Recent media reports have cited substantial growth in annual reimbursements for Medicare Benefits Schedule (MBS) item number 597 for urgent, sociable after-hours consultations. Between 2010 and 2015, expenditure from MBS item number 597 increased from $91 million to $195 million. The increase in the number of after-hours medical deputising services (AHMDSs) and associated marketing campaigns have been suggested as key drivers of this growth.1
Specific MBS item numbers are available to support general practitioners (GPs) and non-vocationally registered doctors (employed by AHMDSs) to provide after-hours care. After-hours is defined as consultations occurring outside 8.00 am to 6.00 pm on weekdays and 8.00 am to 12.00 pm on Saturdays, and at any time on Sundays and public holidays. Claims are based on urgency, time of day and location of the service provided. For urgent, after-hours care, two items are available, depending on the timing of the consultation (ie whether or not outside 11.00 pm to 7.00 am, or unsociable hours; Table 1). For non-urgent, after-hours attendances, eight items are available on the basis of duration and location of consultation.
AHMDSs have been established in many urban and metropolitan centres across Australia. The exact number of services is difficult to ascertain; however, in a recent review of after-hours care, it was estimated that this had increased from 16 in 2006 to 83 in 2014.2 In addition, there has been an increase in the number of jurisdictions in which AHMDSs provide services. For example, AHMDs were established in the Australian Capital Territory in August 2014,3 Tasmania in early 20154,5 and the Northern Territory (Darwin) in November 2015.6 Furthermore, advertisements for bulk‑billed, after-hours home visiting medical services have become common in recent years. Of note, however, is that the guidelines pertaining to AHMDSs prohibit advertising to promote ‘routine’ or convenience-based medical services as they are unable to provide comprehensive GP care.7
The aim of this study was to assess national and jurisdictional (states and territories) changes in claims for all MBS after-hours items for GPs (excluding care provided in consultation rooms and residential aged care facilities [RACFs]).
Method
MBS claims data were extracted from the Medicare Australia statistics dataset for all after-hours GP item numbers (Table 1). Data were extracted by item number, jurisdiction and financial year using the ‘Medicare Items Statistics Reports’ webpage.8 Data were extracted into Microsoft Excel for Windows. A time series was created for each MBS item number and jurisdiction, for the 2010–11 to 2015–16 period. Analysis was conducted on the numbers of claims nationally for all MBS after-hours item numbers (ie 597, 599, 5003, 5023, 5043, 5063), and per capita rates of claims for MBS item number 597 for states and territories.
Tasmanian public hospital emergency department data were supplied by the Tasmanian Department of Health and Human Services for the 2010–11 to 2015–16 period. These data were provided by acuity, using the Australian Triage Scale.9 As one of the main tenets of AHMDS is that these reduce emergency department presentations,10,11 a comparison of the claims for MBS item number 597 and public hospital emergency department presentation data was conducted. The quantified analysis method compared claims for MBS item number 597 with all emergency department presentations and low acuity presentations over the 2010–11 to 2015–16 period. Low acuity presentations were defined as triage categories 4 and 5 on the Australian Triage Scale.9
Results
National and jurisdictional MBS claims data
Figure 1 provides a national overview of MBS item numbers for after-hours GP consultations for the 2010–11 to 2015–16 financial years. The number of claims for MBS item 597 – urgent, sociable after-hours consultation – increased by 170%, from 562,497 in 2010–11 to 1,516,916 in 2015–16. For MBS item 599 – urgent, non-sociable after-hours consultation – a 106% increase was observed, from 125,025 claims in 2010–11 to 257,774 in 2015–16. While the absolute number of claims for MBS item 5003 – Level A consultation in the after-hours (eg away from consulting rooms, RACF) – were small (1704 in 2010–11 and 6052 in 2015–16), there was a 255% increase over the reporting period. For MBS item 5023 – Level B consultations in the after-hours (<20 mins) – an increase of 125% was observed between 2010–11 and 2015–16 (145,900 and 328,726 respectively). Claims for MBS item 5043 – Level C consultation after-hours (+20 minutes) – increased by 66% (23,817 in 2010–11 to 39,656 in 2015–16). For MBS item 5063 – Level D consultations (+40 minutes) – the number of claims increased by 101%, from 4045 in 2010–11 to 8137 in 2015–16.
