Case
A man aged 49 years presented to a general practice facility with a painful red right eye and associated photophobia and epiphora.
On examination, unaided visual acuity was 6/12 and 6/24 on the right and left eyes respectively, correcting with pinhole to 6/9 bilaterally. Pupils were equal and reactive to light. Lash collarettes were noted bilaterally. The bulbar conjunctiva of the right eye was injected. At the inferotemporal aspect of the cornea there was a crescent-shaped dense, white opacity.
Question 1
What common conditions can present with a unilateral, painful red eye? What serious conditions need to be excluded?
Question 2
What tests or investigations can be performed by a general practitioner (GP)?
Question 3
What additional history may be useful in refining differential diagnoses for a unilateral red eye?
Answer 1
Common differential diagnoses for a unilateral, painful red eye include:
- conjunctivitis – viral, bacterial or allergic
- chalazion
- dry eyes
- blepharitis
- corneal foreign body
- uveitis
- corneal abrasions
- keratitis (infective/non-infective)
- Herpes zoster ophthalmicus
- episcleritis.
Serious, sight-threatening differential diagnoses include:
- acute angle-closure glaucoma
- keratitis
- uveitis
- trauma - hyphaema
- scleritis
- Herpes zoster ophthalmicus
- endophthalmitis
- orbital cellulitis
- carotid cavernous fistula.
Answer 2
Investigations that a GP can perform are:
- fluorescein-staining assessment
- eye swabs – Herpes simplex virus (HSV), Varicella zoster virus (VZV), adenovirus and bacterial culture.
Answer 3
Additional history that may be useful in refining differential diagnoses for a unilateral red eye include:
- contact lens wear – concerning for microbial keratitis
- history of grinding/drilling – suspicious for metallic corneal foreign body
- history of trauma to the cornea (eg fingernail/stick to the eye) – suspicious for corneal abrasion
- history of autoimmune conditions – suspicious for acute anterior uveitis
- history of eye pain associated with nausea and vomiting – concerning for acute angle closure glaucoma
- history of facial erythema and rash – suspicious for ocular rosacea.
Case continued
Following instillation of fluorescein dye, the area of corneal opacification stained under cobalt blue light, indicating a corneal epithelial defect (Figure 1). The patient was referred to an ophthalmology clinic for review within 24 hours. At ophthalmology review, mild malar erythema and telangiectasia were noted, along with blepharitis. On questioning, the patient reported a previous diagnosis of acne rosacea, which had improved with avoidance of precipitating factors.
Question 4
What are the differential diagnoses after the findings at ophthalmology review?
Question 5
What treatment was indicated after ophthalmology review?
Answer 4
Given the findings at the ophthalmology review, the differential diagnoses include:
- microbial keratitis
- marginal keratitis
- autoimmune peripheral ulcerative keratitis.
The provisional diagnosis was marginal keratitis, associated with blepharitis and ocular rosacea.
Answer 5
A swab was performed for HSV and VZV testing by polymerase chain reaction (PCR). Despite the diagnosis of marginal keratitis, the patient was commenced on 48 hours of hourly ofloxacin eye drops to treat possible microbial keratitis. This was to avoid the potentially devastating consequences of inadvertently treating microbial keratitis with steroids in the initial phase.
The patient was educated on the standard treatment for blepharitis (eyelash scrubs and eyelid massage) and was instructed to perform this twice daily. Forty-eight hours later, his pain, photophobia and epiphora still persisted. Right visual acuity had improved to 6/9; however, the marginal infiltrate and conjunctival injection remained the same despite intensive topical antibiotics. HSV and VZV PCR results were negative. Topical anti-inflammatory prednisolone acetate drops were commenced four times daily once infective causes were excluded.
The patient was reviewed regularly over the following weeks. His symptoms resolved, as did the size of the marginal infiltrate. This was accompanied by slow tapering of the topical therapy. The marginal keratitis healed with a residual corneal stromal scar, which was visually insignificant due to its peripheral location.
Discussion
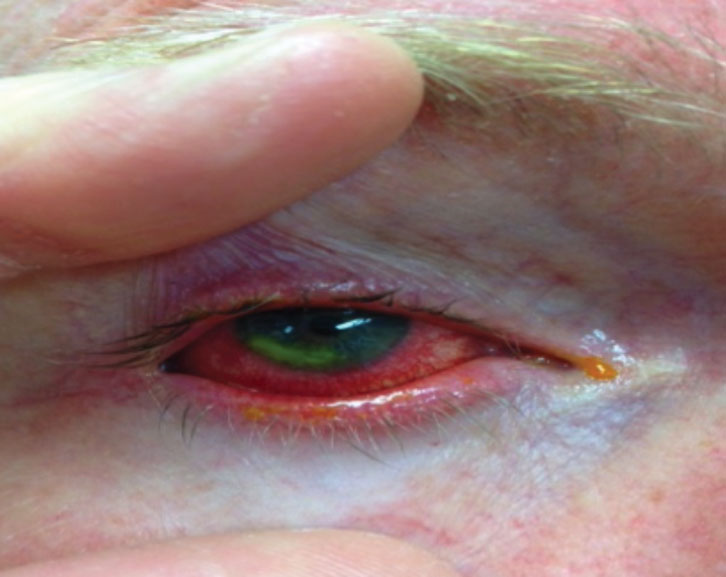 |
| Figure 1. Patient’s right eye after fluorescein staining |
Marginal keratitis is an inflammatory condition of the peripheral cornea secondary to chronic blepharitis, which can be associated with ocular rosacea. Patients usually present with a foreign body sensation or pain, epiphora, photophobia and, occasionally, reduced visual acuity. Typically, the inflammatory lesion is separated from the limbus by a clear margin. Initially, the overlying epithelium is intact; however, if left untreated this breaks down, creating an epithelial defect (Figure 1). The lesion spreads radially along the margin of the limbus.
Rosacea is a common cutaneous condition affecting about 10% of the adult population.1,2 Approximately 58–72% of patients may have ocular manifestations in the form of eyelid and ocular surface inflammation.1,3,4 Common presentations of ocular rosacea include blepharitis, conjunctivitis, meibomian gland dysfunction, chalazion and, less commonly, marginal keratitis (33%),1,4 which, although rarely, can lead to corneal perforation.5
Despite these common ocular presentations, ocular rosacea is frequently under-diagnosed.6 Diagnosis is based on clinical features and can be challenging, as up to 90% of patients may have subtle or no accompanying roseatic skin changes.1 Studies have demonstrated that efforts to enquire about ocular symptoms in dermatology patients and skin symptoms in ophthalmology patients favour an earlier and more accurate diagnosis of ocular rosacea.1
Key points
- Rosacea, although common, is often overlooked by general practitioners. Ocular rosacea, in particular, is frequently under-diagnosed.
- Diagnosis relies on a high level of suspicion, and clinical observation of characteristic skin and ocular manifestations.
- Clinicians’ increased awareness of ocular findings will aid earlier diagnosis and treatment, preventing permanent ocular injury.
- It is paramount to distinguish between microbial and non-microbial marginal keratitis, and to treat a possible infective cause prior to any addition of topical steroids. