Constipation is a common problem in childhood, affecting an estimated 3% of children worldwide and up to 30% in some settings.1–3 There is a degree of variability in the expected frequency of stools in healthy children; however, most children pass stools every two to three days, whereas breastfed babies may only pass stool once a week. Constipation is defined as the infrequent passage of stools (≤2 per week) with associated stool retention, and possible painful bowel actions or overflow faecal incontinence and soiling (encopresis). ‘Functional constipation’ describes constipation that does not have an organic aetiology.4
Constipation in children is usually functional or idiopathic, and related to behavioural withholding after a painful or unpleasant stool event. Stool builds up within the colon and rectum, leading to the absorption of water and, therefore, accumulation of hard faecal matter.5 This faecal retention stretches the lower bowel and rectum. Over time, the sensation of ‘needing to go’ when the rectum is full diminishes with persistent rectal stretching from chronic stool loading. This rectal hyposensitivity can lead to involuntary soiling and will persist until chronic stretching is alleviated and prevented from recurring. Soiling can be embarrassing and distressing.
Treatment needs to first disimpact hard stool from the bowel, then maintain ongoing soft stools. A supportive and long-term outlook to treatment over months is required. Successful management of childhood functional constipation in primary care will have a significant positive impact for children and families, and be very rewarding for clinicians.
History
Key features to ask about are the stool frequency and consistency using the Bristol stool form scale (Figure 1),6 precipitating factors (eg painful stool events, behavioural toileting refusal), faecal soiling, and the presence of any red flags that suggest serious organic pathology (Table 1). Childhood functional constipation is best described using the Rome IV criteria and is defined by the presence of two or more of the following features for at least one month:5,7–9
- ≤2 stools per week
- excessive stool retention
- painful or hard bowel movements
- presence of large faecal mass in rectum
- history of large diameter bulky stools
- >1 episode per week of faecal incontinence after toilet training completed.
While the median age for onset of functional constipation is 2.3 years,5 common times for constipation to arise include transition to solids, toilet training and school entry. Other precipitants to investigate include painful bowel actions leading to withholding behaviour (eg perianal skin conditions, anal fissures), toileting refusal, change of diet and psychosocial stressors.
The Bristol stool form scale (Figure 1) allows a reproducible, subjective assessment of stool consistency,6 and the chart is freely available online from the Royal Children’s Hospital’s Constipation clinical practice guideline.10 A Bristol type 3 or 4 stool every day or every second day is the goal. When constipated, there may be hard stools (types 1–2); if there is retained impacted stool, there may be watery overflow diarrhoea (types 6–7).
Dietary factors, including inadequate fibre and water intake, are rarely the primary cause of constipation but may contribute. Ask about other medications (eg anticholinergics), previous laxative use, and their duration and effect.
Organic disorders are uncommon, but consider the possibility of coeliac disease or cow’s milk protein allergy if the history is suggestive. The presence of red flag symptoms (Table 1), such as urinary incontinence in a previously continent child, should prompt specialist referral.