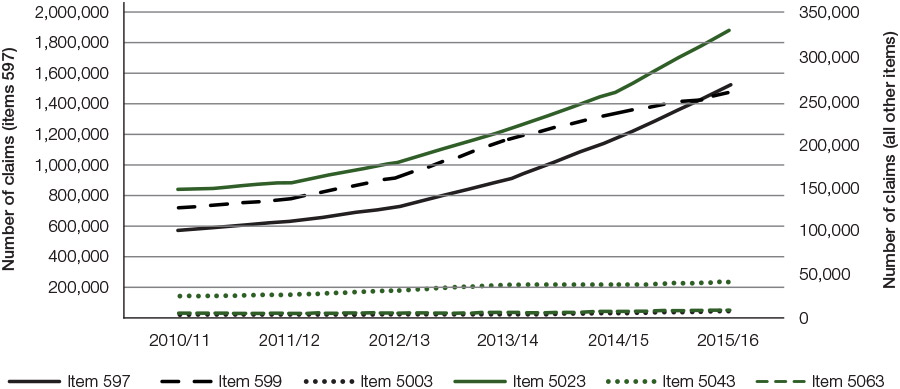
Figure 1. National claims for MBS items 597, 599, 5003, 5023, 5043, 5063 from 2010–11 to 2015–16
Source: Medicare item reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp
Figure 2 illustrates the claims for MBS item number 597 per 100,000 persons per financial year nationally and by jurisdiction. Nationally, the rate of claims per 100,000 persons per financial year increased steadily from 2518 in 2010–11 to 3120 in 2012–13 (24% growth). Over the subsequent three financial years, claims increased to 6221 per 100,000 persons per financial year, representing a 99% increase since 2012–13.
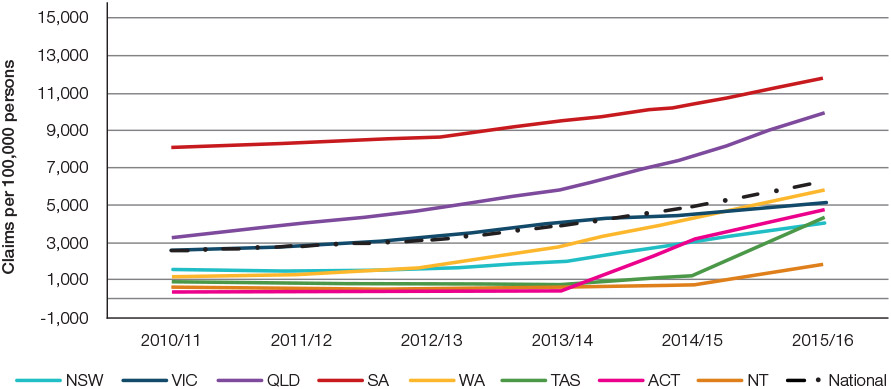
Figure 2. State and territory claims for MBS item 597 per 100,000 persons
Source: Medicare item reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp
South Australia consistently had the highest rate of claims for MBS item number 597 per 100,000 persons per financial year. In 1996–97, when per capita reporting of this MBS item number first became available, the South Australian rate was 2562 per 100,000 persons, markedly higher than all other jurisdictions. It was 246% greater than the national average rate of 740 claims per 100,000 persons (data not shown). In 2010–11, there were 8032 claims per 100,000 persons in South Australia, 219% of the national rate. Claims in South Australia increased by 46% over the subsequent five financial years to 11,750 claims per 100,000 persons in 2015–16.
