Physiotherapists are the fifth largest health workforce group in Australia. In 2014, there were 11,608 full-time equivalent physiotherapists working in private practice.1,2 In Australia, physiotherapists have been first-contact primary healthcare professionals since 1976.1 A 2010 survey conducted by the Australian Physiotherapy Association found that 71% of patients treated by private practitioner physiotherapists had self‑referred.2 Physiotherapists also receive referrals from other health professionals, such as general practitioners (GPs).
There are limited published Australian data about the extent to which GPs formally refer patients to physiotherapists and whether this has changed over time. The Bettering the Evaluation and Care of Health’s (BEACH’s) A decade of Australian general practice activity 2005–06 to 2014–15 reported that overall referrals to allied health professions increased by 65% from 2005–06 to 2014–15, largely driven by increased referrals to psychologists. Further, the report showed that nationally, there were 810,000 more GP referrals to physiotherapists in 2014–15 than a decade earlier. The rate of referral to physiotherapists increased by about 25%, from 1.1 per 100 encounters (95% confidence interval [CI]: 1.0, 1.3) in 2005–06 to 1.4 per 100 encounters (95% CI: 1.3, 1.6) in 2014–15.3
In 2004, items for a limited number of allied health services (10950–10970) were added to the Medicare Benefits Schedule (MBS) for people with a chronic disease management plan.4 A further MBS item number was added in 2011 for the physiotherapy assessment of children with a disability (82030).
Analysis of MBS claims data from 2005 to 2009 found an increase in claims for all allied health services, with a threefold increase for physiotherapy.5 A qualitative study explored whether access to allied health services changed as a result of the MBS item numbers for chronic disease. There was some evidence that access had increased for the most disadvantaged peoples, but they were unable to continue with treatment once they used the five sessions subsidised by MBS. Those with the ability to pay were able to continue treatment after they used the subsidised sessions.6 Neither publication detailed demographic characteristics of patients and the common problems referred by GPs to MBS-funded care by physiotherapists.
The aims of this study were to assess changes in the rate of GP referral to physiotherapists in Australia from 1998 to 2014, and to determine patient characteristics associated with increased likelihood of such referral.
Methods
This study is a secondary analysis of data from the BEACH program, the methods of which have been described in detail elsewhere.7,8 For this study, we used annual weighted encounter data from 1998–99 to 2014–15 inclusive, and encounters where a referral to a physiotherapist was made were identified. This was to measure the referral rate to physiotherapy per 1000 GP encounters per year before and after the introduction of allied health MBS items in 2004 and the MBS item for allied health assessment of disability in children in 2011.
The annual referral rate per 1000 GP encounters per year was then extrapolated (methods previously described)3 to estimate the number of GP encounters nationally where the patient was referred physiotherapy. The number of individuals who visited a GP at least once in a given year (attending population) was calculated from summary MBS data supplied by the Department of Health.3 The referral rate per 1000 attending persons was calculated as total referrals divided by total attending population.
Investigation of the types of problems referred and characteristics of those referred was limited to a subset of recent BEACH data recorded between April 2010 and March 2015. Patient characteristic-specific rates of referral to physiotherapy by GPs were calculated. The problem(s) referred were classified according to the International Classification of Primary Care – Version 2 (ICPC-2).9 For this paper, the coded problems were grouped by ICPC-2 chapters, which relate to body systems.7
The BEACH study was approved by the ethics committees of the University of Sydney and the Australian Institute of Health and Welfare (ref: 2012/130).
Results
There were 1,668,060 GP–patient encounters recorded in the 17 data years between 1998 and 2015 (approximately 100,000 per year). The rate of referral from GPs to physiotherapy increased significantly from 9.2 (95% CI: 8.3, 10.1) per 1000 encounters in 1998 to 14.4 (95% CI: 13.1, 15.7) in 2014 (Figure 1). However, most of this increase occurred in the five years from 2009–10 to 2014–15. There was no statistically significant immediate growth from the introduction of the allied health MBS items in 2004 to 2009. As a rate per 1000 attending persons, the annual rate of referral increased significantly by about 50%, from 62.6 (95% CI: 56.5,68.6) in 2000 to 97.9 (95% CI: 88.9,106.7) in 2015 (Figure 2).
