An increasingly robust body of evidence supports the effectiveness of active transport – walking, cycling or use of public transport – in reducing non-communicable diseases (NCDs). Regular active transport is associated with clinically significant risk reductions in obesity, diabetes, hypertension, cardiovascular disease and all-cause mortality.1–3 Furthermore, it is likely that the benefits of regular active transport outweigh risks, including exposure to traffic collisions and air pollution at the population level;4,5 however, this relationship is likely to be geographically dependent and more evidence is needed in the Australian context.
Recent years have seen significant growth in programs and policies to encourage active transport. Taking Melbourne, Victoria, as an example, active transport interventions have ranged from aspirational targets, including aims to increase cycling to 25% of all commuter trips by 2020, through to the construction of high-quality cycling and walking infrastructure, urban planning policies that promote mixed-use walkable neighbourhoods, and social marketing campaigns.6–9
Very little is known about how general practitioners (GPs) can contribute to active transport. A 2009 randomised controlled trial conducted in primary care found that obese middle-aged women who were randomised to commuter cycling, GP counselling and provision of a bicycle were more likely to continue cycling at 18 months, compared with controls.10 An article published in 2012 reported that GPs saw poorly built environments as a barrier to their patients who were obese taking up more walking.11 A 2014 article put forward an agenda for clinicians to better understand the impact of travel behaviour on their patients’ health.12
The reasons for an individual choosing to take up active transport are complex, but may represent interactions between environmental, socioeconomic, cultural, policy and health factors on the individual’s lived experience. In this sense, for this article, we conceptualised active transport as a complex adaptive system with the patient and GP at the centre of the system, their attitudes and behaviours around active transport being influenced by socioecological determinants. In this model, feedback systems and interactions within and between subsystems have the potential to create behaviour change (Figure 1). We aimed to explore GPs’ views around promoting active transport to gain a better understanding of GPs’ perceived barriers and facilitators in the clinical context.
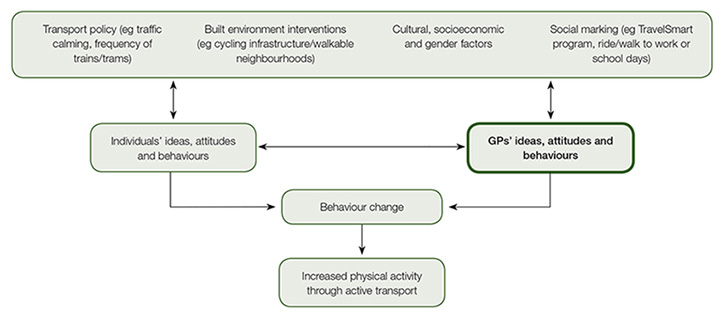
Figure 1. A conceptual model of active transport as a complex system
Methods
Sample, recruitment and variables
We recruited GPs through the Victorian Primary Health Research Network13 and informal professional networks. We aimed to maximise our sample with respect to participant age, gender, socioeconomic variability of practice neighbourhoods, practice location (ie inner metro, outer metro or regional) and the quality of the built environment around practice neighbourhoods. We used the Australian Bureau of Statistics (ABS) Socioeconomic Index for Areas (SEIFA) – Relative Socioeconomic Advantage and Disadvantage (ISRAD) indicator to model relative levels of advantage and disadvantage in practice neighbourhoods.14 We used a walkability index as a proxy for the quality of the built environment.15 Practices were classified as inner metro, outer metro or regional on the basis of the above measure. We had no explicit exclusion criteria. Recruitment and interviews were conducted between April and September 2016.
Interviews
All GPs who were approached agreed to participate in the study and provided consent in keeping with the University of Melbourne’s requirements. Telephone and in-person interviews were conducted by CP and audio-recorded for analysis (Appendix 1; available online only). Our interview schedule was informed by the socioecological model.16
Data analysis
We performed an inductive framework analysis17 while being sensitive to identifying novel themes in the data lying outside the framework. Data were coded in NVivo11 by CP and random samples double coded for consistency by JF.
Ethical approval was obtained from the Human Ethics Advisory Group, Department of General Practice, at the University of Melbourne (approval number: 1646442.1).