For the Australian Capital Territory, Tasmania and the Northern Territory, it was possible to identify dates for the establishment of AHMDSs. For the Australian Capital Territory, this occurred in August 2014,3 in February and June 2015 for Tasmania,4,5 and late November 2015 for the Northern Territory.6
For the Australian Capital Territory, the rate of claims increased from 345 per 100,000 persons per financial year or less until 2013–14, to 3162 per 100,000 persons in 2014–15. In 2015–16, the rate of claims continued to increase, with 4728 per 100,000 persons. Since 2013–14, an increase of 1270% was observed for the rate of MBS item 597 claims.
In Tasmania, two AHMDS were established in the first half of 2015. Up until 2013–14, the rate of claims for MBS item 597 was 735–848 per 100,000 persons per financial year. In 2014–15, which included less than five months of AHMDS providing services, the rate of claims increased to 1256, and in 2015–16, to 4302 claims per 100,000 persons per financial year. This represents a 485% increase between 2013–14 and 2015–16.
In the Northern Territory, the rate of claims was 442–710 per 100,000 persons per financial year up to 2014–15. In 2015−16, the rate of claims increased to 1772, representing a 150% increase since 2014–15. The 2015–16 reporting period includes the first seven months of the AHMDSs commencing operations in Darwin.
As AHMDSs were introduced in multiple locations over a rolling period in other jurisdictions, the impact of the introduction of AHMDS in these locations could not be definitively established. However, clear trends of increasing claims were observed. For Western Australia, over the 2010–11 to 2015–16 period, a 407% increase was observed for MBS item number 597 claims (1145 claims per 100,000 persons in 2010–11 to 5800 claims per 100,000 persons in 2015–16). For Queensland, a 208% increase was observed (3239 claims per 100,000 persons in 2010–11 to 9989 claims per 100,000 persons in 2015–16). For New South Wales, an increase of 162% was observed (increasing from 1536 claims per 100,000 persons in 2010–11 to 4728 claims per 100,000 persons in 2015–16).
Table 1. GP after-hours MBS items15 and definitions of after-hours periods7
|
Item number
|
Item description
|
2016 fee
|
|---|
|
Urgent items
|
|
|
|
597
|
Urgent attendance after-hours
(sociable hours)
|
$129.80
|
|
599
|
Urgent attendance after-hours
(unsociable hours)
|
$153.00
|
|
Non-urgent items
|
|
|
|
5003
|
Level A consultation after-hours
(away from consulting rooms, RACF)
|
$54.95
|
|
5023
|
Level B consultation after-hours (<20 mins)
|
$74.95
|
|
5043
|
Level C consultation after-hours (+20 mins)
|
$109.90
|
|
5063
|
Level D consultation after-hours (+40 mins)
|
$143.70
|
|
After-hours
|
|
|
|
Weekdays
|
6.00 pm to 8.00 am
|
|
|
Saturdays
|
Noon onwards
|
|
|
Sundays and public holidays
|
All day
|
|
|
Unsociable hours (7 days per week)
|
11.00 pm to 7.00 am
|
|
|
RACF, residential aged care facility
|
Tasmanian MBS and emergency department data
Figure 3 shows Tasmanian-specific data for the number of MBS item number 597 claims and presentations to Tasmanian public hospital emergency departments. Between 2010–11 and 2015–16, an increase in all public hospital emergency department presentations of 7% was observed (143,848 in 2010–11 to 153,692 in 2015–16). The number of low-acuity presentations increased marginally from 84,396 in 2010−11 to 84,985 in 2015–16 (0.7%; Figure 3).
For Tasmania, the number of claims for MBS item number 597 was 3856–4377, between 2010–11 and 2013–14. The 2014–15 period covers the establishment of the two Tasmania-based AHMDSs (February and June 2015). In 2014–15, the number of claims increased to 6634, and subsequently to 22,841 in 2015–16. This represents a 492% increase in the number of claims for MBS item number 597 since 2013–14 (Figure 3).