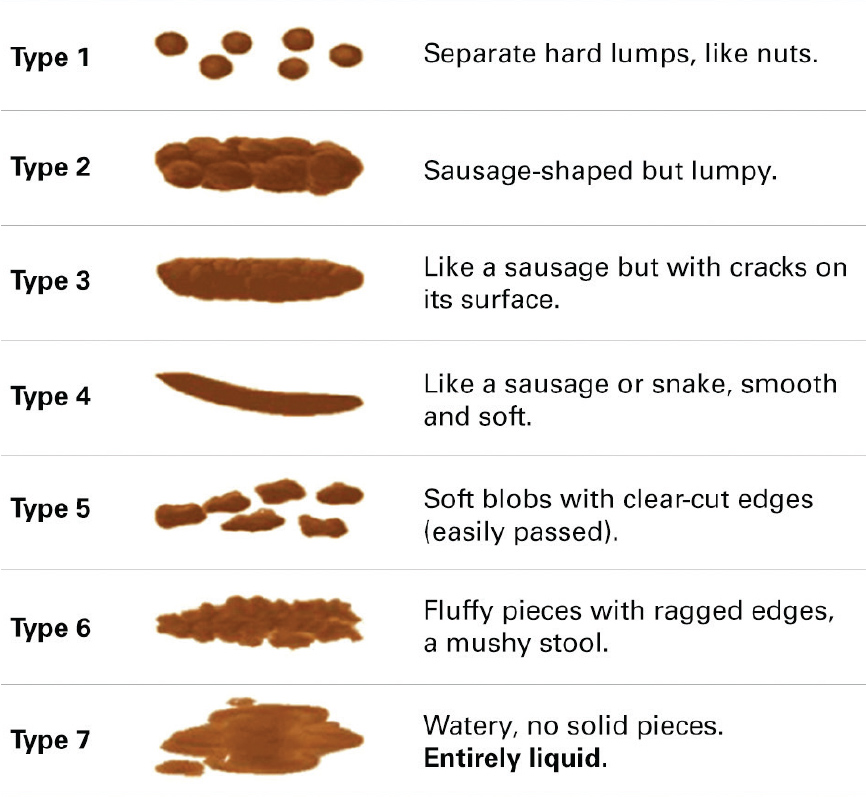
Figure 1. Bristol stool form scale6
Table 1. Childhood constipation key history and red flags
|
Constipation history key areas
|
|---|
|
Stool frequency: <2 per week
|
|
Stool consistency (using Bristol stool chart, normal is types 3–4)
|
|
Painful bowel actions, straining, withholding behaviour
|
|
Passing large, bulky stools
|
|
Faecal incontinence and soiling
|
|
Other precipitants: toileting refusal, psychosocial stressors, school entry
|
|
Diet: introduction of solids, adequate fibre and water intake
|
|
Other medications such as anticholinergics
|
|
General growth and developmental progress
|
|
Previous treatments: duration and effect/success
|
|
Red flags for other disorders
|
|---|
|
Failure to pass meconium <48 hrs after birth
|
Hirschprung’s disease
|
|
Onset of constipation (from birth or first weeks of life)
|
Congenital, mechanical obstruction
|
|
Stool consistency (ribbon/pencil-thin stools)
|
Anorectal malformation
|
|
Bloody diarrhoea
|
Infection, inflammatory bowel disease, cow’s milk protein allergy
|
|
Developmental delay
|
Metabolic or other
|
|
Lower limb neurology or urinary incontinence in older child
|
Spinal pathology
|
|
Other physical signs: lethargy, fever, bilious vomiting, rash
|
Infection, obstruction, metabolic
|
Examination
A general examination should include recording the current growth parameters and centiles (ie height, weight, head circumference), compared with previous records, to check for faltering growth trajectory and failure to thrive. A targeted abdominal examination should check for distension, bowel sounds and palpable stool. The spine and sacrum (to exclude hair patches, sacral pits, scoliosis), and lower limbs (muscle bulk, tone, power, reflexes of the lower limbs or functional testing in younger children) should be examined for features that suggest possible neurological aetiology. The perianal area should be examined for the anal orifice position, fissures and skin tags. Digital rectal examination is not routinely indicated in children, as the history and abdominal examination is sufficient for evaluation of retained stool:2 refer for specialist assessment if there are specific concerns.
Investigations
Investigations are not necessary if the history is consistent with functional childhood constipation. Full blood count and testing for coeliac disease, hypercalcaemia or hypothyroidism should be considered in cases of intractable constipation. Abdominal X-ray is not routinely indicated2,3 and does not assist with the diagnosis of idiopathic or functional constipation. The history and physical examination of the abdomen provides sufficient clinical information regarding the presence of retained stool. Repeat X-rays are not required.
Treatment
Toileting behaviours and education
Education of appropriate toileting behaviour is essential for long‑term success in the management of constipation. This should be seen as the main treatment, with the role of laxatives being to facilitate easy passage of stools. Reassurance may be required to alleviate parental anxiety. Resources for families and clinicians include the Royal Children’s Hospital’s Constipation clinical practice guideline and Kids Health Info Fact Sheets.
