Winnunga sees around 4000 patients per year and has operated a monthly diabetes clinic since 2002.6 In addition to being a source of peer support, the clinic provides cooking demonstrations and patient education on lifestyle changes and diabetes management. Patients can access podiatry, dietician and diabetes educator services without appointments. An endocrinologist also visits every 3 months.
This study also aimed to contribute to the understanding of the health of urban Aboriginal and Torres Strait Islander peoples by reviewing diabetes management in Winnunga. A number of studies have focused on rural Aboriginal and Torres Strait Islander communities.7–9 Less information is available on diabetes care of Aboriginal and Torres Strait Islander peoples living in an urban setting, where the majority of Aboriginal and Torres Strait Islander peoples live.10–13
Methods
This study was a retrospective clinical audit of a random sample of 65 adult patients with type 2 diabetes who attended Winnunga during 2012 and who were active clients (ie visited three or more times over 2 years). The random sample represented 45% of the target population (145 patients). Electronic medical records were used to identify patients. The variables extracted included patient characteristics, clinical outcomes (HbA1c, low-density lipoprotein [LDL], high-density lipoprotein [HDL], total cholesterol, triglycerides, blood pressure, urinary albumin creatinine ratio, eGFR, BMI), medications and dates of the last examinations and investigations.
Patient records were audited using outcome targets and optimal monitoring frequencies from the Royal Australian College of General Practitioners (RACGP) guidelines (Table 1).14 Analysis included the proportion of patients who met optimal monitoring frequencies and mean clinical outcomes, and the proportion of patients who met the RACGP outcome targets. Results were compared with the National Association of Diabetes Centres (NADC) Audit and Benchmarking study.15 The NADC report summarised diabetes care for 3356 adults, mostly non-Indigenous, with type 2 diabetes from 42 diabetes centres around Australia during 2011.
Table 1. Management guidelines for type 2 diabetes 2011/12
|
Checks
|
Monitoring frequency
|
|---|
| Height and weight |
Quarterly |
| Blood pressure |
Quarterly |
| Eyes check |
Annually |
| Feet check |
Annually |
| HbA1c |
Bi-annually |
| Lipids (triglyceride; HDL, LDL, total cholesterol) |
Annually |
| Renal: microalbuminuria (ACR) and plasma creatinine (eGFR) |
Annually |
|
ACR, albumin:creatinine ratio; eGFR, estimated glomerular filtration rate
|
|---|
Winnunga patients who attended the diabetes clinic were compared with those who did not attend. Clinical outcomes between the two groups were compared using Student's t-tests and Chi-square tests, with a 5% level of significance. Excel and STATA were used to perform statistical analyses.
Ethical approval was obtained from the Australian National University Human Research Ethics Committee (reference number 2012/485). The Winnunga Board also approved this project.
Results
Patient characteristics
The mean patient age was 56 years. Most patients identified as Aboriginal and Torres Strait Islander (Table 2). On average, patients visited Winnunga general practitioners (GPs) 10 times during 2012, and almost half attended the diabetes clinic at least once.
Table 2. Characteristics of patients with diabetes at Winnunga, 2012
| Number of patients in sample (n) |
65 |
| Mean age (years) |
55.6 |
| Female (%) |
59 |
| Aboriginal and Torres Strait Islander (%) |
85 |
| Mean Winnunga GP visits, 2012 |
10 |
| Visits diabetes clinic (%) |
45 |
| Mean visits to diabetes clinic |
1.2 |
| Endocrinologist involved in care (%) |
15 |
| Completed cycle of care (%) |
9.2 |
| Smoker (%)* |
29 |
| Mean BMI (kg/m2)* |
36.7 |
| *Results not available for all participants; n = 52 for smoker; n = 51 for BMI |
|---|
Diabetes care processes
Blood pressure was the most frequently monitored outcome; about two-thirds of patients had their blood pressure checked in the past 3 months (Table 3). A similar proportion of patients had their lipids and renal function monitored in the past 12 months. However, only 40% of patients had their HbA1c checked in the past 6 months. Only around one-third of patients had their eyes and feet checked in the past 12 months. Vaccination rates were low.