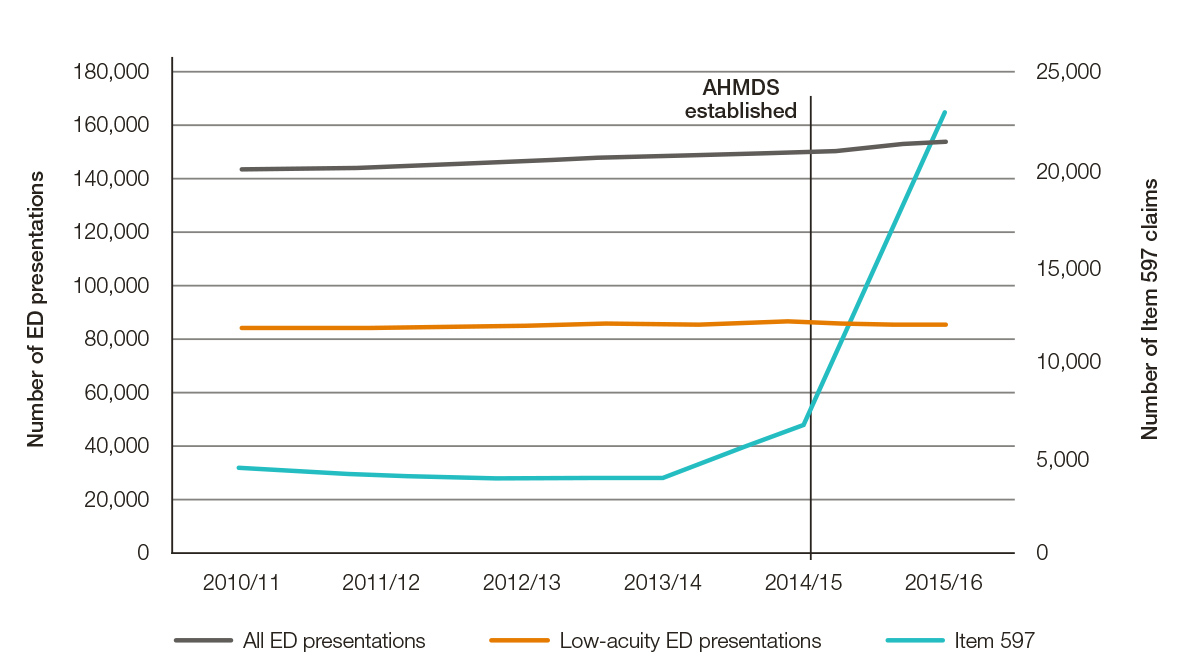
Figure 3. Tasmanian public hospital ED presentations (all and low acuity) and claims for MBS item 597 by financial year from 2010–11 to 2015–169,16
Source: Medicare item reports http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp;
Tasmanian ED separation data obtained from Department of Health and Human Services (Tasmania). Low acuity refers to triage categories 4 and 5.
Discussion
This analysis provides confirmation that substantial increases in the number of claims for all after-hours MBS item numbers between 2010–11 and 2015–16, particularly for MBS item number 597, has occurred. Growth in non-urgent claim items (ie 5003, 5023, 5043, 5063) was also observed, although not as extensive (relatively or absolutely) and off a much lower base than for MBS item number 597. Growth occurred at both national and jurisdictional levels. With reference to claims data for the Australian Capital Territory, Tasmania and the Northern Territory, clear evidence emerges that the commencement of AHMDSs in these jurisdictions are, to a large extent, responsible for this growth in these regions. By contrast, Tasmanian emergency department data show no commensurate decrease in total or low‑acuity presentations.
AHMDSs became formalised as service providers in 1999 following the establishment of the Approved Medical Deputising Services Programme by the Department of Health in the same year. According to guidelines made pursuant to section 3GA of the Health Insurance Act 1973,7 an AHMDS is defined as:
an organisation that arranges for, or facilitates the provision of, medical services to patients of general practitioners (Principals) by other medical practitioners (deputising doctors) during the absence of, and at the request of, the Principals.