Children should be encouraged to sit on the toilet for five minutes after meals, up to three times per day. Parents should be advised about making toilet sitting a positive activity, with encouragement and support for the child.11 Consider using a star chart to record progress (ie regular sitting, bowel actions, accidents, medications), which can be reviewed at follow-up appointments. Toilet sitting should be praised, even when no stool is produced. Children should sit with their feet supported and with their knees just above their hips – use a small stool or books to achieve this position. The child should straighten their back and bulge out their abdomen. For school-aged children, it may help to arrange for the child go to the toilet in the last period before lunchtime, or after eating, before playtime commences. A brief note or phone call to the child’s teacher may assist in establishing this routine, and gather further information from the school environment that may be helpful.
Disimpaction
Disimpaction is often the first step needed to achieve treatment success, to remove the build-up of stool. This should be instigated where there is a history suggestive of chronic constipation and overflow soiling, with faecal loading on examination.12 During disimpaction, families should be advised about what to expect, including elimination of the impacted faecaloma and a period of loose stools. PEG (polyethylene glycol) 3350 with or without electrolytes should be used for disimpaction (Table 2).2,12–16 It is often helpful to keep school-aged children home from school for a few days (usually during second to fourth day of treatment) to achieve adherence and minimise the distress of increased soiling, or plan the disimpaction during school holidays. Aim for a watery, clear stool, which often takes up to a week of treatment to achieve. Parents may stop the disimpaction too early as the loose stools can be challenging to manage, so it is important to prepare them for the short-term inconvenience required for successful treatment.
Table 2. Childhood constipation disimpaction: First-line oral outpatient recommended regimen20
|
|
PEG 3350 + electrolytes (paediatric/junior strength sachets) or PEG 3350 without electrolytes (small scoop)
|
|---|
|
Age
|
Day 1
|
Day 2
|
Day 3
|
Day 4
|
Day 5
|
Day 6
|
Day 7
|
|
1–12 months
|
1/2–1
|
1/2–1
|
1/2–1
|
1/2–1
|
1/2–1
|
1/2–1
|
1/2–1
|
|
1–6 years
|
2
|
4
|
4
|
6
|
6
|
8
|
8
|
|
6–12 years
|
4
|
6
|
8
|
10
|
12
|
12
|
12
|
|
|
PEG 3350 + electrolytes (adult strength sachets) or PEG 3350 without electrolytes (large scoop)
|
|---|
|
12–18 years
|
8
|
8
|
8
|
–
|
–
|
–
|
–
|
|
PEG, polyethylene glycol
|
Maintenance treatment
After disimpaction has been achieved (if required), maintenance therapy should be initiated (Table 3). Treatment effectiveness is defined by soft, spontaneous bowel actions most days of the week (Bristol types 3–4). There should be no faecal soiling or sense of urgency. Families should be advised to continue regular laxatives for at least two months, as premature treatment cessation often leads to recurrence within a few weeks. Titrate the dose to treatment effectiveness rather than ceasing too early. Educate families about the purpose of this extended duration of treatment, which is for the bowel to ‘re-learn’ signals from the brain as to when the rectum is full. When the rectum has been chronically full, the signals have been switched off, and a period of regular soft stools are required for this re-learning. Use of simple language and a diagram may be helpful. Families are often concerned that the continuation of laxatives will lead to diarrhoea or dependence. It is important to reassure families that this should not occur if they use the appropriate dose and frequency.
