In seeking contraception, young women are typically demonstrating their intention not to become pregnant. However, as high rates of unintended pregnancy, terminations and use of the ‘morning after pill’ attest, many young women either use unreliable methods of contraception or are unreliable in their use of contraception.1 Contraception should be easy, safe, reversible, reliable and have minimal side effects. This is especially important for those who are in the early stages of their sex lives, when fecundity and risk of sexually transmissible infections (STIs) are high, and immaturity combined with opportunity can compromise the best of intentions.
Long-acting reversible contraceptives (LARCs) are defined as any contraceptive that requires administration less than once per cycle (ie per month).2 This includes copper and progestogen-only intrauterine devices (IUDs), and progestogen subdermal implants and injections. However, subdermal implants and IUDs, which have a life of at least three years, have superior efficacy over injections, which require administration every three months. Implants and IUDs are highly cost-effective when compared with other contraceptive methods.
By reducing heavy menstrual bleeding and menstrual pain, LARCs can also provide benefits beyond contraception.3 What LARCs have in common is their efficacy; LARC methods are statistically less likely to result in an unintended pregnancy than vasectomy or tubal ligation.4 One study estimated that if only 5% of British women of reproductive age who are typical users of oral contraceptives used a LARC instead, the decrease in contraception failure would result in 7500 fewer unplanned pregnancies annually.5 Only IUDs and implants will be considered further in this paper.
Globally, it is recognised that adolescents are at high risk of unintended pregnancy, and that increased access to LARC methods would be of benefit in addressing this.2,6 Recommendations for LARC use as first-line contraception in nulliparous women have been in place for over a decade in the US and UK;2,6 however, Australian studies have found that general practitioners (GPs) and women see the oral contraceptive pill as the prevailing cultural contraceptive norm.7,8 Analysis of Australian data between 2007 and 2011 found that for women aged 12–24 years, 5.3 per 100 contraception issues managed in a consultation were in relation to the etonogestrel implant (implant).9 For women of the same age group, only 0.3 per 100 contraception issues managed were in relation to IUDs. Rates of IUD use remain very low in Australia, with a global review of women aged 15–49 years citing that only 1.3% of Australians used IUDs.10
The subdermal etonogestrel implant
Currently, of the IUD and the etonogestrel implant, the implant is the more common choice for young nulliparous women. In the early days of implant use there were stories on the internet of incorrect insertions resulting in pregnancy; however, a superior delivery system has addressed these risks and it is now recognised as being highly acceptable and extremely effective for young nulliparous women.
While changes in menstrual bleeding with any progestogen-only contraceptive is to be expected, there is some evidence that changes in bleeding patterns are more likely to result in discontinuation of the implant than the IUD. A review of 11 clinical trials conducted in different countries, with almost 1000 patients aged 18–40 years who had used the implant, found 11.3% of women discontinued implant use because of bleeding irregularities.11 Changes in bleeding patterns were not uncommon, with women experiencing amenorrhoea (22.2%), infrequent (33.6%), frequent (6.7%) or prolonged bleeding (17.7%). Dysmenorrhoea was resolved in 77% of women who experienced this at baseline. However, as this analysis included women up to 40 years of age, whether the impact is the same on nulliparous and very young women is not clear. For these women, their life stage, past menstrual experiences and ability to cope with unexpected bleeding are very different from that of older women. More nuanced studies are needed to unpack the many issues, physical and psychological, that are associated with discontinued implant use.
The only absolute contraindication to the use of an implant is current breast cancer. The risks of implant use are considered to outweigh the benefits for patients with severe cirrhosis, unexplained vaginal bleeding and a past history of breast cancer.12
The IUD
Although uptake of the implant remains low in Australia, uptake of the IUD is even lower.9 There is evidence that concerns about current IUDs, based on experiences with older devices, have resulted in a reluctance by practitioners to prescribe IUDs, particularly for nulliparous women.13
IUD myths
Risk of infection and pelvic inflammatory disease
A key barrier to IUD use by adolescents has been identified as healthcare providers’ concerns about its safety, particularly in adolescents in the younger age group.14 One of the strongest myths appears to be the misperception that IUDs are associated with higher rates of pelvic inflammatory disease (PID). This myth probably stems from the widely publicised class action against the US manufacturers of the Dalkon Shield in the 1970s. This IUD was found to cause infection, infertility, spontaneous abortion and ectopic pregnancy because of the multifilament tail inside a thin nylon sheath that promoted the ascent of bacteria from the vagina to the uterus.13 There is no evidence for an association between sepsis and the vastly modified IUDs with their monofilament strings that are currently available.15
The American Congress of Obstetricians and Gynecologists (ACOG) offers evidence from studies prior to 2000 to demonstrate the very low absolute risk of PID associated with IUD insertion.6 A slightly more recent review comparing women of all ages with chlamydia or gonorrhoea with those who did not have an infection at the time of copper IUD insertion found an absolute PID risk of 0–5% for those with STIs and 0–2% for those without.16 Studies exploring the risks of infection with the use of currently available IUDs are scarce, but such studies are compromised by the asymptomatic nature of many STIs.