AHMDSs were envisaged as a support mechanism for general practices in the after-hours period, arising out of recognition that there was a workforce shortage for providing after-hours medical care to the community.7 The use of AHMDSs was also indirectly supported through the Department of Health’s Practice Incentives Program: After Hours Incentives.12 The data presented in this paper suggest that AHMDSs may not be operating these services as intended (ie supporting general practice).
According to the Health Insurance Act 1973,7 an AHMDS is required to enter into a formal deputising arrangement with a general practice. It is therefore possible for an AHMDS to have only a small number of formal arrangements with general practice, with the great majority of patients accessing the service via self-referral. No data are publicly available regarding patient pathways to AHMDSs and the proportion of patients accessing services under formal agreements.
Many AHMDSs advertise bulk-billed, after-hours medical consultations at home. However, the guidelines pertaining to AHMDSs prohibit advertising to promote ‘routine’ or ‘convenience’ type medical care, given they do not offer comprehensive GP care.7 Specifically, section 3GA of the Health Insurance Act 1973, states:
As Medical Deputising Services do not offer comprehensive GP care, direct advertising to encourage patients to use Medical Deputising Services for ‘routine’ or convenience purposes, thereby compromising their access to the full range of GP services, is prohibited.
As bulk-billed, in-home services provided after-hours may certainly be viewed as convenient, it can be argued that AHMDSs are marketing themselves directly to the community using multi-platform advertising approaches. Whether AHMDSs are working within this section of the guidelines is unclear. Review by an administrative law expert is required to answer this question.
Further, it is important to consider the effect AHMDSs are having on the primary healthcare ‘market’. Irrespective of which after-hours MBS item number is being claimed,13 patients now have a choice between services: the convenience of in-home, bulk-billed medical consultations outside of office hours or, alternatively, an appointment at a general practice during office hours, which may incur out-of-pocket costs.
Given that after-hours general practice clinics are operating in urban areas – areas that should have the critical mass to sustain them – it is questionable why such services are not being preferentially supported in the after-hours period. Funding models that target support of after-hour clinics can assist with the financial sustainability of these services, while providing comprehensive patient care.14
There are key issues requiring urgent attention that relate to the large increases reported for after-hours MBS claims and the growth of AHMDS businesses. First, how are patient outcomes affected by increased use of these services? Important aspects of such an evaluation relate to continuity of care, including timely provision of clinical summaries to the patient’s regular GP by the AHMDS. A second key issue relates to the equitable distribution of resources. As AHMDSs have only been established in metropolitan and large regional settings (Appendix 1; available online only), rural and remote communities are unlikely to be receiving the same level of access to urgent after-hours care. If the growth in claims for MBS item number 597 has been largely driven by AHMDSs, as the data suggest, then this use of resources is not being equitably distributed. Health equity is a cornerstone of the Medicare system; therefore, careful consideration of services that do not support this objective is required.
Conclusion
This is the first study to assess national and jurisdictional growth in claims for MBS item number 597 in the context of the recent expansion of AHMDSs. Substantial growth in claims was identified. Establishment dates of AHMDS were established for three jurisdictions. Comparison of claims for MBS item number 597 pre-establishment and post-establishment found growth ranging between 150% and 1270% in 12 to 24 months. The assumption that increased provision of urgent, after-hours consultations would reduce demand for emergency departments was not observed for the Tasmanian case study.
Authors
Barbara de Graaff PhD, Postdoctoral Fellow, Menzies Institute for Medical Research, University of Tasmania. barbara.degraaff@uts.edu.au
Mark Nelson PhD, Chair, General Practice; and Head, Discipline of General Practice School of Medicine, University of Tasmania
Amanda Neil PhD, Select Foundation Senior Research Fellow, Menzies Institute for Medical Research, University of Tasmania
Competing interest and funding: None.
Provenance and peer review: Not commissioned, externally peer reviewed.