Hospital emergency departments are under considerable strain across Australia. Recent evidence has found a marked increase in the use of emergency departments, rising by 52% between 2002 and 2013; semi-urgent or non-urgent presentations (triage categories 4 or 5) alone have increased by 33%.1 The peak time of semi-urgent or non-urgent presentations at emergency departments was between 10.00 am and 1.00 pm.2 As this peak time was during the normal operating hours for primary care practices in the community, the reasons for presenting to an emergency department rather than a general practice may relate to perceived or actual availability and affordability of primary care services, as has been shown in a paediatric population.3,4 Hospital data5,6 and interview data regarding emergency department attendance6 suggest that a lack of appointment availability, difficulty in obtaining timely appointments and the high cost of primary care are common barriers to accessing general practice.7
There is little empirical evidence at the local level about actual access to general practitioners (GPs) and bulk-billing rates. A recent study used a ‘secret shopper’ method to assess appointment availability rates in a random sample of general practices in Victoria. Freed et al8 found that 78% (n = 175/225) of general practices offered same-day access for a hypothetical child with a semi‑urgent or non‑urgent presentation. This methodology provides empirically derived estimates of the actual availability and costs for general practice appointments rather than relying on perceptions.
There is a paucity of evidence about same-day appointment availability, bulk‑billing rates and out-of-pocket costs in general practices, particularly across regional areas. Objective, independently derived empirical evidence is needed to develop evidence-based policy approaches to more efficiently target general practice and emergency department services and resources. Therefore, this study replicates the ‘secret shopper’ method described by Freed et al,8 to determine same-day appointment availability, bulk-billing rates and appointment costs for adults in general practices in northern New South Wales.
Methods
The study was a cross-sectional, phone interview census of all available general practices across 12 local government areas in northern New South Wales. The North Coast Primary Health Network (NCPHN) provided a list of primary healthcare practice names, which includes the practices’ local government area, but does not include the number of doctors in each practice or any details about the size of the practice. The NCPHN also approved the hypothetical scenario, which was prepared to enable a standardised patient history should the medical receptionists seek additional information.
Practices were randomised using a random number generator in Microsoft Excel. The caller was a trained researcher who requested an appointment with any available GP from that practice. In total, 184 general practices were contacted by phone on weekdays between 1 and 7 March 2016. All calls were made between 8.30 am and 11.00 am to standardise the likelihood of same-day appointment availability. If the phone was not answered by a person (ie it was diverted to an answer service or rang out), one or two follow-up calls were attempted during the same morning, but was not followed up on a different morning, to preserve the randomisation sequence.
The primary outcome of the study was the availability of a same-day appointment for a new patient for any GP within the practice. Secondary outcomes were:
- the availability of a female GP on the same day
- the availability of bulk billing
- if bulk billing was not available, the associated out-of-pocket costs for the appointment.
The hypothetical patient scenario was designed to reflect a presentation frequently encountered in general practice. The scenario was consistent with a category 4 or 5 classification on the Australasian Triage Scale, if the patient were to present to an emergency department. If required, the researcher posed as the relative of a woman aged 60 years who recently moved to the area, had been experiencing mild abdominal pain over the past few days and was covered by the Medicare Benefits Schedule (MBS) but not eligible for any other concessions.
Data analysis was conducted using Microsoft Excel and Stata (version 13). Appointment availability was calculated as a proportion of the total available appointments, both overall and by local government area. Geographical data from the study was digitised using ArcMap 10.3 to produce a graphical map of same-day appointment availability per local government area.
Ethics approval was obtained from Southern Cross University’s Human Research Ethics Committee (ECN-15-311).
Results
Of 184 practices contacted, 22 were excluded as these exclusively offered specialised medical services, including Aboriginal health services (n = 12), skin clinics (n = 5), women’s health (n = 2) and headspace (n = 1), and because of missing data (n = 2), leaving a sample size of n = 162.
The availability rate of a same-day appointment for new patients across the region was 47.5% (n = 77). This availability rate increased to 57.4% for an appointment within 48 hours of the call, almost 60% within three days, and 70% were met within 10–15 days (Table 1).