Difficulty of insertion and pain
There is little evidence to suggest that IUD insertion is technically more difficult in adolescents compared with older women.6 In Australia, some providers will insert an IUD under a light general anaesthetic. Other forms of pain management used for IUD insertion include nonsteroidal anti-inflammatory drugs (NSAIDs) and local cervical anaesthetics. In a 2009 review of randomised controlled trials that explored interventions for insertion pain,17 only four trials, each from a different country, could be found. The findings highlight the difficulty of comparing such trials and the need for further robust research. However, in any trial, it would be difficult to control for the expectation of pain held by many young women, and no studies have yet compared the pain of insertion of different types of IUDs for nulliparous women.
Risk of perforation during insertion
A large European study of 64,000 women found an overall risk of perforation of 1.4 per 1000 women. The authors described perforation as rare, with an absence of serious sequelae. However, only 0.9% of the women were aged under 20 years.18 While the risk of perforation on insertion would seem more likely for nulliparous women because of greater resistance to cervical dilation and a smaller uterine cavity, no studies have directly compared perforation risk between nulliparous and parous women.19 A pilot study reporting on 117 insertions in nulliparous women reported no perforations.20 Although not currently available in Australia, Kyleena, Liletta and Skylar are newer and slightly smaller IUDs that may be of benefit for nulliparous women. The ACOG6 makes no mention of the risks of perforation during insertion for these or the Paragard and Mirena IUDs, which are available in Australia, suggesting that they do not consider it an important risk.
Risk of expulsion
Most reviews that have highlighted young age, previous IUD expulsion and nulliparity as being associated with slight increases in expulsion risk have been limited and equivocal, and focus on studies conducted prior to 2002.19 A recent chart review, covering 36 months, of approximately 2500 women aged 13–35 years found an expulsion rate of 6% and no differences in expulsion rate according to age.21 By contrast, the contraceptive CHOICE project followed, also for 36 months, approximately 5400 women aged 14–45 years who received an IUD. Expulsions were more common in those aged 14–19 years, and in women of all ages who were parous, obese (body mass index [BMI] ≥30 kg/m2) and with self-reported heavy menses.22
Risk of ectopic pregnancy
Given the very high effectiveness of IUDs, the absolute risk of an ectopic pregnancy is extremely low.23 The European Active Surveillance Study for Intrauterine Devices monitored more than 60,000 women aged 18–50 years with newly inserted copper IUDs or Mirena IUDs for one year. While ectopic pregnancy rates were slightly higher in women aged under 30 years compared with older women, overall ectopic pregnancy rates were extremely low. In keeping with earlier research, ectopic pregnancy rates were 0.02–0.2 per 100 woman-years for Mirena users, and 0.1–0.8 per 100 woman-years for copper IUD users.24
Contraindications
Absolute contraindications to IUD use are pregnancy, insertion after puerperal sepsis or septic abortion, unexplained vaginal bleeding, gestational trophoblastic disease with rising ß-human chorionic gonadotropin levels, endometrial cancer, distortion of the uterine cavity from fibroids or congenital abnormality, and current PID.12
Patient perceptions
Studies of patient perceptions found that barriers to the wide use of LARC methods by adolescents include a lack of familiarity with, or misperceptions about, the methods, high cost, and lack of access.25 In the Australian study of the Contraceptive Use, Pregnancy Intentions and Decisions (CUPID) of almost 3800 Australian women aged 18–23 years, 158 participants commented on a contraceptive consultation they had had with a GP.26 Some participants believed they were offered limited choices because of their age, none discussed LARCs, and many felt that their GPs did not give them information about potential side effects of contraceptives.
