Case
An Indian man, aged 33 years, presented to his general practitioner (GP) with fever, dyspnoea, intermittent, sharp, non-radiating retrosternal chest pain, nausea and night sweats. His skin, joint, lymphatic, cardiorespiratory and gastrointestinal examinations were non‑contributory. Other issues included:
- mild ulcerative colitis that was managed with maintenance sulfasalazine, and four months earlier with prednisone and methotrexate
- hypoechoic complex left testicular cyst (Figure 1) without epididymo-orchitis, which was identified five months earlier with intermittent pain, but was considered of uncertain significance.
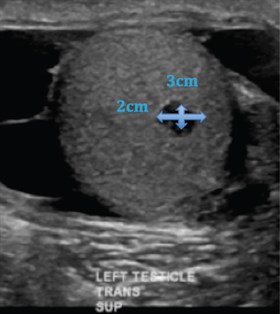
Figure 1. Left testicle on ultrasound
The patient was born in India and migrated to Australia at 17 years of age, with four return trips, most recently two years earlier. He received the BCG vaccination and had no known tuberculosis (TB) contacts. He lived with his wife, had no children or pets, and was a non-smoker and abstainer of alcohol.
He was regularly reviewed over a four-week period, during which he completed a course of amoxicillin and roxithromycin. He remained febrile (39.5°C) and his inflammatory markers were elevated (white cell count: 22.1 x 109/L and C-reactive protein [CRP]: 230 mg/L), normal chest X-ray and negative QuantiFERON-TB Gold (QFT-G) test.
Question 1
What is the most likely diagnosis? What differentials would you consider?
Question 2
What is the role of the QFT-G test in TB diagnosis?
Question 3
What further investigations would you perform?
Answer 1
Reactivated latent TB infection (LTBI) is an important differential diagnosis in an individual from India with persistent fever, who was recently treated with immunosuppressive medications. Individuals with LTBI have a 5–10% lifetime risk of reactivation.1,2 In this case, the risk factors for reactivation include being from a high-risk, endemic area and recent use of corticosteroids to manage his ulcerative colitis.2 Genitourinary involvement occurs in 10% of extrapulmonary TB (EPTB) cases.3 Scrotal TB typically present with epididymo-orchitis and non-simple lesions.4
Infectious, malignant and inflammatory aetiologies must be considered. Human immunodeficiency virus (HIV) with opportunistic infection must be excluded. In a young man, testicular cancer may disseminate through para-aortic and pulmonary lymph nodes. Polyarteritis nodosa may affect the testicles and mesenteric vessels, causing abdominal pain. Inflammatory bowel disease is difficult to differentiate from TB if not actively considered and excluded at the time of presentation.
Answer 2
QFT-G analysis measures the amount of interferon-gamma (IFN-γ) released into whole blood by lymphocytes following stimulation by synthetic Mycobacterium tuberculosis antigens.5,6 It is unaffected by the BCG vaccine.5,6 QFT-G is not a useful test in active TB as it cannot distinguish between latent and active TB. It is also negative in up to half of patients, and has a sensitivity of about 64% and specificity up to 100% in active TB.6,7
Active TB results in a complex immune system response, whereby patients are less likely to produce the detected cytokines. Furthermore, QFT-G appears to have even poorer sensitivity of around 67% in detecting active EPTB.6,7 The gold standard for diagnosis of active TB is culture. False negatives and false positives may result from patient factors such as immune function, disease factors (eg presence of EPTB) and multiple steps in collection or processing.
This patient could have had active EPTB at the time of QFT-G collection, which would explain the negative result.
Answer 3
A computed tomography (CT) scan of the chest, abdomen and pelvis should be performed to examine for pulmonary consolidation, lymphadenopathy and other organ involvement of either TB or testicular cancer. Sputum samples for acid-fast bacilli (AFB) smears and TB culture are positive in one-third of patients with EPTB with no pulmonary involvement.8,9 HIV predisposes for disseminated TB and serology should be performed. Elevated levels of alpha fetoprotein (AFP) and beta-human chorionic gonadotropin (b-hCG) would raise concern for testicular cancer. A vasculitic screen with raised erythrocyte sedimentation rate and positive perinuclear anti-neutrophil cytoplasmic antibodies would suggest microscopic polyangitis. Dysmorphic red cells or casts in urine microscopy may suggest renal vasculitis.
