Case 1
A man aged 65 years, who had a past history of three malignant melanomas, returned to the dermatologist for melanoma surveillance. He reported no new lesions of concern. On careful inspection of a tattoo on his left deltoid, a pale pink papule was identified (Figure 1).
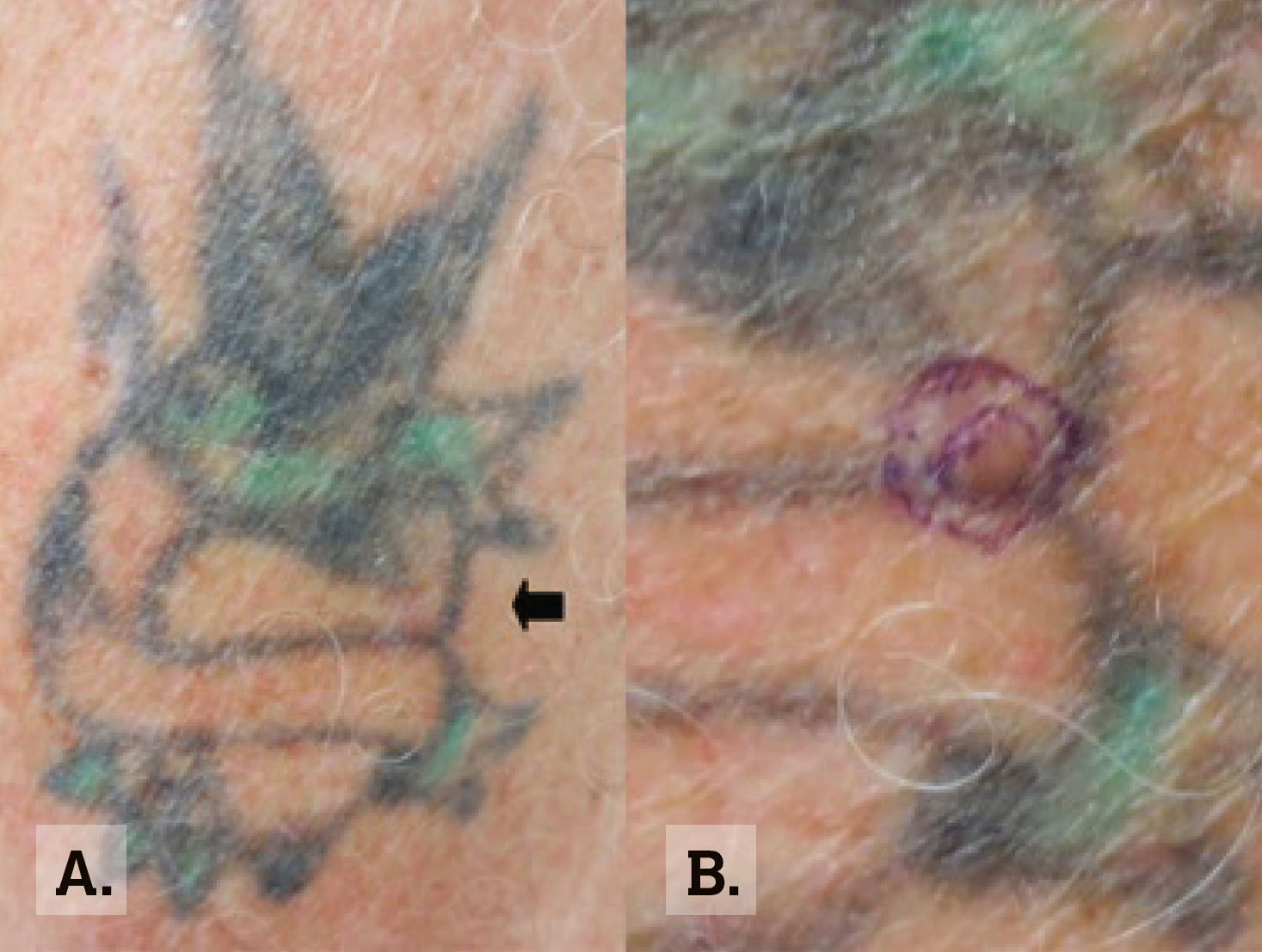 |
Figure 1. Tattoo in Case 1
A. Macroscopic image of tattoo on left deltoid.
B. Lesion marked on closer macroscopic view. |
Case 2
A man aged 55 years, who had a history of multiple non-melanoma skin cancers, presented to the dermatologist for a routine full skin examination. He reported no new lesions of concern. He had large extensive tattoos on both lower limbs (Figure 2). On examination he had a keratotic lesion on the right medial lower leg within the tattoo (Figure 2).