Table 3. Diabetes-related checks and preventive care at Winnunga, 2012
| |
Winnunga
(n = 65) %
|
|---|
| BMI checked in past 3 months |
43 |
| BMI checked in past 12 months |
68 |
| Eyes checked in past 12 months |
29 |
| Feet checked in past 12 months |
35 |
| HbA1c checked in past 6 months |
40 |
| HbA1c checked in past 12 months |
68 |
| Lipids checked in past 12 months |
68 |
| Blood pressure checked in past 3 months |
65 |
| Blood pressure checked in past 12 months |
89 |
| ACR checked in past 12 months |
60 |
| eGFR checked in past 12 months |
71 |
| Influenza vaccination in past 12 months |
42 |
| Pneumococcal vaccination in past 5 years |
29 |
| ACR, albumin:creatinine ratio; eGFR, estimated glomerular filtration rate |
|---|
Clinical outcomes
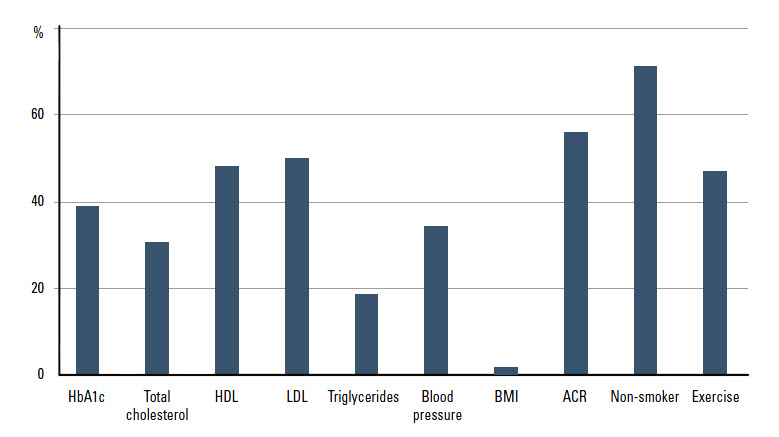
Most clinical outcomes had a low rate of missing values (Table 4). The mean HbA1c level was 8.2%; 39% of patients with a recorded HbA1c had good glycaemic control (HbA1c <7%; Figure 1); and 19% of patients had an HbA1c of 7–8%. The average blood pressure was 136/80 mmHg and 34% of patients achieved the target (<130/80 mmHg). Almost one-third of the patients smoked. Almost all patients with recorded BMIs were overweight or obese; the mean BMI was 37 kg/m2. Less than half of the patients exercised for more than 30 minutes a day; 72% of patients were on metformin; and 25% were on insulin.
Table 4. Clinical outcomes for patients with diabetes at Winnunga, 2012a
|
Clinical outcome
|
n
|
Winnunga (mean)
|
RACGP guideline (targets)
|
|---|
| HbA1c (%) |
59 |
8.2 |
≤7 |
| Blood pressure systolic (mmHg) |
64 |
136 |
≤130 |
| Blood pressure diastolic (mmHg) |
64 |
80 |
≤80 |
| Total cholesterol (mmol/L) |
59 |
4.6 |
<4.0 |
| LDL cholesterol (mmol/L) |
58 |
2.5 |
<2.5 |
| HDL (mmol/L) |
58 |
1.1 |
>1.0 |
| Triglycerides (mmol/L) |
59 |
2.3 |
<1.5 |
| ACR (mg/mmol) |
52 |
28.6 |
<3.5 (women)
<2.5 (men) |
| eGFR (mL/min/1.73 m2) |
59 |
86.9 |
– |
|
RACGP guideline targets
|
n
|
% of Winnunga patientsb
| |
|---|
| HbA1c ≤7% |
59 |
39 |
|
| Blood pressure <130/80 mmHg |
64 |
34 |
|
| Total cholesterol <4.0 mmol/L |
59 |
31 |
|
| HDL >1 mmol/L |
58 |
48 |
|
| LDL <2.5 mmol/L |
58 |
50 |
|
| Triglycerides <1.5 mmol/L |
59 |
19 |
|
| BMI <25 kg/m2 |
51 |
2 |
|
| ACR (women: <3.5 mg/mmol; men: <2.5 mg/mmol) |
52 |
56 |
|
| Non-smoker |