Thirty-six clinics (22.2%) offered an appointment on a different day, with a mean wait time of 3.6 days (standard deviation [SD]: 3.3 days). Almost 20% of practices could not offer an appointment at all (n = 31; 19.1%). The main reasons given were that the clinic was not taking new patients (n = 14) or the practice was fully booked (n = 7).
The telephone was not answered (ie rang out, diverted to a message service) in 10.5% of the clinics (n = 17). The reasons for the phone being unanswered were varied, including disconnected (n = 4) and answer machine message diverting patients (n = 6).
There were wide variations in the number of practices and same-day availability throughout the region by local government area; the median number of practices per local government area was 11 (range: 1–27). Same-day availability rate per local government area ranged from 11% to 63%, with an average of 42.2% and median of 43.8% (Table 2; Figure 1). The overall availability rate of a female GP was 30.2% (n = 49); this ranged from 0 to 50% (Table 2).
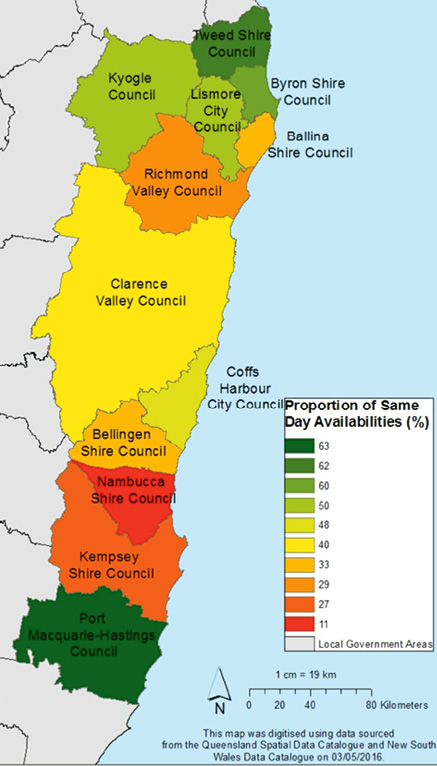
Figure 1. Proportion of same-day appointments for general practices by local government area
Bulk billing rates ranged from 0 to 50% of all practices in this study, with a median of 21% (n = 34). For practices taking appointments and not bulk billing (n = 78), the average out-of-pocket expenses after the MBS rebate was $29.98 (range: $12.95–60.30).
Table 1. General practice responses to new patient appointment request and number of days to next available appointment
|
General practice appointments
|
n
|
%
|
Cumulative %
|
|---|
|
Same-day appointment was available
|
77
|
47.5
|
47.5
|
|
Same-day walk-in (without appointment) was offered
|
1
|
0.6
|
48.2
|
|
Next-day appointment was available
|
15
|
9.26
|
57.4
|
|
Next-available appointment was available in:
|
|
|
|
|
2 days
|
3
|
1.9
|
59.3
|
|
3 days
|
4
|
2.5
|
61.7
|
|
4 days
|
5
|
3.1
|
64.8
|
|
5 days
|
2
|
1.2
|
66.1
|
|
7 days
|
2
|
1.2
|
67.3
|
|
8 days
|
1
|
0.6
|
67.9
|
|
9 days
|
2
|
1.2
|
69.1
|
|
10 days
|
1
|
0.6
|
69.8
|
|
15 days
|
1
|
0.62
|
70.4
|
|
No appointment was available for new patients
|
31
|
19.1
|
89.5
|
|
Phone not answered (ie missing data)
|
17
|
10.5
|
100
|
|
Total
|
162
|
100
|
100
|
Table 2. Proportion of new patient same-day appointment availability and bulk billing across 12 local government areas in regional New South Wales
|
Name of local government area
|
Number of
practices (N)
|
Same-day access
to GP (%)
|
Same-day access
to female GP (%)
|
Bulk billing (%)
|
|---|
|
Ballina
|
9
|
33.3
|
22.2
|
0.0
|
|
Bellingen
|
6
|
33.3
|
16.7
|
33.3
|
|
Byron
|
15
|
60.0
|
33.3
|
6.7
|
|
Clarence Valley
|
15
|
40.0
|
20.0
|
20.0
|
|
Coffs Harbour
|
21
|
47.6
|
38.1
|
14.3
|
|
Kempsey
|
11
|
27.3
|
18.2
|
27.3
|
|
Kyogle + Tenterfield
|
2
|
50.0
|
0.0
|
50.0
|
|
Lismore
|
14
|
50.0
|
50.0
|
21.4
|
|
Nambucca
|
9
|
11.1
|
0.0
|
11.1
|
|
Port Macquarie – Hastings
|
27
|
63.0
|
44.4
|
37.0
|
|
Richmond Valley
|
7
|
28.6
|
14.3
|
0.0
|
|
Tweed
|
26
|
61.5
|
30.8
|
26.9
|
|
Overall total
|
162
|
47.5
|
30.2
|
21.0
|
|
Average by local government area
|
13.5
|
42.2
|
24.0
|
20.7
|
|
Median by local government area
|
12.5
|
43.8
|
21.1
|
20.7
|
|
*Tenterfield was combined with Kyogle because the Tenterfield practice was on the border of Kyogle and was frequented by residents in the Kyogle, and both only had one practice listed
|
Discussion
The current study found that a new adult patient selecting a medical practice at random in regional, north-eastern New South Wales had a 70% chance of getting an appointment with a GP within two weeks, but a 30% chance of not getting anything. The probability of seeing a GP on the same day in north-eastern New South Wales was less than 50% (47.5%) for any GP and only 30.2% for a female GP. This was highly variable across different local government areas. The lowest appointment availability rate was 11%, but even the highest (61.5%) was well below that found in a recent Melbourne-based study that included metropolitan and regional areas. Freed et al8 found a 78% probability of getting an appointment for a child to see a doctor on the same day. However, a child with an infection may be prioritised, making a direct comparison speculative.