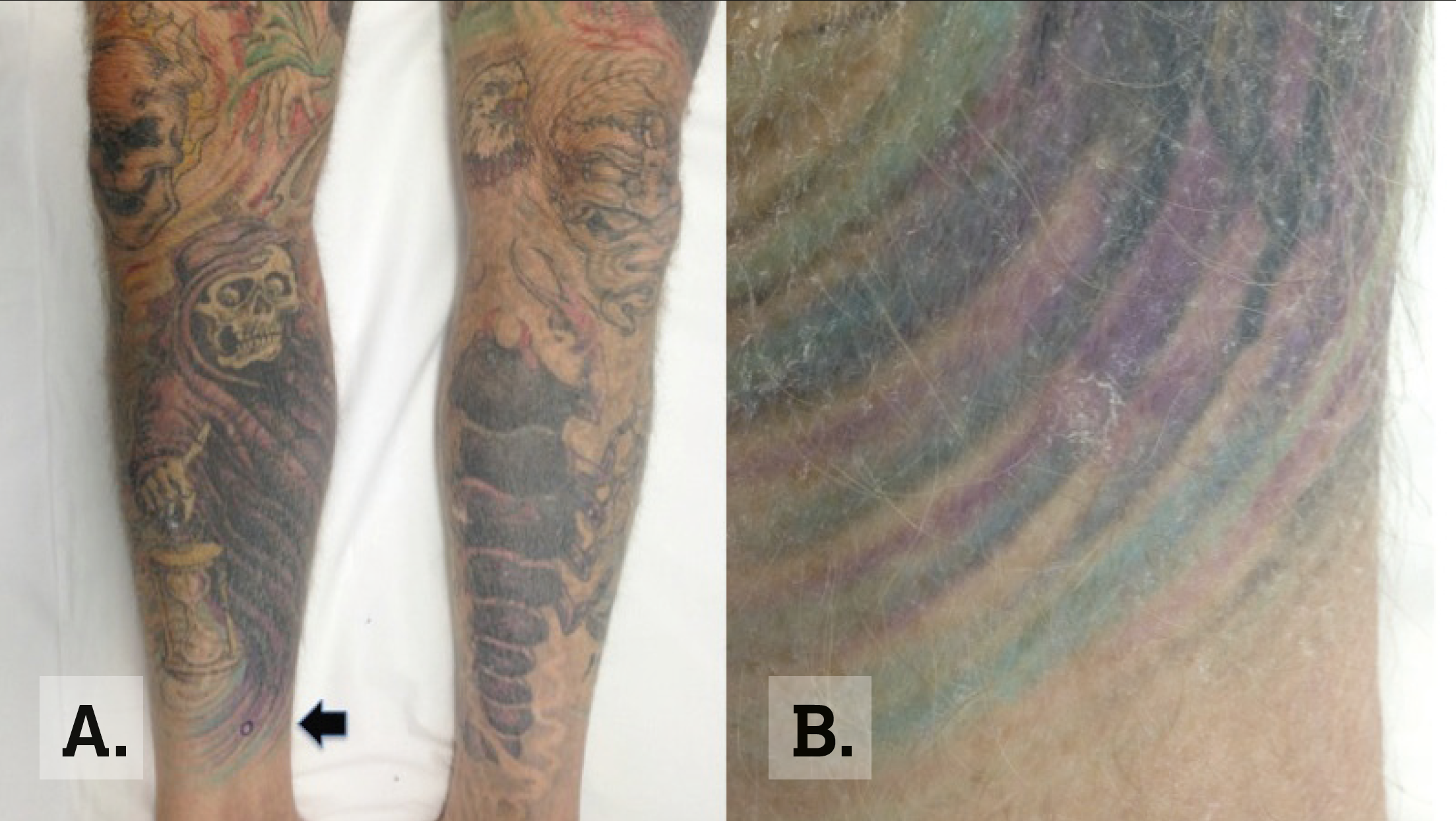 |
Figure 2. Case 2 tattoo
A. Macroscopic image on lower limbs.
B. Close view of keratotic lesion. As if designed to deliver our warning against skin cancer, this grim reaper points a finger in the direction of the patient’s lesion. |
Question 1
What are the diagnoses for Cases 1 and 2?
