Promoting and maintaining the health of Aboriginal and Torres Strait Islander women is integral to ‘close the gap’ between Aboriginal and Torres Strait Islander and non-Indigenous Australians.1 Aboriginal and Torres Strait Islander women have higher fertility rates, compared with other Australian women,2 yet they experience a greater burden of illness. The increased prevalence of conditions, such as cardiovascular disease, type 2 diabetes mellitus and cervical cancer, attribute to higher mortality and morbidity rates.3 This disparity in health is perpetuated in the perinatal period because of low rates of antenatal attendance,4–6 continuing harmful substance use,7,8 a high prevalence of maternal medical complications,9 poor maternal nutrition10,11 and mood disorders.12 Maternal health problems are further compounded by higher parity,7 a greater number of teenage mothers,2 and short pregnancy intervals from delayed contraception uptake in the postpartum period.4,13
The health outcomes of Aboriginal and Torres Strait Islander women can be improved through increased engagement with health services during the perinatal period. Postnatal care, in particular, supports maternal health needs by reinforcing preventive healthcare, such as cervical screening and lifestyle advice, providing contraception, reviewing social and emotional wellbeing and following up any problems identified during the antenatal period.
However, data specifically reporting on postnatal care in Australia is sparse. One study that looked at perinatal care provided by Aboriginal and Torres Strait Islander primary health centres in regional Australia showed that just over half of the women presented for postnatal care.6 The aim of this paper was to identify predictors for postnatal attendance by Aboriginal and Torres Strait Islander women who attend an Aboriginal and Torres Strait Islander community-controlled health service.
Method
A retrospective cohort study was conducted through the Mums and Babies Program14 at the Townsville Aboriginal and Islander Health Service (TAIHS). Eligible women were identified through a medical record search as those who attended the service for any antenatal care for a singleton pregnancy during the period of 1 January 2009 to 1 January 2011, inclusive. Participants were excluded for early pregnancy loss (<20 weeks gestation) or twin pregnancy during the study period. Other reasons for exclusion are outlined in Figure 1.
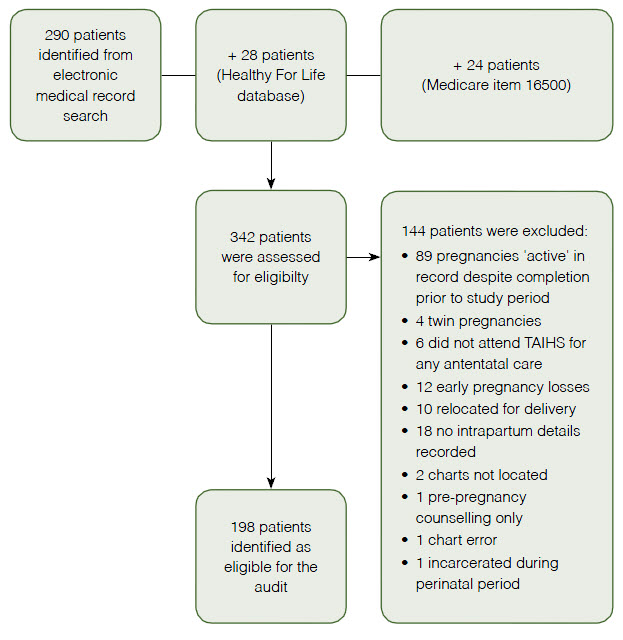 |
| Figure 1. Participant selection |
Various demographic, behavioural, antenatal, intrapartum and postnatal factors were reviewed. Adequate antenatal care was defined as more than four antenatal visits, consistent with key performance indicators for Aboriginal and Torres Strait Islander health services.15 Specific findings regarding teenage pregnancies (women aged <20 years) and grand-multiparity (>5) were reported. Participants were considered to have returned for postnatal care if they attended TAIHS within 3 months postpartum.
Inter-coder reliability was checked on a random sample of 20% of the study population and the majority of variables had high correlation (>90%).
Data analysis was stratified by women who returned to TAIHS for postnatal care and women who had no record of attending postnatal care with any service. Data were analysed using univariate descriptive measures, Pearson’s chi-square tests, Student t-tests (with two samples, assuming unequal variance) and Mann-Whitney U (two-tailed) tests. Fisher’s exact test was used if less than five cases were found in any cell. Multivariate logistic regression analysis was performed on variables significant at a bivariate level to determine independent predictors for postnatal attendance. A P value of <0.05 was considered statistically significant.
Approval was granted by the Royal Australian College of General Practitioners National Research and Evaluation Ethics Committee (NREEC 12-004) and the TAIHS Board of Directors.
Results
From the initial search, 342 patients were identified and 198 were identified as eligible (Figure 1). The mean age of eligible participants was 24.7 years (SD, 18.3–31.2). The majority smoked cigarettes (62.8%) and nearly two-fifths consumed alcohol (36.6%). Nearly two-thirds (65.5%) of eligible women were overdue for a Papanicolaou (Pap) smear at their first antenatal visit.