Results
Descriptive analysis
We conducted 10 semi-structured interviews with five male and five female GPs. The mean GP age was 52 years (range: 30–74 years of age). Mean interview length was 41 minutes (range: 21–52 minutes). The mean SEFIA percentile of the suburbs in our sample was 51.8 (range: 1–100). The mean walkability score was 5 (range: 1–10). Four GPs practised in inner metropolitan Melbourne locations, four in outer metropolitan locations and two in regional areas of Victoria. Two GPs worked in Aboriginal community controlled health organisations (ACCHOs), one worked with culturally and linguistically diverse (CALD) patients and one GP worked with homeless patients (Table 1).
Table 1: Participant characteristics
|
Participant
|
Gender
|
Practice type
|
Walkability (1 = low to 10 = high)
|
Age (years)
|
SEIFA percentile (1 = low to 100 = high
|
|---|
|
A
|
F
|
Outer metro
|
1
|
38
|
87
|
|
B
|
F
|
Inner metro
|
10
|
30
|
89
|
|
C
|
F
|
Outer metro
|
2
|
54
|
41
|
|
D
|
M
|
Inner metro
|
5
|
50
|
100
|
|
E
|
F
|
Regional
|
No data
|
57
|
8
|
|
F
|
M
|
Outer metro
|
6
|
55
|
70
|
|
G
|
F
|
Inner metro/CALD
|
10
|
56
|
75
|
|
H
|
M
|
Outer metro/ACCHO
|
4
|
62
|
6
|
|
I
|
M
|
Inner metro
|
4
|
74
|
41
|
|
J
|
M
|
Regional/ACCHO
|
No data
|
45
|
1
|
|
ACCHO, Aboriginal community controlled health organisation; CALD, culturally and linguistically diverse
|
Most GPs in the study met the recommended level of physical activity (30 minutes of moderate intensity physical activity) on most days. The majority of participants commuted to work by car, but a number cycled and walked recreationally and occasionally for commuting. It is possible that these factors would have influenced GPs’ perspectives.
Three themes emerged from the interviews: active transport as a form of incidental activity; building active transport capacity in general practice; and the social and built environment.
Theme 1. Active transport as a form of incidental activity
Participants were not familiar with terminology around active transport (ie promoting transport-related physical activity). As one participant suggested:
Active transport is something that is newer and I’d be interested to see if you asked GPs what they would think of the word active transport and how it would pertain to what they do. You might get a bit of a mixed response just maybe saying well what do you mean by that? – GP D, inner metro
Despite this, participants had considerable experience in promoting active transport while not naming it as such. Participants recounted scenarios where they counselled patients on walking to the shops rather than taking the car, or getting off the tram one or two stops earlier on their daily commute:
They might get in the car and go down on a regular basis to get their newspaper. Well, I just suggest if it’s within a 20-minute walk or a half an hour walk, to consider doing that by foot and leaving the car in the garage. – GP I, inner metro
Participants framed these activities as incidental activity, which was a more familiar concept to them. They saw benefits in promoting incidental activity as it could be incorporated into a patient’s day-to-day life. Participants saw this as a way to gently and sustainably incorporate exercise into a daily routine. As one of the participants stated:
I think it’s a way of getting maybe some less motivated, some patients who maybe don’t have the time or the motivation to do other forms of exercise, getting them active. – GP B, inner metro
When discussing incidental activity with patients, participants were less likely to think or talk about cycling and public transport. However, they did share concerns around cycling and safety. These included concerns about potential traffic collisions and protecting personal safety:
There’s concerns around road safety [and lack of], bike lanes, bike paths. So safety as a road user, but also safety if you are isolated on a back street or something feeling vulnerable. – GP A, outer metro
Participants felt that conversations around active transport would fit best into consultations relating to preventive health, management of cardiovascular risk factors and mental health presentations.
Participants framed active transport benefits in terms of health benefits to the individual. When asked about benefits, few participants cited wider community and environmental benefits of active transport (eg reduced carbon emissions, traffic congestion, noise and air pollution).
Theme 2. Building active transport capacity in general practice
Participants felt that active transport was not ‘on the radar’ of most GPs. When asked why, most of them felt that this was an emerging area that had not yet made its way into clinical practice. Similarly, participants had limited knowledge of the policy landscape around active transport, including community programs designed to promote active transport.
