were consistent with the New South Wales Department of Health’s Drug and alcohol withdrawal clinical practice guidelines.4 There were high rates of general practitioner (GP) counselling and referrals to drug and alcohol services. Low medication rates, which included diazepam and vitamin B1, followed the guidelines. The ordering rates for liver function tests showed GPs were monitoring the effects of alcohol abuse on the health of their patients. GPs are presumably ordering full blood counts to detect raised mean corpuscular volume, a marker of chronic high alcohol consumption.
GPs are in a prime position to identify and manage patients with chronic alcohol abuse as 85% of Australians see a GP at least once a year.5 Our study suggests that when GPs manage chronic alcohol abuse, they do so appropriately. Further study examining the management rate of chronic alcohol abuse among at-risk groups, such as socioeconomically disadvantaged patients, is required.
Authors
Christopher Harrison BPsych (Hons), MSocHlth, Senior Research Analyst, Menzies Centre of Health Policy and the Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW. christopher.harrison@sydney.edu.au
Janice Charles BA, MSc (Med), Senior Research Officer, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Graeme C Miller MBBS, PhD, FRACGP, Medical Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Helena Britt BA, PhD, Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During its final year of data collection, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, Seqirus (Australia) Pty Ltd, Sanofi-Aventis Australia Pty Ltd and the Australian Government Department of Veterans’ Affairs. Funding organisations had no editorial control over any aspect of this article.