52 |
71 |
|
| Exercise (>30 min/day) |
51 |
47 |
|
|
Medications
|
|---|
| Metformin (%) |
|
72 |
|
| Insulin (%) |
|
25 |
|
| Other diabetic medications (%)c |
|
28 |
|
| Exenatide (%) |
|
11 |
|
| Combinations (%)d |
|
6 |
|
|
aResults not available for all participants
bRepresents percent of those where the test or procedure was done
cPioglitazone maleate, glimepiride, gliclazide, rosiglitazone, glibenclamide, vildagliptin, carbose, sitagliptin, glipizide, saxagliptin, linagliptin, liraglutide
dMetformin hydrochloride combined with rosiglitazone, vildagliptin, sitagliptin, or glibenclamide
ACR, albumin:creainine ratio; eGFR, estimated glomerular filtration rate
|
|---|
*Results not available for all participants; data represents percent of those where the test or procedure has been done
|
|
Figure 1. Clinical outcomes for patients with diabetes at Winnunga, percentage of patients within RACGP therapeutic targets, 2012*
|
|---|
Comparison with non-Indigenous Australians (NADC)
The sample of mainly Aboriginal and Torres Strait Islander peoples from Winnunga were, on average, about 8 years younger than the mostly non-Indigenous sample from Australian diabetes centres.15 Winnunga patients were more likely to smoke (29%, compared with 13%) and be overweight; only 2% of Winnunga patients with a recorded BMI had a BMI of less than 25 kg/m2, compared with 11% of the NADC sample. Winnunga patients on average had a higher HbA1c (8.2%, compared with 7.9%) and poorer lipid control. A lower proportion of Winnunga patients met the blood pressure target (34%, compared with 53%). However, the rate of albuminuria was lower among Winnunga patients (44%, compared with 55%). A higher proportion of Winnunga patients was on insulin (25%, compared with 19%).
Comparison between diabetes clinic attendees and non-attendees
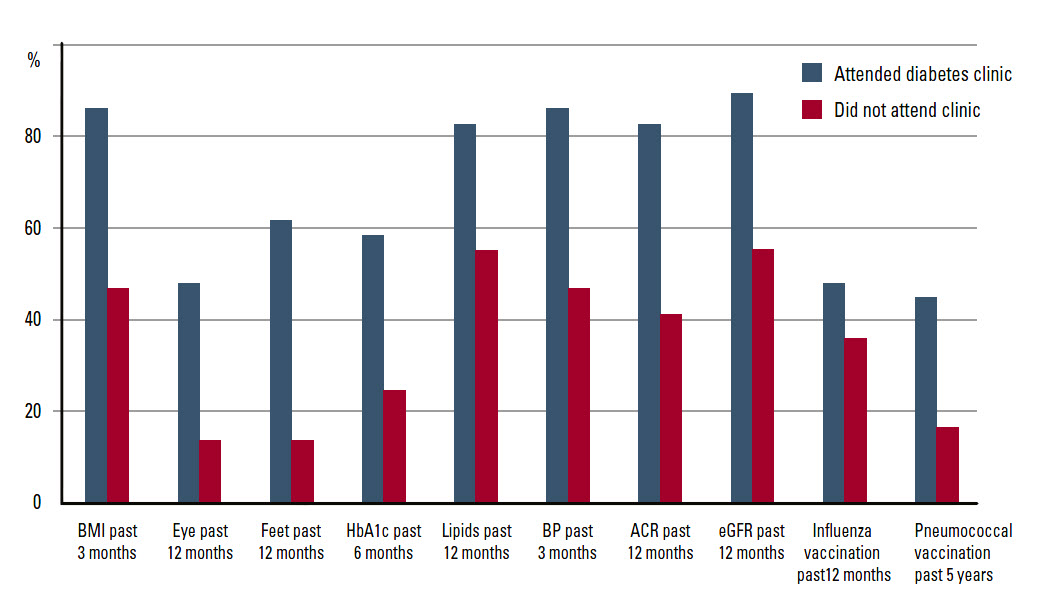
There was no statistically significant difference between characteristics of Winnunga patients who attended the diabetes clinic and those of non-attendees (at 5% level of significance; Table 5). On average, those who attended the clinic visited Winnunga GPs more regularly (13, compared with 7 times in 2012). Clinic attendees were statistically significantly more likely to meet the targets for routine checks (Figure 2; Table 5) and have pneumococcal vaccination recorded.