A strong predictor of the type of contraception used is knowledge of contraceptive methods. One study found that for every correct response on a contraceptive knowledge scale, the likelihood of a young woman aged 18–29 years using a hormonal implant or LARC increased by 17%.27
An online quantitative study of 200 Australian women aged 18–50 years and 162 GPs found that side effects of contraception and frequency of administration were the two most important considerations for participants. Interestingly, women rated cost as more important than effectiveness, whereas GPs held the opposite view. However, as this study included women up to 50 years of age, results should not be extrapolated to nulliparous women.7
From a practical point of view, young women are most likely to be worried about the pain of LARC insertion. While distressing anecdotes about the pain of IUD insertions are abundant on the internet,28 accounts of successful and pain-free insertion are few and far between. Compounding this is the fact that there are few studies of IUD insertion that include nulliparous women, resulting in a limited data pool.19
The GP’s role
Recently, it has been argued that health practitioners seeing young women seeking contraception should reconsider the way in which they deliver information. Health practitioners in the US-based contraceptive CHOICE study were instructed to counsel on the full range of birth control options; however, they were to first present birth control options with the strongest evidence of effectiveness (ie LARC), before offering evidence‑based information about safety, effectiveness, risks and benefits of all reversible contraceptive methods.25 Of the 5086 women aged 14–20 years who were enrolled in the study, 3557 chose a LARC method (70%). Of those aged 14–17 years, 69% chose a LARC and of those aged 18–20 years, 61% chose a LARC. Among those choosing a LARC, 63% of those aged 14–17 years chose the implant, and 71% of those aged 18–20 years chose an IUD. LARC use is clearly acceptable and common among adolescents, with the younger group being more interested in the implant.
An Australian trial is following on from the CHOICE study. Mazza and colleagues recently received National Health and Medical Research Council (NHMRC) funding for the Australian Contraceptive ChOice pRoject (ACCORd) study. This study will educate GPs to provide LARCs as the first structured contraceptive advice to all women seeking contraception.29 The study will also facilitate the implementation of rapid referrals to overcome one of the existing barriers to LARC prescription, which potentially leaves the patient without reliable contraception while waiting for an appointment for LARC insertion.30 ACCORd will directly address the Family Planning Alliance Australia’s 2014 position statement, which states that ‘LARC can be offered as a first-line contraceptive option for all women, including young women, despite the misperception that IUDs are not suitable for this age group’.31 This position statement calls for all practitioners to discuss the benefits of LARCs with patients seeking contraception, and to ensure that access to LARCs be facilitated by the provision of clear local referral pathways. The statement has been supported by a recent expert round table, which also called for primary care incentives to encourage greater LARC use.32
Conclusion
Ineffective contraception is a major risk for unintended pregnancy and can be the result of inconsistent condom or oral contraceptive use, or use of the withdrawal method. LARCs offers effective and safe contraceptive alternatives and are well accepted by women of all ages. LARCs are recommended in the UK, US and Australia as first-line contraceptives for nulliparous women; however, misperceptions held by health practitioners may be contributing to the low uptake of these methods.
Key points
- Proactively and opportunistically review women’s contraceptive choices (eg at presentations for script renewal, Pap smear testing, Well Women’s Check) to determine their satisfaction with their current form of contraception. Ensure they are aware of the newer LARC methods and their safety, ease of use and efficacy, including in young women.
- The chart of relative effectiveness (Figure 1) is useful in explaining that LARC has the lowest failure rate of all contraceptive methods. Furthermore, there is no evidence that IUDs alter the likelihood of pregnancy following removal.2
- Check whether patients harbour any misconceptions about LARCs and rectify these. Many young women are ignorant about their genital anatomy, and will need concrete description about IUD insertion. They will also need a realistic view of the possible discomfort involved, given the proliferation of negative stories on the internet.33 Ensure women understand insertion and removal procedures, including pain relief options, and potential side effects of the method and management options for these. Box 1 offers some useful websites for patient information.
- Arrange to review the patient after insertion to check experiences and institute management appropriate for side effects.
- Pap smears are not essential before inserting an IUD,34 but remind women that contraception does not protect against STIs, and screen for STIs at the time of or before insertion of LARC.
- The copper IUD is a good choice for young women who prefer to be hormone-free.
- For detailed advice, the WHO guidelines on medical eligibility provide a frequently updated, detailed and well-referenced guide to contraceptive choice for women of different ages, parities and comorbidities.23
- Information for GPs on insertion is available at:
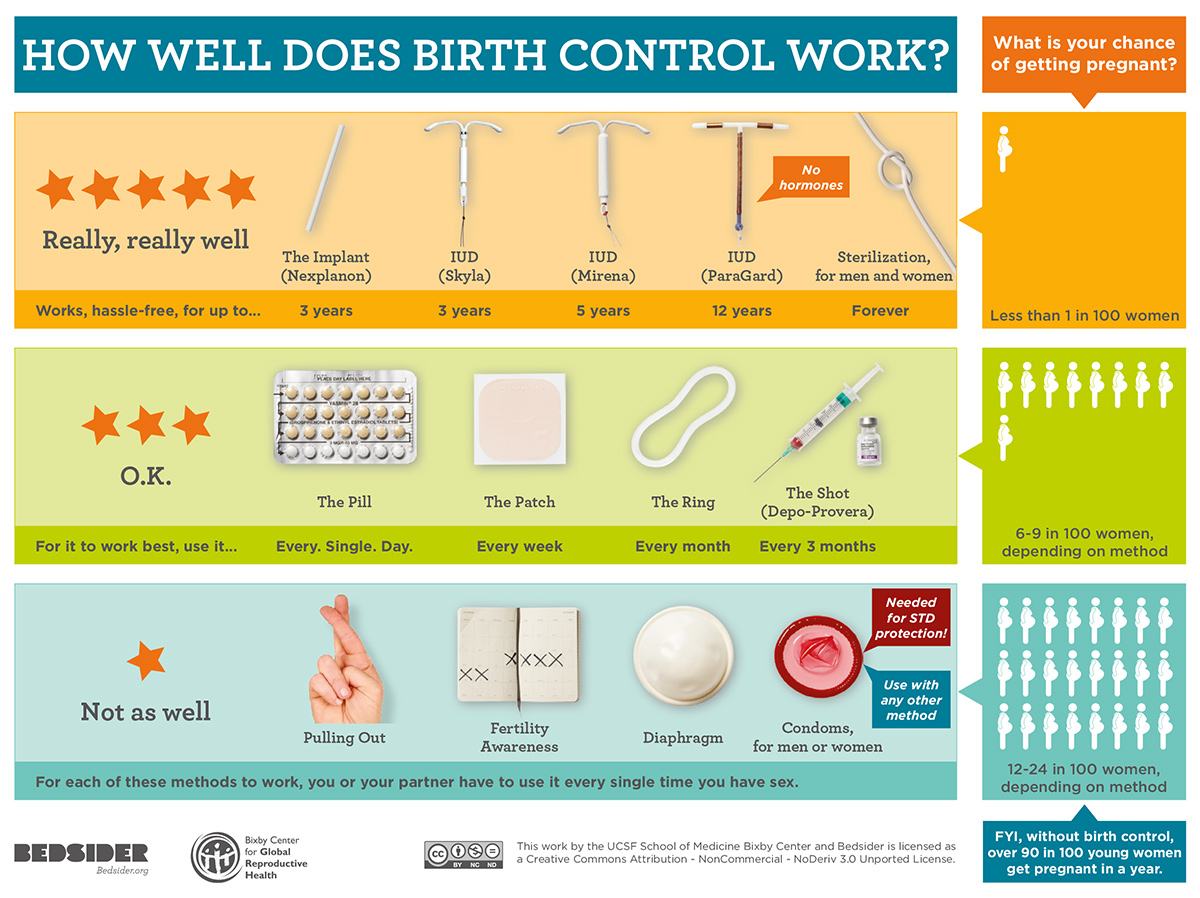
Figure 1. Relative effectiveness of contraception
Authors
Meredith Temple-Smith BSc, MPH, DHSc, Director of Research Training, Department of General Practice, Melbourne Medical School, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Parkville, Vic. m.temple-smith@unimelb.edu.au
Lena Sanci MBBS, PhD, FRACGP, Deputy Head, Department of General Practice, Melbourne Medical School, Faculty of Medicine, Dentistry and Health Sciences, University of Melbourne, Parkville, Vic
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.