Participants discussed a number of strategies to promote active transport and have it included in the general practice agenda. GPs felt that The Royal Australian College of General Practitioners (RACGP) could have a policy statement around active transport, and that active transport evidence could be incorporated into relevant clinical practice guidelines as they become updated:
I think the College, RACGP, is a good body to encourage GPs to do that. I think [promoting active transport is] as important as offering other educational activities or suggestions that they do from time to time, so I think they should be involved. – GP I, inner metro
Participants also felt that more sophisticated interventions could be helpful. These ranged from developing educational materials for GPs, such as a learning module on the gplearning portal on the RACGP website, through to the provision of clinical handouts and waiting room materials that link evidence around active transport, availability of local infrastructure and community programs in patients’ minds.
Participants also felt that clinical trials could be useful in evaluating interventions, and that general practice could collaborate with Primary Health Networks (PHNs) and, in some cases, ACCHOs to deliver key parts of interventions.
Participants identified two factors that could be barriers to their involvement in active transport, both of which are well documented in the existing physical activity literature. The first relates to individual GPs’ interest in their own preventive health. Participants felt that doctors who are more physically active themselves would be more likely to model those values, including activities such as active transport to their patients:
One of my old colleagues used to ride to work and I had a patient of hers the other day saying how admirable she was because she always rode to work, so I do wonder if it is something that patients kinda notice about their doctors. – GP B, inner metro
The second barrier related to time pressure. Participants stressed that this was not a problem unique to active transport:
I think time is an issue and I think we’re constrained by the fact that we often only have time to do the bare essentials – what the point of presentation is then explanation about immediate treatment. I think time probably stands in the way of or has stood in the way so far of doing a lot on lifestyle modification. – GP C, outer metro
Theme 3. The social and built environment
Participants understood that there were a number of factors in their patients’ worlds that could act as barriers or facilitators to taking up active transport. At the most basic level, GPs felt that chronic diseases, including musculoskeletal conditions, cardiovascular diseases, obesity and mental illness, would deter their patients:
I find it a bit hard to imagine instructing the first case, the older 60 year old guy with mental illness and cardiovascular disease, because I can’t really envisage his home situation and what it actually would entail for him to walk somewhere, ride somewhere or take public transport. – GP A, outer metro
Participants also felt that socioeconomic disadvantage could act as a barrier. Those working with patients in high-rise public housing had particular concerns around crime and how the built environments in these spaces affect perceptions of personal safety:
People have got concerns about personal safety around the area. So if you were say in winter, and you’re suggesting someone might - if they do go to work, walk home from work or something like that. Well it’s dark and they don’t necessarily feel safe walking in the dark. – GP G, inner metro/CALD
Similarly, participants felt that for some Aboriginal and Torres Strait Islander patients experiencing socioeconomic disadvantage, the strains disadvantage places on finances, housing and relationships could act more broadly as a barrier to active transport:
It’s hard for people to take on something else that they’re being told that they have to do, that they just don’t have the space to do. Thinking in terms of health literacy, it’s not really that people don’t understand that it may be good for their health but it’s more they don’t have the headspace to organise to commit to something like that regularly. They’re often bouncing from crisis to crisis. – GP H, outer metro/Aboriginal health
Finally, cultural norms in patients’ communities were strongly identified as barriers and facilitators. Our participants thought patients would be more open to active transport if it were something their friends, family and community were already doing. In understanding the factors that shape cultural norms, participants acknowledged this was likely to reflect a complex interplay around not only the location of the community in relation to jobs and services, but also access to appropriate active transport infrastructure and less tangible factors, including the values of communities towards factors such as liveability, air and noise pollution, congestion, as well as ethnicity and socioeconomic factors:
Some cultures in Europe where people largely commute by active transport, you know it’d just be more the done thing. Whereas over here, it’s certainly in the outer metropolitan area where I am, it’s a little bit anticultural, or counter-cultural to be recommending that. It is a harder conversation or idea to give, compared to somewhere, like I could imagine in Amsterdam or in Copenhagen or even in Brunswick or Carlton, where everyone would know people that commute by bike or are walking distance to their school and work. – GP A, outer metro
Discussion
To our knowledge, this is the first study to explore GPs’ ideas around promoting active transport. We found that concepts around active transport relate well to GPs’ existing understanding of incidental physical activity. GPs provided a number of practical strategies to add active transport to the general practice agenda, including through policy statements, clinical practice guidelines and the development of multicomponent interventions. The intimate knowledge participants had about their patients’ lives led them to consider the impact of social and environmental factors on their patients’ likelihood to engage with active transport, an insight that would make GPs well suited to contributing to wider policy discussions around this topic.