There were no statistically significant differences in the clinical outcomes between the two groups. Metformin use was statistically significantly higher among those who attended the clinic (90%, compared with 58%) but insulin use was similar (25%). Those who attended the clinic were also more likely than non-attendees to be using other diabetic medications.
Table 5. Characteristics of two groups of patients with diabetes at Winnunga, 2012
|
Characteristicsa
|
Attended diabetes clinic (n = 29)
|
Did not attend diabetes clinic (n = 36)
|
|---|
|
Age (years)
|
56.9
|
54.5
|
|
Female (%)
|
52
|
64
|
|
Aboriginal and Torres Strait Islander (%)
|
93
|
78
|
|
Winnunga GP visits, 2012
|
13.0*
|
6.7
|
|
Visits to diabetes clinic
|
2.7
|
0.0
|
|
Endocrinologist involved in care (%)
|
17
|
14
|
|
Completed cycle of care (%)
|
14
|
5.6
|
|
Smoker (%)b
|
19
|
39
|
|
BMIb (kg/m2)
|
37.2
|
36.0
|
|
Checks
|
|---|
|
BMI checked in past 3 months (%)
|
86*
|
47
|
|
Eye checked in past 12 months (%)
|
48*
|
14
|
|
Feet checked in past 12 months (%)
|
62*
|
14
|
|
HbA1c checked in past 6 months (%)
|
59*
|
25
|
|
Lipids checked in past 12 months (%)
|
83*
|
56
|
|
BP checked in past 3 months (%)
|
86*
|
47
|
|
ACR checked in past 12 months (%)
|
83*
|
42
|
|
eGFR checked in past 12 months (%)
|
90*
|
56
|
|
Influenza vaccination in past 12 months (%)
|
48
|
36
|
|
Pneumococcal vaccination in past 5 years (%)
|
45*
|
17
|
|
Clinical outcomesa,b
|
|---|
|
Blood pressure systolic (mmHg)
|
134
|
138
|
|
Blood pressure diastolic (mmHg)
|
80
|
81
|
|
HbA1c (%)
|
8.2
|
8.1
|
|
Total cholesterol (mmol/L)
|
4.4
|
4.7
|
|
LDL(mmol/L)
|
2.3
|
2.6
|
|
HDL (mmol/L)
|
1.0
|
1.1
|
|
Triglycerides (mmol/L)
|
2.3
|
2.4
|
|
ACR (mg/mmol)
|
12
|
48
|
|
eGFR (mL/min/1.73 m2)
|
79*
|
94
|
|
RACGP guideline targetsb
|
|---|
|
HbA1c ≤7% (%)
|
30
|
47
|
|
Total cholesterol <4.0 mmol/L (%)
|
33
|
28
|
|
HDL >1 mmol/L (%)
|
41
|
55
|
|
LDL <2.5 mmol/L (%)
|
59
|
42
|
|
Triglycerides <1.5 mmol/L (%)
|
19
|
19
|
|
Blood pressure < 130/80 mmHg (%)
|
29
|
39
|
|
BMI <25 kg/m2 (%)
|
0
|
4
|
|
ACR (women: <3.5 mg/mmol; men: <2.5 mg/mmol) (%)
|
61
|
50
|
|
Non-smoker (%)
|
81
|
62
|
|
Exercise (>30 min/day) (%)
|
35
|
60
|
|
Medications
|
|---|
|
Metformin (%)
|
0.90*
|
0.58
|
|
Insulin (%)
|
0.24
|
0.25
|
|
Other diabetic medications (%)c
|
0.41*
|
0.17
|
|
Exenatide (%)
|
0.24*
|
0.00
|
|
Combinations (%)d
|
0.10
|
0.03
|
|
aData are means unless stated otherwise.
