Case
A woman, 88 years of age, presented with a three-month history of left-hand weakness. The weakness was of gradual onset, with no history of preceding injury. There was no associated pain, but there was occasional paraesthesia on the lateral side of her thumb. She was unable to actively extend her fingers and thumb, although flexion was unaffected. She also noted a longstanding mass on the anterolateral aspect of the affected forearm.
On examination, the mass measured 30 x 50 mm, was non-tender, non-mobile and not tethered to skin. Neurological examination revealed wasting of the anterior forearm on the affected side, with weakness in finger extension 0/5, thumb abduction 0/5, and wrist extension 3/5. No other neurological deficit was detected.
Question 1
What are the differential diagnoses for unilateral hand weakness?
Question 2
What is the likely diagnosis in this case?
Answer 1
Differential diagnoses for unilateral hand weakness include:
- central nervous system causes (eg cerebrovascular accident, multiple sclerosis, brain tumour)
- cervical pathology (eg cervical stenosis, radiculopathy)
- peripheral nerve lesion (eg trauma, compression, tumour, malignancy)
- systemic disease (eg diabetes, autoimmune diseases, infections)
- iatrogenic causes (eg radiotherapy, chemotherapy, drugs).
Answer 2
The pattern of hand weakness in this patient is consistent with a posterior interosseous nerve (PIN) lesion. The PIN supplies muscles in the extensor compartment of the forearm,1 and is involved in wrist extension (eg extensor carpi radialis brevis, extensor carpi ulnaris), finger extension (eg extensor digiti minimi, extensor digitorum, extensor indicis), and thumb extension and adduction (eg extensor pollicis longus, extensor pollicis brevis, abductor pollicis longus), all of which were affected in this case.
Other common peripheral nerve lesions were excluded as they did not match the presentation of the patient. Carpal tunnel syndrome typically presents with pain and paraesthesia in the first three digits and half of the fourth digit.1 An ulnar nerve lesion presents with paraesthesia of the fourth and fifth digits, with weakness of interosseous muscles in severe cases, affecting grip strength.1
Cervical pathology was unlikely as it is usually associated with neck or arm pain.2 A central cause was deemed unlikely given there were no other neurological symptoms.
Case continued
The patient was sent for further investigation by nerve conduction studies and ultrasonography. Nerve conduction studies confirmed a PIN lesion at the level of the radial head. Ultrasonography revealed the forearm mass to be consistent with a lipoma. The patient was referred to a neurosurgeon, who ordered magnetic resonance imaging (MRI). The MRI confirmed the mass to be a lipoma, measuring 29 x 29 x 55 mm. The lipoma appeared to arise from the supinator, displacing brachioradialis, and associated with the neurovascular bundle (Figure 1). This was the likely cause of the patient’s symptoms, with mass effect of the lipoma causing compression of the PIN against underlying bone.
|
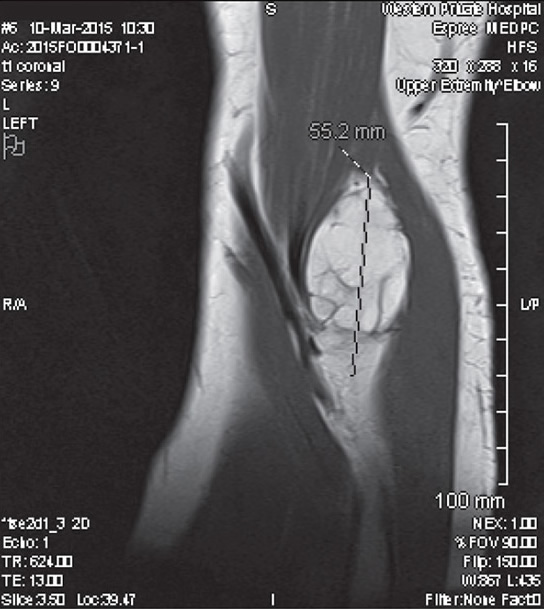
Figure 1. MRI of forearm showing lipoma (29 x 29 x 55 mm)
|
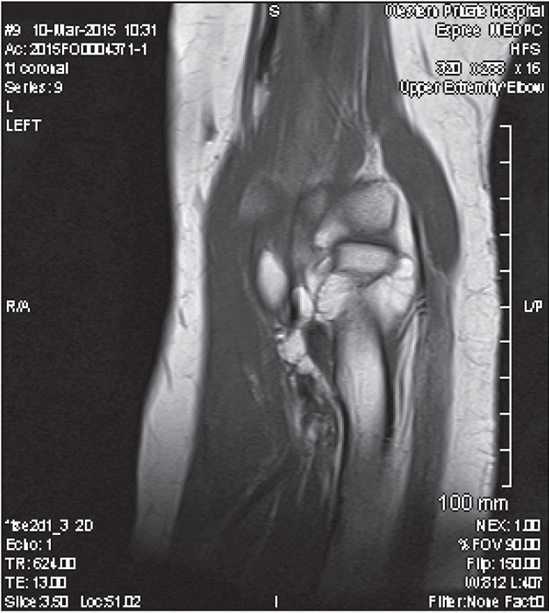
Figure 2. MRI demonstrating lipoma wrapping around the radial head
|
Question 3
How are such lipomas treated?
Question 4
"What would alert you to suspect a PIN palsy? How often is it caused by a lipoma?
Answer 3
Treatment of a PIN palsy caused by a lipoma is through surgical decompression. Intervention within five years can result in near-complete to complete recovery, although further delay in treatment may limit recovery of the affected muscles.3 As such, it is important to identify a lipoma as a potential cause of PIN palsy to ensure timely treatment.
Answer 4
Patients presenting with a PIN palsy caused by lipoma will typically describe weakness of digital extension of insidious onset. Some patients may also experience significant pain radiating from the forearm into the neck and back, and a sense of heaviness in the involved arm.4
Lipomas of the proximal forearm are a rare cause of PIN palsy, with less than 40 cases described in the English literature.5 Lipomas are typically found in subcutaneous tissue; however, in deeper sites, these may be a cause of symptoms arising from compression of nerves against underlying bone.4,6 As such, examination is vital in such presentations as a forearm mass can be easy to overlook.
Case continued
The patient was reluctant to undergo surgical intervention given her symptoms were not limiting her function. Surgery was deferred and the patient was monitored. Ten months later, the mass had become firmer and larger. Given this progression and concerns of potential malignancy, the mass was excised. Histology confirmed the lesion was indeed a lipoma, with no evidence of malignancy. On review, one week postoperatively, the patient reported improved strength and dexterity, and no further paraesthesia. Wrist extension remained at 3/5, although finger extension and thumb abduction improved to 3/5.
Key points
- The differential diagnosis for hand weakness can include a reversible peripheral nerve palsy, even in the setting of severe muscle weakness.
- Lipomas, although benign, can cause peripheral nerve palsy by compression against bone, as in the case of the PIN.
- Identification of a lipoma as the cause of hand weakness can allow timely treatment and prevent permanent disability.
Authors
Mark Huang MD, Intern, Western Health, Vic
Helen Dooley MBBS, Principal, The Clinic Footscray; Life Member RACGP; and Supervisor Liaison Officer MCCC, Vic. dooleyh@clinicfootscray.com.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.