Study limitations
We aimed to minimise selection bias through our maximal variation sample. However, because most participants had an existing relationship with the university and a majority met the Australian physical activity guidelines themselves, bias may be possible. Because of the small sample size and qualitative nature of this study we must be careful about making generalisations, particularly in contexts outside of Victoria, Australia. Finally, the socioecological model allowed us to illuminate social and environmental factors but, inevitably, detracted from other lenses, such as gender and the policymaking process.
Links with existing literature
If we position GPs as a trusted source of health information in our proposed complex adaptive system, it is feasible that if GPs are encouraged to broaden their understanding of incidental activity to incorporate ideas around active transport in the course of their work, this may have a significant impact on participation. This would align with, and could add value to, existing population-based strategies, such as policies to develop healthy environments, community campaigns and transport policies. An analogy exists with GPs providing brief advice on smoking cessation. There is evidence to suggest GPs’ advice augments the experience of patients as they navigate a world of increasing tobacco taxes, community mobilisation against tobacco and increased regulation on smoking in public places.18,19 Investigating potential synergistic links between clinical practice and population strategies in active transport could provide a potential fruitful area of future research.
A broader understanding of active transport may also provide additional tools for GPs in discussing physical activity with their patients. The modest effects of existing physical activity brief interventions appear to wane with time, and evidence for sustained behaviour change at 12 months is weak.20,21 Because it fits into daily routines, it is plausible that promoting active transport may be one tool to bring about longer, more sustained changes in physical activity behaviour.
Finally, the literature suggests a complex interaction between active transport participation, ethnicity, gender and socioeconomic position.22,23 In countries such as Australia and the UK where use of active transport is low, the literature describes much of the recent growth, particularly in commuter cycling, being among Caucasian, educated, middle-class males.24–26 This phenomenon presents a potential problem of widening health inequities. The perspectives of GPs may aid in better understanding the cultural and socioeconomic barriers that shape active transport participation, which may help in addressing these inequalities.
Implications for general practice
GPs are well positioned to contribute to the promotion of active transport. Initial efforts to incorporate active transport evidence into relevant clinical practice guidelines and the development of an RACGP position statement could help raise awareness in the general practice community.
Research priorities that focus on the acceptability and feasibility of clinical active transport interventions from the patient perspective would be welcome, as would better understanding of local risks of commuter cycling. If tailored to geographical areas, these latter data could go some way to giving GPs the information they need to better judge local risks and benefits.
Clinical interventions that synergise with population-based active transport initiatives might have the potential to enhance sustained physical activity behaviour change.
GPs can make valuable contributions to the healthy environment policy debate and help to inform programs and policies to minimise barriers and inequalities in active transport uptake and use.
Authors
Chance Pistoll MBBS, MSc (Public Health), FRACGP, General Practitioner, Lecturer in Primary Care and Healthy Environments, Research Fellow, Department of General Practice, Melbourne Medical School, University of Melbourne, Parkville, Vic. c.pistoll@unimelb.edu.au
John Furler MBBS, PhD, FRACGP, General Practitioner and Principle Research Fellow, Department of General Practice, Melbourne Medical School, University of Melbourne. Parkville, Vic
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
This study was completed as a part of Dr Pistoll’s Academic General Practice Registrar Special Skills post and received funding through the Australian Department of Health, AGPT Academic General Practice Registrar program. We are grateful to Dr Susan Wearne and Dr Louise Stone from the Department of Health for providing feedback on the study design. The Department of Health had no involvement in data collection, data analysis or writing this paper. This paper does not reflect the views of the Department of Health.