Table 1. Pregnancy factors and outcomes associated with decreased fetal movements
|
Pregnancy factors associated with DFM
|
Outcomes associated with DFM
|
|---|
- Fetal growth restriction
- Small for gestational age
- Placental insufficiency
- Oligohydramnios
- Threatened preterm labour
- Fetomaternal transfusion
- Intrauterine infections
|
- Congenital malformation
- Preterm birth
- Perinatal brain injury
- Disturbed neurodevelopment
- Low birth weight
- Low Apgar score
- Hypoglycemia
- Cesarean section
- Induction of labour
- Fetal death
- Neonatal death
|
In particular, DFM is associated with an increased risk of perinatal death (this includes fetal and neonatal deaths).2 Despite advances in obstetric care and decreased perinatal mortality rates in high-income countries, fetal death rates have remained stagnant for the last decade.5 In Australia, the current fetal death rate is 7.4 per 1000 births, and the neonatal death rate is 2.9 per 1000 births. Perinatal mortality rate for Aboriginal or Torres Strait Islander peoples is 20.1 per 1000 births. Pregnant women should therefore be advised to report DFM, as recognition and management may provide an opportunity to prevent adverse outcomes.
Normal fetal movements
Normal fetal movements can be defined as 10 or more fetal movements in 2 hours, felt by a woman when she is lying on her side and focusing on the movement,2–4,6 which may be perceived as ‘any discrete kick, flutter, swish or roll’.1 Fetal movements provide reassurance of the integrity of the central nervous and musculoskeletal systems.1 The majority of pregnant women report fetal movements by 20 weeks of gestation.1
The average number of movements perceived at term is 31 per hour, ranging from 16–45, the longest period between movements being 50–75 minutes.1 Sleep cycles, in which fetal movements can be absent, usually last 20–40 minutes and rarely exceed 90 minutes.1 As the fetus matures, the amount of movement and the nature of movement will change.1 Women should be educated about DFM during antenatal visits, and be given verbal and written information.2,4
Perception of movement
Fetal movement is a subjective measure, mainly assessed by maternal perception.1–2,6 Research has shown that there is a correlation of 37–88% between maternal perception and ultrasound.1 Multiple factors can decrease perception of movement, including early gestation, a reduced volume of amniotic fluid, fetal sleep state, obesity, anterior placenta (up to 28 weeks gestation), smoking and nulliparity.4 Various drugs, including alcohol, benzodiazepines, methadone and other opioids, and cigarette smoking, can cause transient suppression of fetal movement.1,2 A simple explanation provided by some women presenting with DFM is that they have been ‘too busy to feel fetal movements’. It is known that fewer movements are perceived when women are standing or sitting, compared with lying down or concentrating on movements.1 It is commonly thought that having a cold drink or eating something sugary will stimulate fetal movements but there is no evidence to suggest either of these will affect movement.1,2,4
Kick charts, which have been historically used to monitor fetal movement, are not currently recommended.1,2,4 In fact, significant maternal anxiety and unnecessary intervention (ie induction of labour and caesarean section) have been attributed to the use of kick charts.3,4 If there is uncertainty surrounding perceived DFM after 28 weeks gestation, women should be advised to lie on their left side and focus on fetal movements for 2 hours. If they do not feel 10 or more discrete movements in 2 hours they should contact their healthcare provider immediately.1 Nevertheless, maternal concern about decreased fetal movement warrants assessment even if the situation does not comply with the previously stated definition of DFM.2–4
Management of DFM
If a woman presents to her general practitioner with perceived DFM, she will eventually need hospital referral if assessment reflects DFM.3 However, the following elements can be established in primary care.
History
This should include:1,2
- time since onset of DFM
- any fetal movements have been felt – can the DFM be attributed to being too busy to feel movements?
- previous episodes of DFM
- known intrauterine growth restriction (IUGR), placental insufficiency or congenital malformation
- maternal factors such as the presence of hypertension, diabetes, smoking, extremes of age, primiparity, obesity, racial or ethnic risk factors
- previous obstetric adverse events.
Examination
This should include:
- measurement of symphysis–fundal height and palpation of abdomen,1 which should be recorded in the pregnancy health record and compared to previous measurements1,2,4
- auscultation of fetal heart with a Doppler fetal monitor to determine viability.
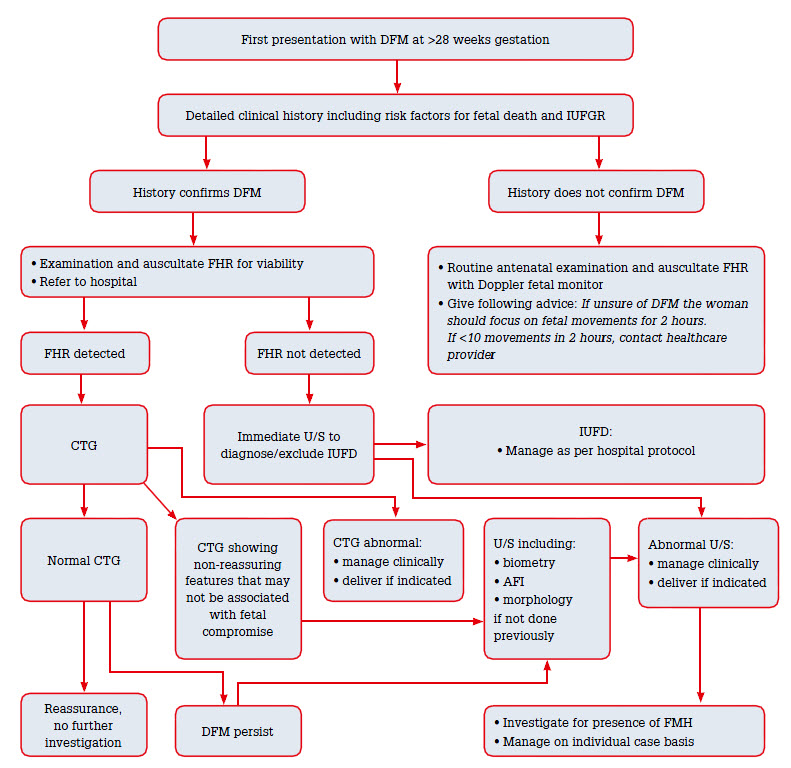
If examination is normal and history does not reflect DFM, further assessment is not indicated at this stage1,4 (Figure 1). If there is a history of DFM and viability is confirmed on Doppler auscultation, a CTG should be performed and referral to hospital is indicated. If CTG is not available in the primary care setting, a woman with a history consistent with DFM should be referred to hospital for a CTG. If the fetal heart is not heard on Doppler auscultation, an urgent hospital referral and ultrasound should take priority.1
 |
|
Figure 1. Decreased fetal movement flow diagram
CTG, cardiotocography; DFM, decreased fetal movements; FHR, fetal heart rate; FMH, fetomaternal haemorrhage; IUFD, intrauterine fetal demise; IUFGR, intrauterine fetal growth restriction; U/S, ultrasound; FMH, fetomaternal hemorrhage
|
|---|
Cardiotocography (CTG)
CTG should be performed for at least 20 minutes. A normal CTG represents a healthy fetus with a normal, functioning autonomic system. CTG monitoring in the setting of DFM has shown to be beneficial in the screening of both low-risk and at-risk pregnancies. In a recent non-randomised Norwegian study of 3014 women presenting with DFM, 97.5% of the women were assessed using a CTG and 3.2% of the presentations were abnormal.4 CTG is a valid screening tool in the setting of DFM, as an abnormal fetal heart rate (FHR) pattern may be associated with poor outcomes.4
Ultrasound
Ultrasound assessment should be considered in any woman presenting with DFM with an abnormal CTG, persistent maternal perception of DFM, or if there is suspected IUGR. One model of practice based on a Norwegian study suggests CTG and ultrasound should be done within 2 hours of presentation if women report no fetal movements.7 This would require prompt referral to hospital from a community setting. If movements are reduced, the study recommends CTG and ultrasound be performed within 12 hours. This approach more than doubled the number of ultrasounds performed but reduced follow-up consultations and induced labour.7 The findings from this study were significant as a reduction in perinatal mortality was shown.7
As a guide, it is recommended that ultrasound be carried out within 24 hours if indicated. However, if CTG is abnormal and ultrasound assessment cannot be delayed, it should be expedited, as immediate delivery may be indicated.1,3 Ultrasound assessment should include abdominal circumference and/or estimated fetal weight to detect IUGR, and assessment of amniotic fluid volume. If fetal morphology has not yet been assessed it would be appropriate to include it in the ultrasound.1,2,4 At present, evidence suggests that the addition of Doppler studies does not provide any additional benefit.2,6,7
The biophysical profile (BPP) is the observed association between hypoxia and FHR, fetal movement and fetal tone. BPP as an investigation into fetal wellbeing in high-risk pregnancies is not currently supported by randomised controlled trials.1 The Cochrane systematic review of BPP for high-risk pregnancies included five studies; however, only two studies included women with DFM. The review concluded that BPP testing was ‘associated with a probable increase in caesarean section and no improvement in neonatal outcome’.1
The recommendation to perform ultrasound assessment for women presenting with DFM is based on the evidence that ultrasonography is useful in detection of conditions contributing to DFM.4
Fetomaternal haemorrhage
Investigation for fetomaternal haemorrhage, for example the Kleihauer-Betke test, should be considered if an abnormal CTG is found but an ultrasound shows a normal fetus.2,3 This recommendation is based on evidence that there is substantial fetomaternal haemorrhage in approximately 4% of fetal deaths and 0.04% of neonatal deaths.8 Clinical risk factors are not a good predictor of the likelihood of massive FMH. It is possible that DFM may be the only history suggesting FMH.3,8
Summary
70% of pregnancies with a single episode of DFM go on to be healthy pregnancies. Women who have normal investigations and resumed movements following a presentation and history suspicious for DFM should always be reassessed if they experience repeat episodes.1 Representation for DFM should prompt review for predisposing factors, examination, CTG and an ultrasound. Early delivery is an option for DFM that may be considered in particular situations, when the risks to the mother and baby have been weighed up appropriately.2–4,6
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.