The assessment and management of pigmented nail bed lesions can be a significant challenge for clinicians. The difficulty arises from the wide spectrum of differential diagnoses, including potentially life-threatening subungual melanoma. Furthermore, many clinicians are inexperienced in the assessment and management of nail apparatus pathology. Figure 1 shows the anatomy of the nail apparatus and location of the germinal matrix, an important site for the development of nail bed pathology.
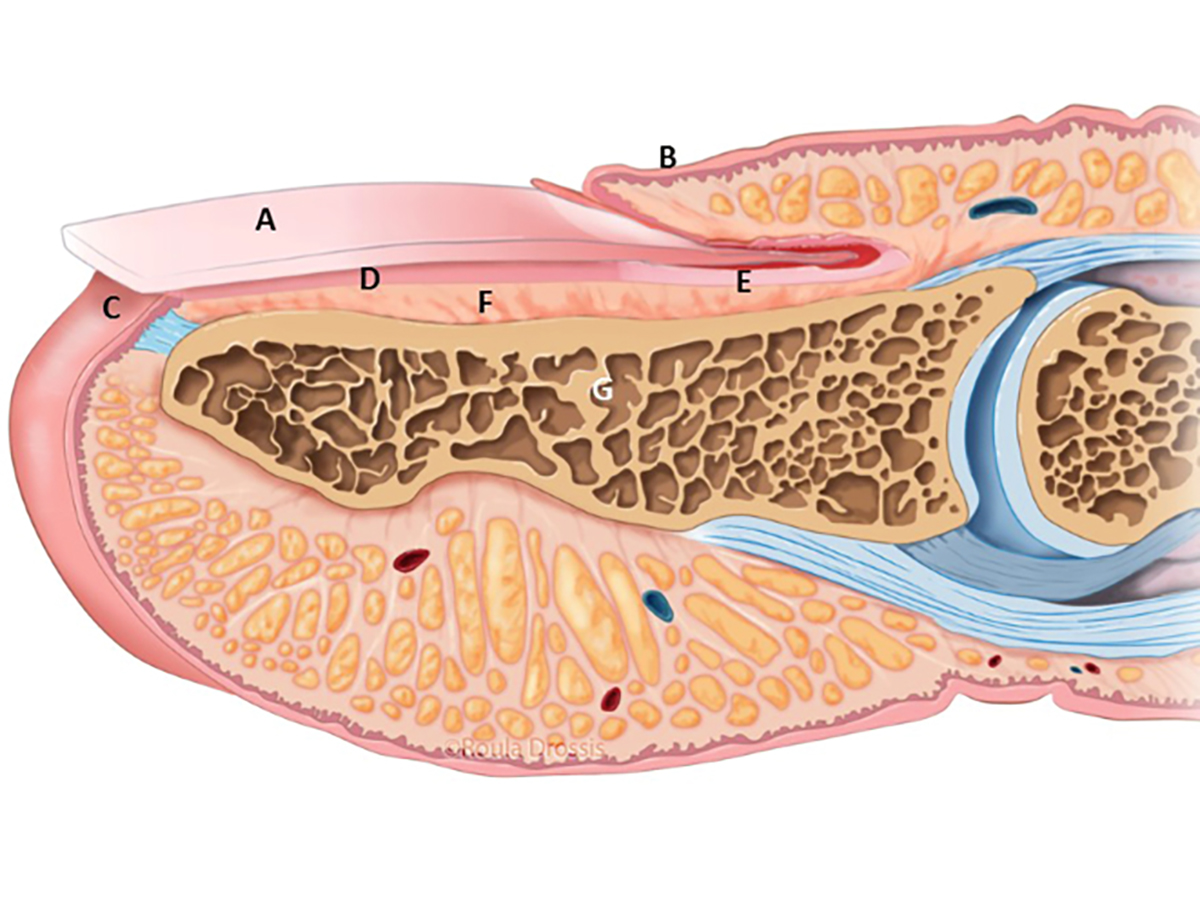
Figure 1. Anatomy of the nail apparatus
A, nail plate; B, proximal nail (eponychial) fold; C, hyponychium; D, nail bed (sterile matrix); E, nail bed (germinal matrix); F, periosteum; G, bone of distal phalanx
Reproduced with permission from Melanoma Institute Australia, copyright Roula Drossis
Subungual melanoma is classified as a subtype of acral lentiginous melanoma, an uncommon form of melanoma that occurs in the glaborous skin of the palms and soles. Acral lentiginous melanoma represents approximately 1–3% of melanoma presentations in the Australian population.1 These tumours are at least equally common in darker skinned individuals and occur most often in the thumb and great toe.2,3
Sun exposure is not related to the development of acral melanomas and, on genomic analysis, they appear to represent a distinct group of tumours. As a group, acral melanomas tend to present late with thicker, more advanced primary tumours. It is postulated that this is related to delays in recognition and diagnosis.2,3 However, matched stage-for-stage, acral melanoma confers the same risk to the patient in terms of recurrence and regional and distant spread, as other cutaneous melanomas.3 Detecting subungual melanoma at an early stage potentially has a great impact on a patient’s likelihood of cure.4
Differential diagnoses
The differential diagnoses for a patient presenting with a subungual lesion are broad. Lesions can be divided into melanocytic and non-melanocytic. They can also be categorised as neoplastic, traumatic, infective, systemic and drug-induced. Figure 2 illustrates the clinical appearance of some common differentials.