Median parity for participants was 1.5 (interquartile range [IQR] 0–3). One-third of women were nulliparous (31.8%) and 15.2% (30/198) of women were grand-multiparous. The median number of antenatal visits for participants was 4.5 (IQR 2–7); half attended ≤4 visits. 17.2% of women attended their first antenatal visit at 24 weeks gestation or later.
Ninety-five women (48.0%) attended TAIHS in the postpartum period, 13 attended another health service and 90 (45.5%) did not have any record of postnatal attendance. The women who returned to TAIHS were seen at a median time of 3 weeks (IQR 1–6) postpartum. After multivariate adjustment, the number of antenatal visits attended was found to be a statistically significant independent predictor of postnatal attendance (â = 0.05, t(180) = 3.46, P < 0.001).
Table 1 compares the demographic, behavioural and perinatal details for women who attended TAIHS in the postnatal period (TAIHS-PNC group) with those who were not recorded as attending any postnatal care (no-PNC group). The TAIHS-PNC group was older than the no-PNC group (mean age 25.9 years [SD, 18.8–33.1], compared with 23.8 years [SD, 18.1–29.3], P = 0.02). Both groups had similar ethnicity representation, location of residence, parity and substance use.
The TAIHS-PNC group attended the service for a median number of seven antenatal visits (IQR 4–9), compared with three visits (IQR 2–5) in the no-PNC group (P <0.001). The TAIHS-PNC group was also more likely to present early in pregnancy for antenatal care, (9 weeks [IQR 5–18], compared with 13.5 weeks [IQR 7–22], P = 0.04). There were similar modes of delivery and perinatal outcomes for both groups.
Table 1. Demographic and perinatal characteristics as related to postnatal attendance
|
|
|
TAIHS-PNC group‡
(n = 95)
|
No-PNC group‡
(n = 90)
|
P value§,||
|
|---|
|
Mean (SD) age, years
Aged <20 years
|
25.9 (18.8–33.1)
20 (21.1% CI: 12.8%–29.2%)
|
23.8 (18.1–29.3)
27 (30.0% CI: 20.5%–39.5%)
|
0.02¶
0.16
|
|
Indigenous status
|
|
Aboriginal
Aboriginal and Torres Strait Islander
Torres Strait Islander
|
70 (73.7% CI: 64.8–82.6%)
8 (8.4% CI: 2.8–14.0%)
17 (17.9% CI: 10.2–25.6%)
|
70 (77.8% CI: 69.2–86.4%)
6 (6.7% CI: 1.1–10.9%)
14 (15.6% CI: 8.1–23.1%)
|
0.80
|
|
Resident of Townsville
Inner suburb*
|
95 (100%)
68 (71.6% CI: 62.5–80.7%)
|
90 (100%)
57 (63.3% CI: 53.3–73.3%)
|
–
0.23
|
|
Tobacco use
|
55/87 (63.2% CI: 53.1–73.3%)
|
51/80 (63.8% CI: 53.3–74.3%)
|
0.94
|
|
Alcohol use
|
26/78 (33.3% CI: 22.8–43.8%)
|
30/74 (40.5% CI: 29.3–51.7%)
|
0.36
|
|
Pap smear overdue
|
46/70 (65.7% CI: 54.6–76.8%)
|
27/39 (69.2% CI: 54.7–83.7%)
|
0.71
|
|
Median parity (IQR)
Parity 0
Parity 1–4
Parity ≥5
|
2 (0–4)
26 (27.4% CI: 18.4–36.4%)
52 (54.7% CI: 44.7–64.7%)
17 (17.9% CI: 10.2–25.6%)
|
1.5 (0–3)
32 (35.6% CI: 25.7–45.5%)
45 (50.0% CI: 39.7–60.3%)
13 (14.4% CI: 7.1–21.7%)
|
0.40**
0.47
|
|
Median number of antenatal visits (IQR)
|
7 (4–9)
|
3 (2–5)
|
<0.001**
|
|
Median gestation at first visit, weeks (IQR)
|
9 (5–18)
|
13.5 (7–22)
|
0.04**
|
|
Quality of antenatal care
|
|
≤4 antenatal visits
Gestation ≥24 weeks at first visit
|
33 (34.7% CI: 25.1–44.3%)
11 (11.6% CI: 5.2–18.0%)
|
58 (64.4% CI: 54.5–74.3%)
18 (20.0% CI: 11.7–28.3%)
|
<0.001
0.12
|
|
Normal vaginal delivery
|
|
Mode of delivery
Elective caesarean delivery
Complicated delivery†
|
68 (71.6% CI: 62.5–80.7%)
9 (9.5% CI: 3.6–15.4%)
18 (19.0% CI: 11.1–26.9%)
|
70 (77.8% CI: 69.2–86.4%)
7 (7.8% CI: 2.3–13.3%)
13 (14.4% CI: 7.1–24.7%)
|
0.62
|
|
Perinatal outcome
|
|
Preterm (<37 weeks)
Low birth weight (<2500 g)
Mean birth weight, grams (IQR)
Perinatal deaths (PMR)
Admission to neonatal special care unit
|
14 (14.7% CI: 7.6–21.8%)
12 (12.6% CI: 5.9–19.3%)
3182 (3021–3342)
3/95 (32/1000)
15/61 (24.6% CI: 13.8–35.4%)
|
9 (10.0% CI: 3.8–16.2%)
9 (10.0% CI: 3.8–16.2%)
3185 (3043–3326)
1/90 (11/1000)
19/70 (27.1% CI: 16.7–37.5%)
|
0.33
0.57
0.98¶
0.62††
0.74
|
|
IQR, interquartile range; PMR, perinatal mortality rate (number of deaths per 1000 live births), SD, standard deviation; No-PNC, no postnatal care; TAIHS-PNC,
TAIHS-postnatal care
*Suburb within 10 km of service; †emergency caesarean delivery or instrumental delivery; ‡data represented as number (%, 95% confidence intervals) unless otherwise stated; §P <0.05 statistically significant; IIPearson’s chi-square performed unless otherwise stated; ¶Student’s t-test performed; **Mann-Whitney U test performed; ††Fisher exact test performed
|
Discussion