Case continued
The patient was referred to the local hospital as he was febrile and tachycardic (heart rate 130 bpm sinus rhythm) for further investigation.
There was no growth in urine or blood cultures. Induced sputum was smear-negative and mycobacterial culture-negative. CT scans of the chest, abdomen and pelvis showed normal heart and lung fields, enlarged right subcarinal and paratracheal lymph nodes, and multiple nodular lesions in the liver (Figure 2).
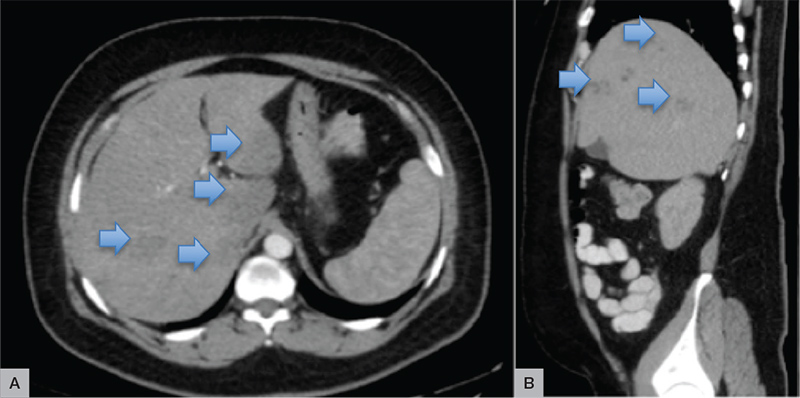
Figure 2. Computed tomography scans of the abdomen (A) and pelvis (B)
Histopathology from a core liver biopsy revealed necrotising granulomatous inflammation, consistent with disseminated TB involving the liver, lymph nodes and testicle. No AFB were seen and there was no growth. While awaiting biopsy results, the patient remained tachycardic and a CT pulmonary angiogram revealed a new significant 3.6 cm pericardial effusion.
The patient was commenced on standard HRZE (isoniazid, rifampicin, pyrazinamide and ethambutol) daily therapy for presumed TB, and oral prednisone 50 mg daily for tuberculous pericarditis. Following this, the pericardial effusion resolved without further intervention, his steroids were rapidly tapered after three weeks, and he continues on HRZE treatment.
Question 4
How common is pericardial TB? Are corticosteroids as adjunctive treatment indicated?
Answer 4
TB pericarditis accounts for the majority of pericarditis cases in developing countries, and is associated with high morbidity and mortality (approximately 25%), even with anti-TB treatment.10 It typically presents as a slowly progressive febrile illness with dyspnoea and variable chest pain, where it is often described as anterior and pleuritic.11 Rarely, it presents acutely with tamponade.3,10 The key investigation is a trans-thoracic echocardiogram; however, CT of the chest can provide valuable information regarding pleural, pericardial and lymph node involvement.11 A recent, large study provides the highest level of evidence for the use of steroids in pericardial tuberculosis.10 The steroid benefit appears greater in patients who are HIV-negative by the reduction in the rate of complicating constrictive pericarditis, with a hazard ratio of 0.56.10
In this case, tuberculous pericarditis probably caused the initial symptoms with a significant pericardial effusion developing over the course of one week following admission of the patient to hospital.
Key points
- Reactivation of latent TB is an important differential to be considered in an individual with a history of travel to, or migration from, a TB-endemic area who presents with persistent fever and constitutional symptoms.
- The QFT-G test can be negative in individuals with active TB, particularly if it is extra-pulmonary.
- Pericardial TB is more common in developing countries and thus individuals who have resided in, or travelled to, TB-endemic areas, especially within the recent two years. Steroids reduce the rate of complicating constrictive pericarditis.
Authors
Cassandra E B Brown MBBS (Hons), DCH, Medical Officer at The Children’s Hospital at Westmead, NSW. cassandra.brown@health.nsw.gov.au
Caitlin Keighley MBBS, BMedSci (Hons), DRANCOG, Medical Officer at Westmead Hospital, Westmead, NSW
Scott Chapman MBBS, FRACP, Staff Specialist, Infectious Diseases and Head of Department, Blacktown-Mt Druitt Hospital, Blacktown, NSW,
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.