Another key finding was that only one in five practices (21%) offered bulk billing. The Melbourne-based study found that 75% of the clinics contacted offered bulk-billing services.8 According to MBS statistics for 2015–16, the Australian bulk‑billing rate for attendance to a GP was 83.7%, with Victoria close to the average (83.1%); however, New South Wales had a higher than average rate (87.7%).9 The region in New South Wales covered by this study fell well short of these figures. This may partially be explained by the new patient status presented in the scenario. Bulk-billing services may be lower for new patients, and this effect may be obscured by grouping all patients together. Future MBS statistics could perhaps include a subcategory for new patients to facilitate future targeted planning for the anticipated increases to the populations in regional areas (eg ‘sea-changers’, ‘tree-changers’).
When bulk billing is not available, an additional payment is required by the patient. This out-of-pocket expense ranged widely from region to region in this study, averaging at $30. This was less than the state average of $32.6 and national average of $33.4.9 Cost has been found to be a major barrier for people needing to access primary care. A study of a representative sample (n = 400) of Western Australian residents in an outer metropolitan area found that difficulty getting an appointment (58.8%) and appointment costs (24.5%) were the two biggest reasons preventing access to primary care (n = 516 responses, multiple responses were allowed).7 Across all primary health networks in Australia, the percentage of adults who delayed seeing a GP because of cost has been found to range from 2% in the central and eastern suburbs of Sydney to 9% in the Murray area. In a national patient experience survey, the proportion of people who waited longer than they felt was acceptable for an appointment in 2015 was 19%.10
Regional GPs face particular clinical and service delivery challenges. The health service population needs in regional Australia are exacerbated by a large proportion of low-income households, and people on disability or sickness and unemployment benefits,11 and an ageing population.12 The limited supply in the health workforce and ageing GP workforce13 compounds the population demographics and high chronic disease rates.14 Almost half of older GPs in the Northern Rivers region in New South Wales are planning to retire before the traditional retirement age of 65 years.13
Health services reform is part of the New South Wales Rural Health Plan, which aims to improve access to health services as close to home as possible.14 Despite the fact that the New South Wales government has increased investment in rural health services over the past few years,14 findings from this study suggest further improvements are required to facilitate easier access to primary healthcare for regional areas, particularly for first-time patients. With 80% of people who recently attended an emergency department citing the lack of GP availability when needed as the major reason for attending, there is a possibility that increasing GP availability would decrease attendance to emergency departments.7 Indeed, in 2014–15, eight of the 12 local government areas in this study had higher than state average hospitalisations rates.15 Further research is required to identify how patients make decisions about whether they would attend general practice or emergency department for non-urgent conditions.