Postnatal care presents an opportunity to review and reinforce maternal health needs in addition to those of the newborn, a service of particular value for Aboriginal and Torres Strait Islander women. However, a low rate of postnatal attendance (48%) was noted for the women in our study. This is similar to previous research, which showed about half (53%) of women who attended antenatal care at Aboriginal and Torres Strait Islander health services returned for postnatal care.6 We found increased antenatal attendance to be a statistically significant independent predictor of postnatal attendance (P <0.001). Early presentation for antenatal care (P = 0.04) was also found to have a significant association with postnatal attendance.
Inadequate antenatal attendance has been a historical issue for Aboriginal and Torres Strait Islander women in Australia and rates of low attendance range from 19% to 43%.4–7 This is still reflected in our study (50%). Although improvements to neonatal outcomes have been shown by increasing antenatal attendance,14,16,17 the effects on maternal health have not been extensively explored.
This study identified a number of maternal health issues that would benefit from ongoing follow-up. We found high rates of smoking (62.8%) and alcohol use (36.6%) during pregnancy, consistent with national figures. Half of Aboriginal and Torres Strait Islander women in Australia smoke during pregnancy, compared with 15% of all women.7 For women who do achieve reduction or complete cessation of smoking during pregnancy there is still a significant risk of resumed use in the postpartum period.18
Alcohol use during pregnancy has been reported by one-fifth of Aboriginal and Torres Strait Islander women across Australia.8 The use of alcohol in the postpartum period has yet to be studied.
The majority of women in our study were also overdue for cervical screening. There is a low participation rate for Aboriginal and Torres Strait Islander women in the national cervical screening program.19 This has led to the increased incidence of cervical cancer and associated mortality when compared with other Australian women.19 There is a paucity of data reporting cervical screening participation rates for women specifically in the perinatal period. Anecdotally, however, many women defer Pap smears until the postpartum period. Appreciating the preconception and antenatal health status of Aboriginal and Torres Strait Islander women, it is essential to be able to provide appropriate follow-up after delivery.
Successful antenatal programs have found that Aboriginal and Torres Strait Islander women are more likely to engage with health services that provide culturally appropriate, holistic, community-based care.14,16 Our study suggests that strategies proven effective for antenatal attendance will also improve postnatal follow-up. However, it will be important to investigate community perceptions regarding postnatal care, in addition to specific enablers and barriers to attendance.
Limitations
This study relied on data extraction from an electronic medical record system. Medical record documentation can vary, particularly in a service that experiences a high turnover of staff. Historically, there was no standardised approach to recording antenatal and postnatal care and this has influenced the inter-coder reliability for some of the variables. Although the Mums and Babies Program has protocols in place for follow-up of its clients beyond delivery, we cannot be confident that the women who did not have a record of postnatal attendance did not access care elsewhere.
Implications for general practice
- Low rates of postnatal attendance have been reported for Aboriginal and Torres Strait Islander women, presenting a missed opportunity to deliver preventive healthcare.
- High rates of smoking and alcohol use during pregnancy, as well as low participation rates for cervical screening, are examples of issues to review for Aboriginal and Torres Strait Islander women in the postpartum period.
- By improving antenatal attendance rates for Aboriginal and Torres Strait Islander women, it is expected postnatal attendance will indirectly improve.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We are grateful to the Aboriginal and Torres Strait Islander women who attend TAIHS for their antenatal and postnatal care needs and who continue to support our initiatives that aim to improve the quality of service delivery to the community. We would like to thank the TAIHS Board of Directors for their support for the project, in addition to the staff members who assisted with its implementation. We would also like to thank Dawn Charteris and Dr Sarah Lythgoe for their guidance and feedback.
The study was funded by TAIHS and General Practice Education and Training Limited (GPET) through the first author's Advanced Rural Skills Training in Aboriginal and Torres Strait Islander Health.