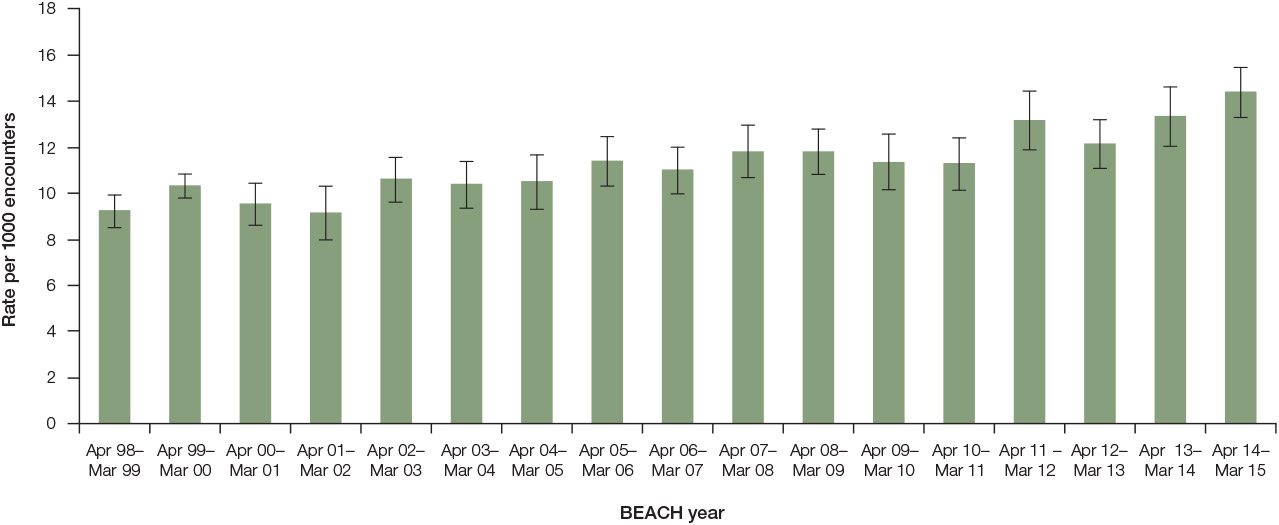
Figure 1. Rate of referral to physiotherapy per 1000 GP encounters by year (1998–99 to 2014–15; bars are 95% confidence interval)
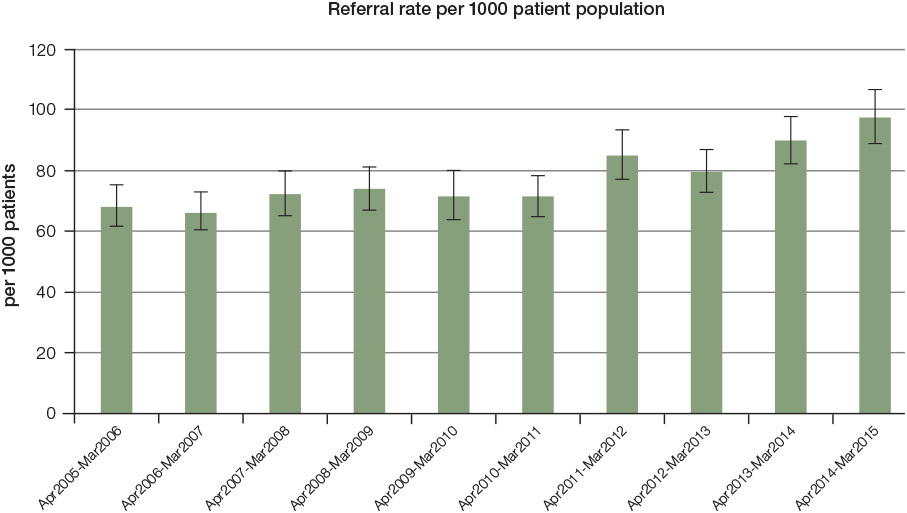
Figure 2. Referral rate to physiotherapy per 1000 patient population (bars are 95% confidence interval)
A number of patient characteristics were associated with referral to physiotherapy (Figure 3). The likelihood of referral was significantly higher at encounters with patients who:
- held a Department of Veterans’ Affairs (DVA) card (2.1 per 100 encounters; 95% CI: 1.9, 2.4) than those who did not (1.4 per 100 encounters; 95% CI: 1.3, 1.4)
- did not hold a Health Care Card (HCC; 1.5 per 100 encounters; 95% CI: 1.4, 1.6) than for those who did (1.2 per 100 encounters; 95% CI: 1.2, 1.3)
- were previously seen at the practice (1.4 per 100 encounters; 95% CI: 1.4, 1.5) than new patients to the practice (0.97 per 100 encounters; 95% CI: 0.9, 1.1).
