Case
A healthy woman aged 19 years was sent to the general hospital in Malaysia by her family physician for a routine medical check-up, as this was a prerequisite for admission to a university graduate course. She was asymptomatic. She did not complain of cough, breathlessness, fever, night sweats, loss of appetite or loss of weight. On examination, vital signs were normal. Her height was 157 cm and she weighed 54 kg. On local examination of the chest, her trachea was shifted significantly to the left side, and the left hemithorax moved less on inspiration, compared with the right. The apex beat was felt in the fifth left intercostal space at the anterior axillary line. Percussion note was dull over the left hemithorax, and auscultation revealed diminished air entry over the entire left chest, anteriorly and posteriorly, with diminished vocal resonance over the same area. The right side was normal. No surgical scars were seen over the chest wall and there was no past history of surgery. The rest of the clinical examination was normal. A chest radiograph (posterioranterior view) showed a diffuse opacity over the entire left hemithorax with the trachea shifted to the left side (Figure 1).
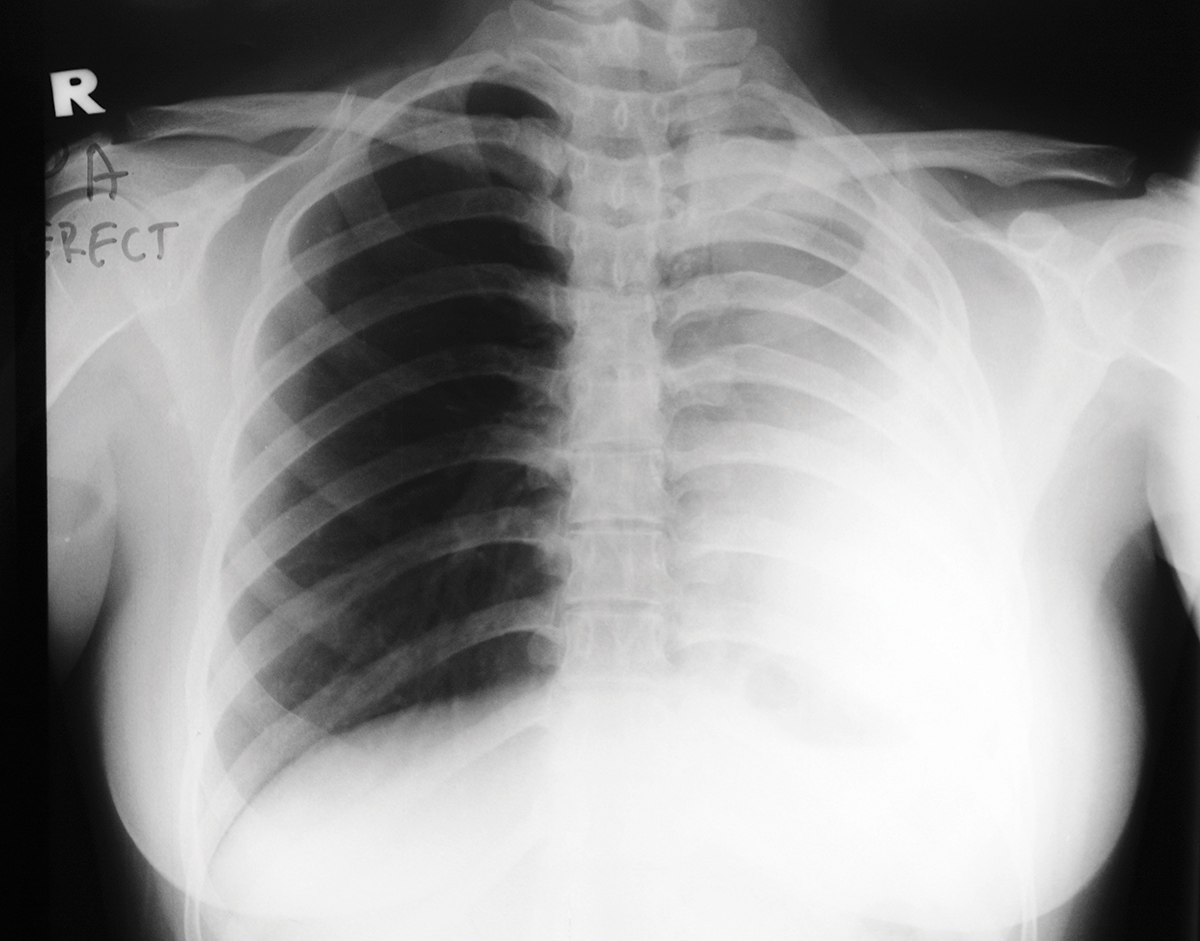
Figure 1. Chest radiograph showing a diffuse opacity over the left hemithorax with a significant tracheal shift to the left side
Question 1
What are the main causes of tracheal deviation?