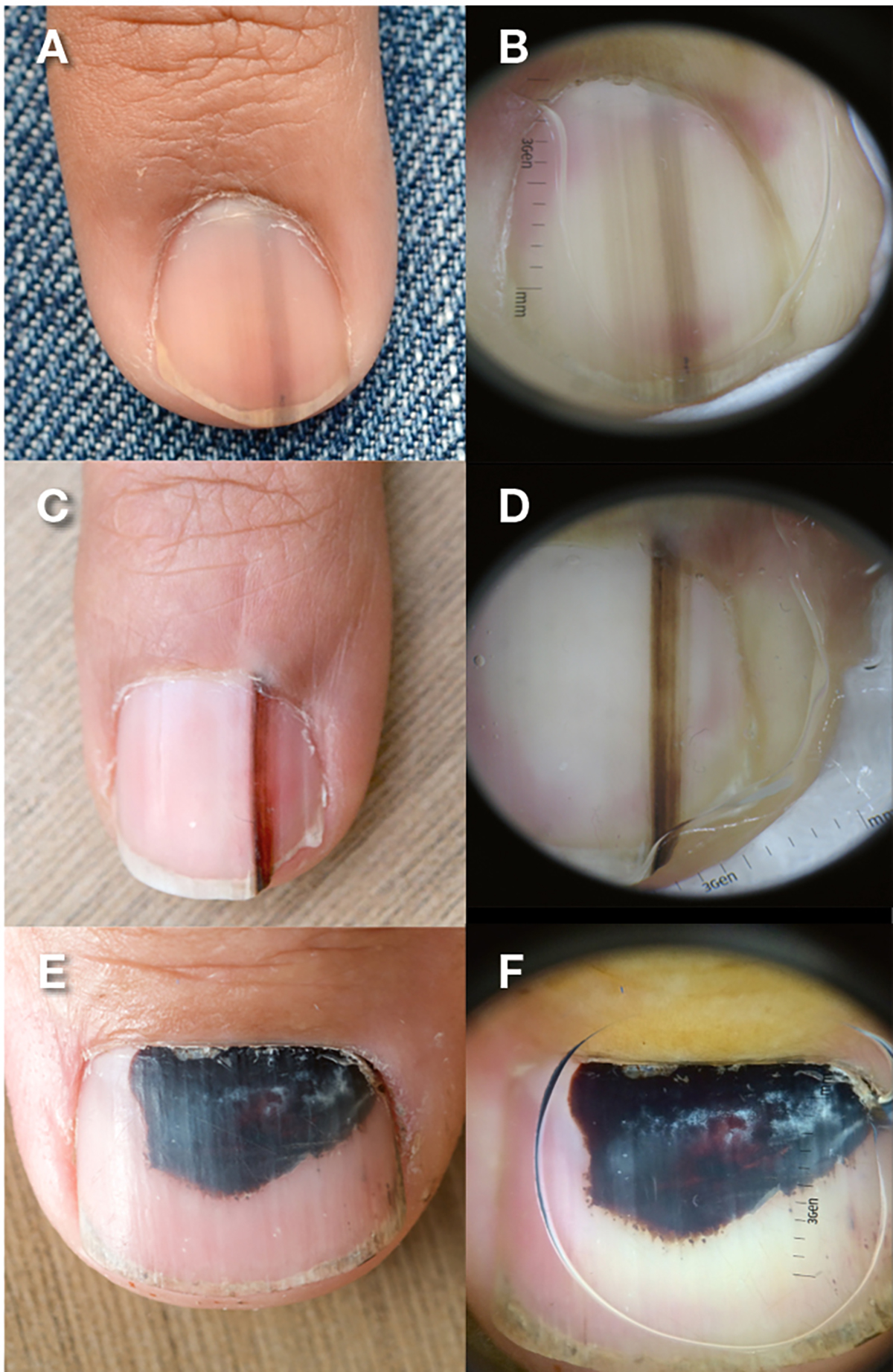
Figure 2. Benign pigmented subungual lesions
A, C, narrow melanonychia with regular borders and parallel bands of pigment; B, D,corresponding dermatoscopic detail of narrow melanonychia with regular borders and parallel bands of pigment; E, F, subungual haematoma with homogenous reddish brown to black colour
Differential diagnoses could include:
- melanocytic lesions
- naevi (moles)
- lentigo (increased single melanocytes)
- melanoma in situ
- melanoma
- subungal squamous cell carcinoma (SCC)
- subungual haemorrhage
- fungal infection
- systemic illness (including systemic lupus erythematosus, scleroderma)
- drug-induced pigmentation
- ethnic-type pigmentation (can often involve multiple digits).