This study had some methodological limitations. As a cross-sectional study, the data were collected at one point in time. The period of data collection was outside of school holidays, but factors such as GP leave could not be controlled. Indeed, a follow-up study could determine the stability of GP availability over time. Another limitation was that the scenario was based on a new patient. Perhaps, it would be easier for an existing patient of the practice to see a GP on the same day. Some of the clinics advised that new patients were required to attend a longer consultation, which may have reduced the availability of a same-day appointment and increased costs. Future studies should collect data on whether a longer consultation was required so that a sensitivity analysis could check whether this factor is likely to inflate appointment availability. In addition, data were not collected about the size of the practices or how many doctors were available in each practice. A useful future study would explore the ratio of patients to GPs with availability and bulk-billing rates.
A major strength of the study was that it was a census with a high response rate and, as such, is the highest level of evidence (Level 1) for a prevalence study.13 That is, every practice was included in the sampling frame, with a high contact rate (90%; ie only 10% of clinics could not be contacted in the randomised sequence). Therefore, these findings are representative of those living in north-eastern New South Wales. Given the extent of the variation in appointment availability rates and departure from those found in the Melbourne-based study8 and MBS statistics,9 these findings should not be used to make estimates about appointment availability to populations beyond the regions included in the study (eg neighbouring regions, more remote or interstate regions, metropolitan areas). Another strength of this study was that it did not rely on self-report or memory recall methods, which may introduce reporting bias. This cross-sectional census method could be applied to different locations, patient groups and clinical conditions.
Conclusion
New patient appointment availability for primary healthcare in northern New South Wales varies widely from region to region. Areas with longer waiting times could be targeted for additional attention from policy makers, such as GP workforce shortages or alternative healthcare models that may increase access to primary healthcare. This cross-sectional census method can be readily implemented to receive rapid feedback about service availability and patient out-of-pocket expenses for patients at the local level.
Implications for general practice
Despite northern New South Wales being an area with higher rates of chronic illness and an ageing population, there was limited access to affordable, same-day GP appointments, especially for female GPs. Improving the availability of primary healthcare services may reduce non-urgent use of emergency department services.
Authors
Joanne Bradbury BA, BNat (Hons), PhD, Lecturer, Evidence-Based Healthcare, Southern Cross University, Gold Coast, QLD
Susan Nancarrow BAppSc (Pod), MAppSc, PhD, Professor of Allied Health and Chair of the Academic Board, Southern Cross University, Gold Coast, QLD
Cathy Avila DipNat (SCNT&TCM), BSc (Hons), PhD, Lecturer, Exercise and Nutritional Biochemistry, Southern Cross University, Lismore, NSW
Sabrina Pit PhD, MSc, DipOHS, GradCert Teaching-Higher Ed, Workforce Research Stream Leader, University of Sydney, and Lead Academic, Clinical and Educational Research, University Centre for Rural Health, Western Sydney University, Sydney University, Lismore; NSW; Southern Cross University, Gold Coast, QLD
Ruth Potts, PhD, BUrb&EnvPlan (Hons), Lecturer, Regional and Urban Planning, Southern Cross University, Lismore, NSW
Frances Doran, BSocSc, GradCert (HE), MSocSc, PhD, Senior Lecturer, Nursing, Southern Cross University, Lismore, NSW
Gary Freed, MD, MPH, Professor of Population Health, University of Melbourne; and Professor of Paediatrics and Public Health, University of Michigan, USA
Competing interest: None
Provenance and peer review: Not commissioned, externally peer reviewed
Acknowledgements
We would like to acknowledge North Coast Primary Health Network (NC PHN) for their support in this project and thank the many kind and caring medical receptionists at the general practices who we spoke to in relation to this study.
Funding was received from Southern Cross University, Division of Research, Seed grant funding.