Answer 1
The main causes of tracheal deviation can be categorised as follows:
- congenital – pulmonary aplasia or agenesis
- malignant – bronchogenic carcinoma (large tumour mass), massive pleural effusion, pulmonary atelectasis, large mediastinal mass (eg malignant lymphoma)
- surgical – pneumonectomy, lobectomy
- infections – pleural effusion (eg pulmonary tuberculosis, bacterial infection), empyema (eg bacterial and anaerobic infections)
- traumatic – severe lung contusion, haemothorax.
Case continued
Pulmonary atelectasis was suspected and a chest computed tomography (CT) scan with contrast was done. It showed complete absence of lung parenchyma on the left side, transmediastinal herniation of the right lung into the left thoracic space (Figure 2, green arrows), and complete absence of the carina and left main-stem bronchus (Figure 2, red arrow). On coronal view of the chest CT scan, the trachea and right main stem bronchus appeared as a single ‘pipe-like structure’, with complete absence of the carina and left main stem bronchus. Only a small indentation was seen at the site of the carinal bifurcation (Figure 3, red arrow).
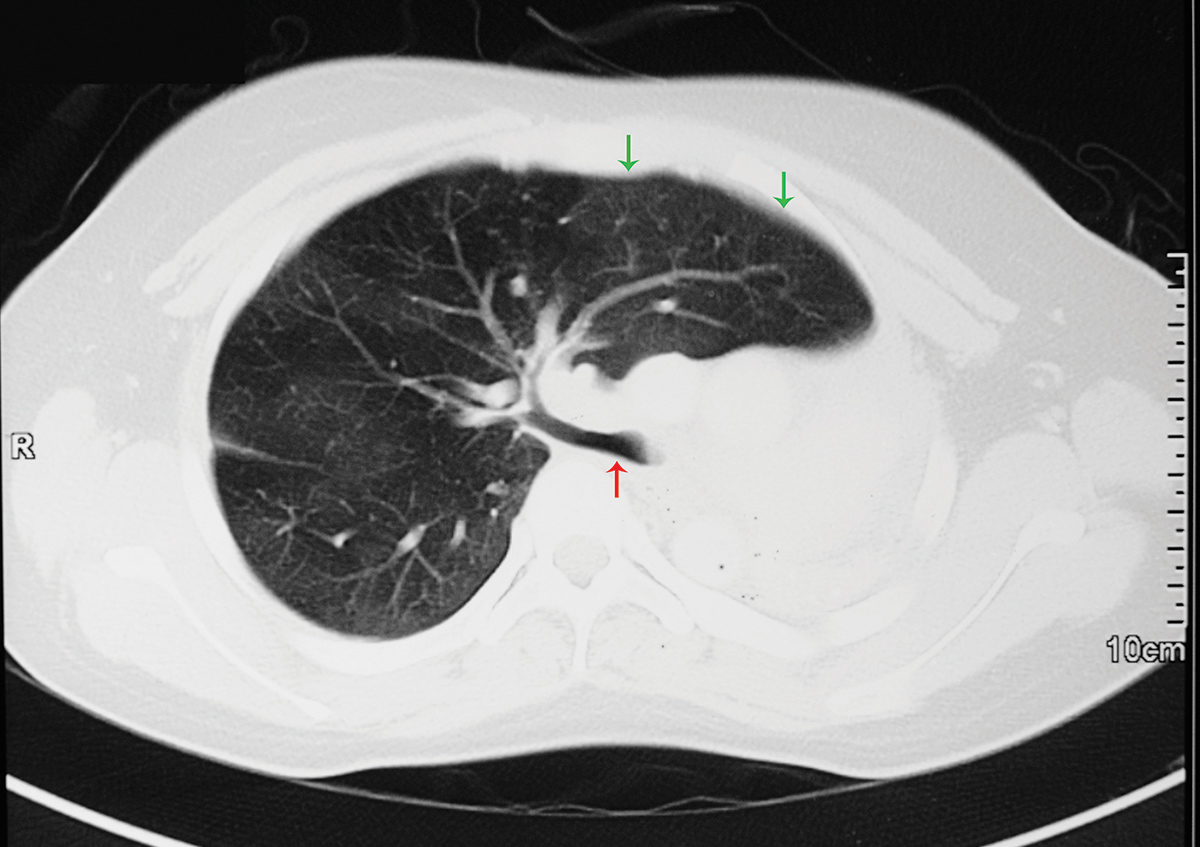
Figure 2. CT chest scan showing complete absence of lung parenchyma on the left side with transmediastinal herniation of the right lung into the left thoracic space (green arrows), and a complete absence of the carina and left main-stem bronchus (red arrow)

Figure 3. Coronal view of the chest CT scan showing the trachea and right main stem bronchus as a single ‘pipe-like structure’, with complete absence of the carina and left main stem bronchus. A small indentation is seen at the site of the carinal bifurcation (red arrow)
Question 2
What is the most likely diagnosis in this patient?
Answer 2
The most likely diagnosis is pulmonary agenesis, which is a very rare condition.1 It was first described by De Pozze, who discovered it by accident during an autopsy on an adult female in 1673.2 Pulmonary agenesis is characterised by complete absence of the carina, main-stem bronchus, pulmonary parenchyma and pulmonary artery on the affected side, and is usually accompanied by transmediastinal herniation of the healthy lung into the thoracic space on the side of agenesis.3 Consequently, in the absence of any past history of surgery, the findings were highly suggestive of pulmonary agenesis on the left side.
Case continued