This pattern of referral was reflected to some degree in the socioeconomic status (SES) of patients who were referred to physiotherapy, with those from low SES marginally less likely to be referred 1.3 per 100 encounters (95% CI: 1.2, 1.4) than those from a high SES 1.5 per 100 encounters (95% CI: 1.4, 1.5).
Overall, females were more likely to be referred to physiotherapy than males, but there were also differences in specific sex–age groups. Among males, those aged 25–44 years were significantly more likely to be referred than all other male age groups. Among females, those aged 45–64 years (1.9 per 100 encounters) and 65–75 years (1.6 per 100 encounters) were significantly more likely to be referred than other female age groups.
The vast majority (80%) of all physiotherapy referrals were for musculoskeletal problems, but referral was only made on 6.8% of all occasions of musculoskeletal problem management in general practice (Table 1). Neurological problems were referred on 2% of all occasions managed, accounting for only 5% of all referred problems. While respiratory problems are very frequently managed by GPs, referrals to physiotherapy for these problems accounted for less than 1% of the total.
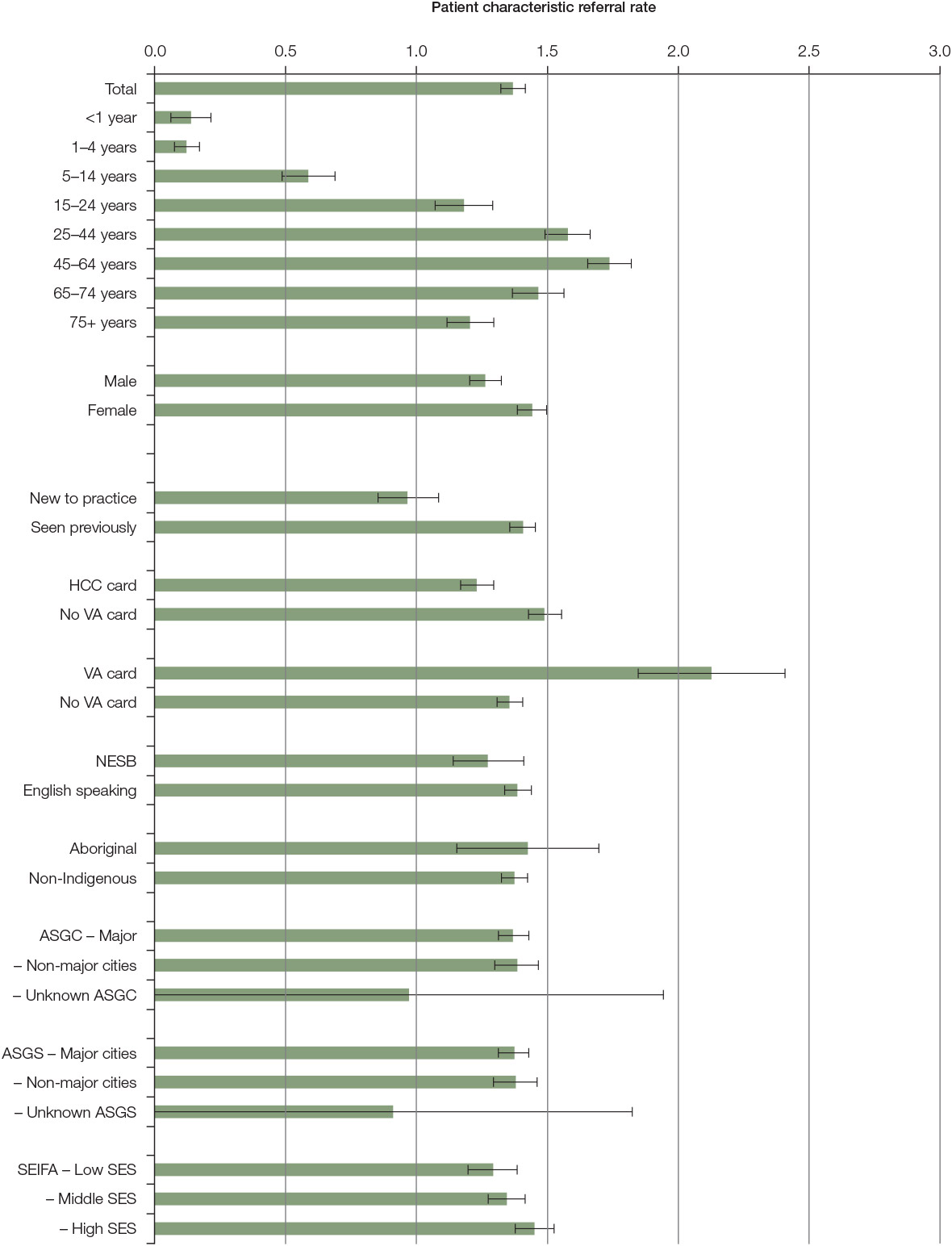
Figure 3. Patient characteristic-specific referral rates to physiotherapy per 1000 encounters
ASGC, Australian Standard Geographical Classification; HCC, Health Care Card holder; Major cities (class 1), Not major cities (classes 2–6 inclusive); NESB, non-English speaking background (patient self-reported, speaks a language other than English as their primary language at home); SEIFA, Socio-Economic Indexes for Areas (based on postcode of patient residence; Low SEIFA, quintiles 1–3; middle SEIFA, quintiles 4–7; high SEIFA, quintiles 8–10); SES, Socioeconomic status; VA, Veterans Affairs’ card holder
Discussion
The rate of referral by GPs to physiotherapists increased significantly from 1998 to 2015, particularly 2009 onwards. Changes to the MBS items for allied health occurred on two occasions, and the more substantial growth in referrals occurred after the second change. Cant et al reported that uptake of general practice management plans (GPMP) and team care arrangements (TCA) was low up to June 2009,5 and TCA is required in order for patients to access MBS items for physiotherapy.
Currently, patients are only eligible for a TCA and GP referral to physiotherapy if they have a chronic or terminal illness and complex care needs. Clearly, there has been an increase in referrals to physiotherapy following the introduction of TCA and the allied health MBS item for childhood disability assessment. However, this study found that many of the problems managed by GPs were musculoskeletal problems, and only a small proportion of these problems were referred to physiotherapy. If patients with musculoskeletal problems do not meet the requirements for TCA, there are limited referral options for those who cannot afford private physiotherapy. GPs can refer patients to public hospital outpatient physiotherapy, but often there are lengthy waiting lists. Patients may be willing to pay for physiotherapy treatments that are known to be effective following discussion and advice from their GP. Further policy and MBS changes may be required to improve access to evidence-based physiotherapy for the many people with musculoskeletal problems presenting to general practice who are not referred to physiotherapy.