Longitudinal melanonychia is a specific appearance of a linear, pigmented band on the nail plate. This appearance in itself is non-specific and can result from the same variety of diagnoses listed above for any subungual pigmentation. Early subungual melanoma often presents as longitudinal melanonychia.
Assessment
Assessment begins with a thorough history of the lesion. This includes noting the duration, changes over time and preceding trauma. It is important not to exclude a diagnosis of malignancy solely on a history of trauma, as many patients with a subungual melanoma will recall an injury to the digit.5 A general medical history, including medications, and a personal and family history of melanoma are important to elicit.
Clinical examination begins with observation. The size, nature and distribution of nail discolouration should be recorded. Further details of the colour pattern should also be documented, including whether it is homogenous or heterogenous, and if it contains regular or irregular, thick or thin bands of colour. The percentage of the nail bed that is occupied by the lesion should be noted. The presence of a Hutchinson’s sign should alert the clinician to the likelihood of a malignant process and can be seen as pigmentation in the skin of the proximal nail fold. Further signs of invasive disease include nail dystrophy and ulceration. Figure 3 shows a spectrum of clinical appearances of subungual melanoma.

Figure 3. Subungual melanoma, spectrum of clinical presentations
A, large pigmented lesions associated with irregular colours, broad band of pigment, ill-defined edges and nail dystrophy; B, pigmented lesion with involvement of 100% of the nail bed, nail dystrophy, Hutchinson’s sign (pigmentation in the skin of the proximal nail fold) and pigmentation of the surrounding skin distally; C, broad pigmented lesion, irregular colour, ill-defined edges, Hutchinson’s sign and pigmentation in the skin distally; D, amelanotic lesion with destruction of the overlying nail plate and the proximal nail fold; E, F, ulcerated fungating lesion that has replaced the entre nail apparatus, with a satellite lesion located in the pulp skin distally
Dermatoscopy is an important component of the clinical assessment of subungual pigmented lesions. It is a non-invasive technique that uses light, magnification and a liquid medium to allow better evaluation of skin microstructures. While dermatoscopic assessment of pigmented nail lesions can be challenging, practise and experience can improve a clinician’s diagnostic accuracy.4
Dermatoscopy of the nail apparatus requires the use of an interface and is not possible with a polarising light technique. Many interface media are available, but a viscous gel, such as ultrasound gel, will conform to the curved surface of the nail plate.5,6 The classic dermatoscopy appearance of the following lesions is described as follows:2,4–6
- subungual haemorrhage
- pigment appears homogenous
- reddish to brown in colours
- migrates distally on the nail
- benign melanocytic pigmented subungual lesion (naevi and lentigos)
- pigment appears in discrete granules (cellular inclusions)
- bands of pigment have a narrow width (<3 mm)
- distinct edges
- homogenous colour
- parallel bands
- no involvement of the skin of the nail fold
- subungual melanoma
- broad bands of pigment (>3 mm)
- dark brown to black colour
- irregular colours
- fuzzy or blurred lateral borders
- irregular bands that are not parallel, often wider at the proximal end
- presence of pigmentation on the adjacent skin (Hutchinson’s sign)
- nail dystrophy and/or ulceration.
The goal of initial assessment is to form an opinion of the likelihood of the lesion being either benign or malignant. This risk assessment guides whether patients are discharged with reassurance that a lesion is benign, enter a short, defined period of serial monitoring, or undergo a biopsy.
Serial monitoring of a lesion can be a powerful aid in the management of lesions that are indeterminate on initial assessment. The use of dermatoscopy and clinical photography can be particularly helpful and allows for direct comparisons of images obtained over a defined time interval. In cases of subungual haematoma, serial monitoring will often make the diagnosis readily apparent, as the lesion can be observed to migrate distally with normal nail plate growth proximal to the lesion.
We advocate a short, planned period of monitoring. In our practice, the interval between assessments is often 8–12 weeks. However, time intervals should be individualised and based on the likelihood of malignancy and the patient’s circumstances. If a period of clinical monitoring is undertaken, patient recall systems must be used to mitigate the risk of individuals with a potential malignancy being lost to follow up.