bResults not available for all participants, n for attendee and non-attendee; smoker: 26, 26; BMI: 27, 24; HbA1c: 27, 32; total cholesterol/triglycerides: 27, 32; HDL/LDL: 27, 31; blood pressure: 28, 31; ACR: 28, 24; eGFR: 28, 31; exercise: 26, 25.
cPioglitazone maleate, glimepiride, gliclazide, rosiglitazone, glibenclamide, vildagliptin, carbose, sitagliptin, glipizide, saxagliptin, linagliptin, liraglutide
dMetformin hydrochloride combined with rosiglitazone, vildagliptin, sitagliptin, or glibenclamide
*Indicates statistically significant difference between the two groups at 5% level of significance
ACR, albumin:creatinine ratio; eGFR, estimated glomerular filtration rate
|
|---|
 |
|
Figure 2. Diabetes related checks and preventative care of two groups of patients
with diabetes at Winnunga, 2012
|
|---|
Discussion
This study assessed the effectiveness of a diabetes clinic in a sample of mostly Aboriginal and Torres Strait Islander peoples in an urban ACCHS setting. The patients with diabetes at Winnunga were, on average, much younger than patients from the NADC sample. The smoking rate among Winnunga patients with diabetes (29%) was twice that of the NADC sample, but was substantially lower than that of Aboriginal and Torres Strait Islander peoples in general (50%) and Winnunga patients in general (56%).16 Almost all of the Winnunga patients with recorded BMIs were overweight or obese. Managing such risk factors could reduce the risk of diabetes and its complications.14,17,18 In over half of people presenting with type 2 diabetes, restriction of energy intake, increased activity and weight reduction would initially normalise blood glucose levels.19
A primary healthcare service such as Winnunga is the appropriate place to influence risk factor behaviour.
Overall, diabetes checks were routinely conducted, although there is room for improvement. In particular, examination of eyes and feet were often not recorded. The low rates might partly reflect the inconsistent or under-recording of checks performed, especially the eye checks, which are not performed by the service. A systemic approach to care in the general practice setting is likely to result in better outcomes.14
This audit showed that clinical outcomes at Winnunga could be improved. We found that control of risk factors was suboptimal and more intensive management of glycaemia, including lifestyle modifications, was required.
Our study found that those who attended the diabetes clinic were more likely to meet targets for routine checks. This was expected as the clinic educated patients about the importance of checks and provided many of these services. Attendees visited Winnunga GPs more regularly and this contributed to more frequent monitoring. Attendees also had higher vaccination rates and were more likely to be receiving therapeutic intervention, although this might reflect the fact that attendees required more complex management.
The findings were consistent with existing studies that examined the effectiveness of a diabetes clinic in primary care.3–5 These studies have also found positive associations between diabetes clinic attendance and a number of outcomes, including regular checks and reduced hospital admissions.
However, this study found no statistically significant difference in the clinical outcomes between diabetes clinic attendees and non-attendees. This differed from some studies showing that clinic attendance was associated with reduced HbA1c levels.3,20 The lack of association in our study may be because those who had more severe diabetes were more likely to be referred to or to attend the diabetes clinic. The cross-sectional nature of the data meant that it was not possible to establish causation between clinic attendance and the quality of care. Multivariate analysis of longitudinal data would provide more information about the effect of attendance on outcomes. Another limitation was that some patients' clinical outcomes were not recorded, although most outcomes had a low rate of missing values.
The lack of association between clinic attendance and outcomes does not necessarily suggest that the clinic is ineffective. Clinic attendance was associated with more routine checks, which should result in earlier intervention. The clinic may also provide benefits beyond those examined by this study. For example, the clinic was a source of peer support. A comprehensive diabetes clinic may also remove the need for patients to visit many different care providers, saving them time and money.
Implications for general practice
- A comprehensive diabetes clinic can improve management in the ACCHS setting.
- A diabetes clinic can improve regularity of checks and vaccination rates, although insufficient evidence exists to show that attendees have better clinical outcomes.
- This model may be transferrable to other primary care settings.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.