Patients were more likely to be referred to physiotherapy if they held a DVA card or did not hold a HCC. GPs may be less willing to refer patients holding a HCC to private physiotherapy because they may perceive that these patients would be less able to pay the differential cost of the treatment. Conversely, patients with a DVA card were more likely to be referred because physiotherapists are not allowed to charge a co-payment for DVA patients, so the treatment is free to the patient.
In Australia, most (61%) physiotherapists work in the private sector,10 and out-of-pocket costs have been increasing steadily as the fees have increased at a greater rate than MBS rebates. This means access to physiotherapy interventions in private practice is increasingly dependent on the ability to pay. There is evidence that patients without private health insurance or the financial means to pay for physiotherapy may be more likely to access physiotherapy via a TCA.6 This would require a GP consultation to facilitate the referral. A qualitative study of allied health professionals providing interventions through the allied health MBS item numbers found that patients who are the most disadvantaged were still not able to access care because of the gap fee charged. Further, patients who are advantaged were better able to continue allied health treatments after the funded physiotherapy treatments had been used.6 The data presented here suggest GPs may be less likely to refer the more disadvantaged to physiotherapy.
Table 1. Problems managed by ICPC-2 chapter and referral to physiotherapy
|
Problem managed
(ICPC-2 chapter level)
|
Management frequency (n)
|
Number of times problem referred to physiotherapy (n)
|
Referral rate to physiotherapy* (%)
|
Lower 95% confidence interval (CI)
|
Upper 95% CI
|
All problems referred to physiotherapy (%)
|
|---|
|
Musculoskeletal
|
85,988
|
5,521
|
6.79
|
6.54
|
7.04
|
79.97
|
|
Neurological
|
18,855
|
350
|
1.93
|
1.7
|
2.15
|
5.07
|
|
General & unspecified
|
100,109
|
309
|
0.36
|
0.31
|
0.41
|
4.48
|
|
Skin
|
84,824
|
188
|
0.23
|
0.19
|
0.27
|
2.72
|
|
Urology
|
17,438
|
99
|
0.6
|
0.47
|
0.72
|
1.43
|
|
Endocrine and metabolic
|
66,719
|
82
|
0.15
|
0.11
|
0.18
|
1.19
|
|
Female genital system
|
32,408
|
79
|
0.29
|
0.22
|
0.36
|
1.14
|
|
Respiratory
|
92,992
|
77
|
0.09
|
0.06
|
0.11
|
1.12
|
|
Circulatory
|
81,922
|
59
|
0.08
|
0.06
|
0.1
|
0.85
|
|
Ear
|
18,357
|
55
|
0.31
|
0.22
|
0.39
|
0.80
|
|
Psychological
|
67,887
|
31
|
0.05
|
0.03
|
0.06
|
0.45
|
|
Digestive
|
54,530
|
21
|
0.04
|
0.02
|
0.06
|
0.30
|
|
Pregnancy and family planning
|
20,570
|
16
|
0.08
|
0.04
|
0.13
|
0.23
|
|
Blood
|
8,470
|
10
|
0.13
|
0.05
|
0.21
|
0.14
|
|
Male genital system
|
8,715
|
4
|
0.05
|
0
|
0.09
|
0.06
|
|
Social
|
4,750
|
3
|
0.06
|
0
|
0.13
|
0.04
|
|
Eye
|
11,359
|
0
|
0
|
0
|
0
|
0.00
|
|
Total problems
|
775,893
|
6,904
|
0.89
|
0.86
|
0.92
|
100
|
|
*For each chapter, the proportion of all GP occasions of management that resulted in a referral to physiotherapy
|
The majority of patients seen by private physiotherapists in Australia are not referred by their GP,2 and the characteristics of this self-referred population may differ from patients who are referred. There are no Australian data available to describe characteristics of patients managed by private physiotherapists, but international studies have compared characteristics of referred and self-referred patients. A trial of self-referral to physiotherapy in Scotland11 found that patients from more socioeconomically deprived areas were more likely to be referred to physiotherapy by their GP, and those from more affluent areas were significantly more likely to self-refer. However, it was not clear if there was a charge made to the patient for physiotherapy treatment. A Danish study of GP referral to physiotherapy found wide variation in referral rates from the practices surveyed. It also found that female GPs referred more often to physiotherapy;12 however, the impact of SES of the practices on referral rates was not discussed. The results of the Danish study suggest that awareness of physiotherapy and regular contact with a physiotherapist are likely to have an impact on GP referrals.