Videobronchoscopy was done and showed complete absence of the carina and left main stem bronchus, while the right side was normal. This, therefore, confirms the diagnosis of left pulmonary agenesis. Echocardiography was normal, with no structural cardiac defects noted.
Question 3
What is the treatment for this condition?
Question 4
What are the complications associated with this condition?
Question 5
What are the congenital anomalies associated with this condition?
Answer 3
Treatment for pulmonary agenesis is usually conservative, with chest physiotherapy and antibiotics to treat any underlying pulmonary infection on the normal side.4 Curative surgery is usually reserved for co-existent congenital abnormalities, if present.
Answer 4
Complications of pulmonary agenesis include:
- pulmonary hypertension
- repeated infections of the contralateral lung
- compensatory emphysema of the contralateral lung.
Answer 5
The most commonly associated congenital anomalies include structural cardiothoracic defects such as atrial and ventricular septal defects, patent foramen ovale, tetralogy of fallot, diaphragmatic hernia and tracheal stenosis; gastrointestinal anomalies such as oesophageal atresia with or without tracheoesophageal fistula, pyloric stenosis and duodenal atresia; and limb anomalies such as bifid thumb and polydactyly.5,6
Key points
- Careful physical examination along with radiological and bronchoscopic investigations form the cornerstone in the identification of rare and unexpected pathologies, such as pulmonary aplasia and pulmonary agenesis.
- In pulmonary agenesis, the contralateral healthy lung may develop twice as many alveoli as normal in response to the agenesis, resulting in transmediastinal herniation of the healthy lung into the thoracic space on the side of agenesis.
- Pulmonary agenesis may be associated with congenital anomalies, such as structural cardiothoracic, gastrointestinal, genitourinary and musculoskeletal defects.
- Rarely, some patients with pulmonary agenesis may remain completely asymptomatic and healthy and reach early adulthood without ever being diagnosed.
Authors
Rumi R Khajotia MD (Bom), MD (Vienna), FAMA (Vienna), FAMS (Vienna), Consultant Respiratory Physician, Hospital Tuanku Ja’afar, Seremban, Malaysia; Associate Professor in Respiratory Medicine, International Medical University, Seremban, Malaysia. rkhajotia2015@gmail.com
Sree Raman MBBS, FRCP (UK), Senior Consultant Physician, Hospital Tuanku Ja’afar, Seremban, Malaysia
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.