Table 3. Childhood constipation maintenance treatment guidelines10
|
Generic name
|
Mechanism of action
|
Maintenance dose
|
Disimpaction dose
|
Practice points
|
|---|
|
PEG 3350 or
Macrogol 3350
|
- Iso-osmotic
- Brings water into stool
|
- Aged 1–4 years –
1/2 scoop daily
- Aged 4–5 years –
1 scoop daily
- Aged 6–12 years –
1.5 scoops daily
- Aged >12 years –
2 scoops daily
|
Refer to Table 2
|
- Can be added to any warm or cold drink
- 1/2 scoop (8.5 g)
- 1 scoop (17 g)
- Virtually tasteless
- Safe for long-term use
- PBS-listed
|
|
PEG 3350 plus electrolytes or
Macrogol 3350 plus electrolytes
|
- Iso-osmotic
- Brings water into stool
|
- Aged 2–5 years – 1 half strength sachet daily
- Aged 6–12 years –
1 sachet daily
- Aged >12 years –
1–3 sachets daily
|
Refer to Table 2
|
- Full strength (13 g)
- Half strength (6.9 g)
- Salty taste
- Safe for long-term use
- PBS-listed
|
|
Paraffin oil
|
|
- Aged 1–6 years –
10–15 ml daily
- Aged 6–12 years –
15–20 ml daily
- Aged >12 years – up to 40 ml daily
|
NA
|
- Contraindicated in those with aspiration risk
- Can stain underpants orange colour from oil
|
|
Lactulose
|
- Osmotic laxative
- Brings water into stool
|
- Aged 6 months–1 year –
5 ml daily
- Aged 1–6 years –
5–10 ml daily
- Aged >7 years –
10–15 ml daily
|
NA
|
- Can cause bloating/abdominal discomfort
|
|
Coloxyl drops
|
- Poloxamer
- Assists mixture of water into stool
|
- Aged <6 months –
0.3 ml TDS
- Aged 6–18 months –
0.5 ml TDS
- Aged 18 months–3 years
– 0.8 ml TDS
|
NA
|
- Coloxyl + senna should be avoided unless stools are soft as senna is a stimulant
|
|
Sodium picosulfate drops
|
- Stimulant
- Increases peristalsis in the gut
|
- Aged 4–10 years –
5–10 drops nocte
- Aged >10 years –
10 drops nocte
|
NA
|
- Causes cramping if impacted
- Drops are helpful if unable to swallow large volumes
|
|
Bisacodyl tablets
|
- Stimulant
- Increases peristalsis in the gut
|
- Aged >10 years –
1–2 tablets (5 mg) nocte
|
NA
|
- Causes cramping if impacted
|
|
Sodium citrate/sodium lauryl sulfoacetate/
glycerol enemas
|
- Osmotic laxative
- Glycerol acts as lubricant
|
NA
|
NA
|
- Avoid when possible
- 5 mL per rectum
- Consider sedation with use
|
|
NA, not applicable; PBS, Pharmaceutical Benefits Scheme; PEG, polyethylene glycol
|
Diet and food intolerance
Families often ask whether increased fibre or a change in diet will improve their child’s constipation. While an increase in dietary fibre and adequate water intake may assist in improving stool consistency, this alone will be insufficient to resolve the condition.17 It is uncommon for specific foods (eg dairy, wheat) to be contributing, but reassessment during treatment failure should be an opportunity to consider coeliac disease,18 cow’s milk protein allergy19 or food intolerance.
Refractory constipation
If there are ongoing symptoms of constipation after six months of appropriate treatment, a referral for specialist care and a second opinion is warranted. Specifying chronicity and previous treatment measures in the referral letter can assist with prioritising referrals. Continue to monitor treatment while waiting for review, and aim to support families with long-term treatment as ongoing care may be required.
Authors
Michelle Waterham BSc, MBBS (Hons), Department of General Medicine, Royal Children’s Hospital, Melbourne, Vic
Jonathan Kaufman MBBS (Hons), Department of General Medicine, Royal Children’s Hospital, Melbourne, Vic; Department of Paediatrics, University of Melbourne, Vic
Susan Gibb MBBS, FRACP, Department of General Medicine, Royal Children’s Hospital, Melbourne, Vic; Department of Paediatrics, University of Melbourne, Vic. susan.gibb@rch.org.au
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We would like to thank Ms Misel Trajenovska from Regaining control: Bowel and Bladder Dysfunction at the Royal Children’s Hospital for her background information and contribution.