The introduction of the allied health MBS items for chronic disease has resulted in increased access to physiotherapy services.5 However, other studies have highlighted continued inequity in access to allied health, such as physiotherapy for people with chronic conditions.6 Musculoskeletal problems accounted for the vast majority of referrals, although, it was only referred on 6% of management occasions. It is not clear from the data if the wider promotion of the range of clinical problems that can be effectively treated by physiotherapy to GPs and the general public would be beneficial. Providing GPs with more information about the types of conditions with effective evidence-based physiotherapy interventions, such as The Royal College of General Practitioners’ (RACGP’s) HANDI resources, may be helpful in discussions with patients and increase the likelihood of referral.
The differences in referral rates to physiotherapy by patient age and gender are interesting, females being more likely to be referred to physiotherapy than males. The highest rate of referral was for women aged 45–64 years, but for males, it was those aged 25–44 years. In general, more females present to general practice at least once per year in all age groups.7,13 A study of the management of adolescent injuries found that as girls reached the 15–19‑year age group, they presented with fewer injuries and the number of consultations related to reproductive health increased.14 It is feasible that this pattern continues until they reach menopause. By contrast, for males aged 25–44 years, the proportion attending general practice is 71%, compared with 86% for females of the same age, and 65% of the encounters are for a new problem.13 The number of male GP encounters is almost half that of females, but the proportion referred to physiotherapy is higher. It is likely that males are presenting with new problems as a result of sport-related or work-related injuries. International studies have reported that males have an increased incidence of soft-tissue injuries15 and serious work-related injuries,16 compared with women. By contrast, a study of musculoskeletal presentations in general practice in the UK found a higher rate of presentations by women than men in all age groups, but they did not report on the rate of referral to physiotherapy.17
Limitations
Self-referral to physiotherapy has been available in Australia since 1976.1 Once referred to a physiotherapist, patients may be more likely to self-refer with future episodes or a new condition. The data presented here only provide information on GP referrals to physiotherapy and not patterns of referral or attendance at physiotherapy over time.
Future research might explore the decisions Australian GPs make about who they refer for physiotherapy and what influences this decision.
Conclusion
The rate of GP referral to physiotherapists has increased steadily and significantly since the late 1990s, particularly after the second MBS item changes made for some coverage of services provided to those referred by a GP. Patient characteristics that increase the likelihood of referral include the ability to pay or have financial cover for costs, and specific age and gender groups.
Implications for general practice
GPs appear less likely to refer patients who are more disadvantaged to physiotherapy. Maximising the use of TCAs for eligible patients could increase access to physiotherapy for those who cannot afford to pay for private treatment. Patients may be willing to pay for physiotherapy following discussion with their GP.
Authors
Sarah Dennis Grad Assoc Phys, MSc, PhD, Associate Professor of Allied Health, Faculty of Health Sciences, University of Sydney; South Western Sydney Local Health District, NSW. sarah.dennis@sydney.edu.au
Ian Watts BSW, BArchDes, MBA (Exec), Manager, Policy and Industrial Relations, Australian Physiotherapy Association, Hawthorn, Vic
Ying Pan BMed MCH, (formerly) Senior Research Analyst, Family Medicine Research Centre, Sydney School of Public Health, University of Sydney, NSW
Helena Britt BA PhD, (formerly) Director, Family Medicine Research Centre, Professor of Primary Health Research, Sydney School of Public Health, University of Sydney, NSW
Competing interest: None.
Provenance and peer review: Not commissioned, externally peer reviewed.