Question 2
Are skin cancers a complication of tattoos?
Question 3
What is the prevalence of tattoos in Australia?
Question 4
What difficulties are faced in skin cancer detection within tattoos?
Question 5
What are the implications for future practice?
Answer 1
Clinically, Case 1 appears to be a basal cell carcinoma and the histopathology confirmed a multifocal superficial and nodular basal cell carcinoma. Case 2 clinically appears to be a keratoacanthoma, which was confirmed by histopathology.
Answer 2
There are reports of neoplastic changes in tattoos;1–5 however, tattoos are not an established risk factor for melanoma.1,2,6 The literature in the English language reports 16 cases of malignant melanoma developing in tattoos.6 Basal cell carcinoma and squamous cell carcinoma are other neoplastic lesions that have been reported in association with tattoos.4,5 There are also anecdotal, isolated cases of cutaneous lymphoma, dermatofibrosarcoma protuberans and leiomyosarcoma.4
Answer 3
The number of people with tattoos has been increasing worldwide in response to demands of fashion and style. Tattoo prevalence in Australia has increased from 10% in 1998 to 15% in 2004–2005.7 Approximately one in seven Australians has a tattoo. They are most popular in the 20–39-year age group.7 Tattoo designs range from small, single symbols to larger more extensive designs. As tattoo popularity is increasing, there has also been an increased interest in sleeve tattoos, which cover the length of a limb;8 however, no published reports regarding sleeve tattoo epidemiology have been found to date.
Answer 4
Tattoo ink may camouflage the clinical signs of skin cancer. Subtle changes can be disguised within a tattoo, as seen in Cases 1 and 2. Assessment of pigmented and non-pigmented lesions within a tattoo is difficult for patients on a macroscopic level, for health practitioners at a clinical and dermoscopic level, and for histopathologists at a microscopic level.4,5,9,10
Detection by patients and their friends may be delayed if the lesion is masked by a tattoo. For health practitioners, macroscopic assessment can be challenging. For examples, the ugly duckling sign is a mole that appears to be different from all others on the body but may become less visible when moles are surrounded by tattoos. This is of particular importance in high-risk patients with a history of melanoma or dysplastic naevus syndrome. This risk is magnified by the presence of extensive sleeve tattoos. Skin surveillance may additionally be influenced by the tattoo ink colour, and, possibly, detection is more difficult with dark coloured, compared with light coloured, tattoos. Dermoscopy assessment is also interrupted as the tattoo ink and its colour may mask some of the signs for interpretation. All of these issues cause diagnostic difficulties and increase the risk of delayed diagnosis of cutaneous malignancy, potentially resulting in poorer patient outcomes.4,6
Answer 5
It is imperative to address any risk factor contributing to delayed diagnosis or misdiagnosis of non-melanoma skin cancers and melanomas. This is of vital importance in Australia, where the incidence of skin cancer is the highest in the world.11 This risk is magnified by the increasing prevalence of tattoos, their popularity in the cohort least likely to adopt sun protection behaviour,12 and a reported higher prevalence of sunburn.13 Health practitioners face challenges now and in the future, for surveillance and diagnosis of skin cancers within tattoos. Awareness of these diagnostic difficulties and subsequent outcomes needs to be communicated to the public, the tattoo community and health practitioners. It is recommended, for safety reasons, that the tattoo pigment should not be placed on pigmented lesions,14 and skin photography prior to tattoo may aid future skin surveillance. If there is concern about a lesion within a tattoo, the lesion should be closely monitored and/or skin biopsy performed.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.