Referral to a specialist centre with experience in managing subungual melanoma should be made in cases where the diagnosis remains unclear following a short period of monitoring or in cases where a malignant pathology is suspected from the initial assessment. At the time of referral, the patient will be reassessed and this may result in a clear benign diagnosis, a repeated period of clinical monitoring or a biopsy.
Biopsy
Biopsy of a nail bed lesion is a complex procedure. Improperly planned biopsies can risk obtaining an inadequate specimen or damaging the fragile sample of nail matrix so that histopathological examination is compromised. Furthermore, there is the hazard of causing permanent nail dystrophy from injury to the germinal matrix.2,5 As such, referral to a specialist group with experience in managing subungual pathology is often appropriate in cases where a biopsy is being considered.
An understanding of the nail apparatus anatomy is important when planning a biopsy. Longitudinal melanonychia often results from lesions that occur proximally, as pigment is generated by the lesion within the germinal matrix, then incorporated into the nail plate. The germinal matrix, within the proximal nail fold, is difficult to access (Figure 1). A simple blind punch biopsy of the area may miss the lesion of concern and has the risk of causing a vertical scar through all tissue layers, which will produce a permanent synechiae of the fold.
Where it is clinically warranted, we advocate formal excision biopsy of pigmented lesions. Figure 4 depicts a formal nail bed biopsy occurring under tourniquet control, with loupe magnification, in an appropriate operating room. This technique is performed with direct vision of the lesion, which allows for the highest likelihood of a complete, minimally traumatised pathological specimen for assessment. Wherever possible, we advocate direct repair of the nail bed with fine (7-0 or 8-0), absorbable suture material. This is usually the case with most narrow melanonychia. This approach avoids any overlapping scars within the tissue planes and so should minimise the risk of nail dystrophy. In cases of broad melanonychia, excision of the lesion may produce a defect in the germinal matrix that is unable to be closed primarily. In these instances, additional reconstructive techniques such as partial-thickness or full-thickness nail bed grafts can be used; however, discussion of these procedures is beyond the scope of this article.

Figure 4. Excision biopsy technique
A, longitudinal melonychia; B, nail plate removed showing a normal sterile matrix; C, reflection of proximal nail fold to reveal pigmented lesion within the germinal matrix; D, excision biopsy of lesion (specimen placed on dorsal aspect of finger) defect in germinal matrix can be seen with perosteum visible in base; E, primary repair of nail bed with 8-0 braided resorbable suture; F, repair of proximal nail fold and nail plate replaced as
a dressing and splint (note nail plate with residual pigmented streak will fall out in several weeks)
A number of alternative nail bed biopsy techniques have been discussed in the literature, although many carry a significant risk of causing nail dystrophy when compared with our preferred approach. These alternative techniques include blind punch biopsy through the proximal nail fold, double punch biopsy of distal lesions, nail removal and shave biopsy, and longitudinal en bloc excision.2,5,7,8
Conclusion
Managing patients who present with pigmented subungual lesions can be a source of anxiety for clinicians. However, a systematic approach to assessing and reviewing these patients has the potential to minimise patient morbidity and improve patient outcomes. While some patients will present with obvious signs of advanced subungual melanoma and require immediate referral, the majority will have benign or indeterminate pathology on initial assessment. Accurate clinical assessment and judicious use of short-term clinical monitoring will help to identify patients who will benefit from an expert review. Given the poor outcomes associated with delays in diagnosing subungual melanoma, early detection may have the possibility to appreciably improve disease outcomes for these patients.
Nail bed biopsies are complex procedures and carry the risk of producing an inadequate or damaged specimen that is unsuitable for histological assessment, and of causing permanent nail dystrophy. Where clinically indicated, we advocate that a formal open nail bed biopsy should be performed by an experienced clinician.
Authors
Michael Alexander Rtshiladze MBBS, MS, FRACS (Plast), Poche Fellow, Melanoma Institute Australia, North Sydney, NSW
Jonathan Raymond Stretch MBBS, PHD, FRACS (Plast), Deputy Director, Melanoma Institute Australia, North Sydney, NSW; Associate Professor, Discipline of Surgery, Sydney Medical School, University of Sydney, NSW
David Alexander Stewart MBChB, FRACS (Plast), Visiting Medical Officer, Department of Hand & Peripheral Nerve Surgery, Royal North Shore Hospital, St Leonards, NSW; Senior Lecturer, Discipline of Surgery, Sydney Medical School, University of Sydney, Sydney, NSW
Robyn PM Saw MBBS, MS, FRACS, Melanoma Institute Australia, North Sydney, NSW; Head, Department of Melanoma and Surgical Oncology, Royal Prince Alfred Hospital, NSW; Associate Professor, Discipline of Surgery, Sydney Medical School, University of Sydney, NSW. robyn.saw@melanoma.org.au
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.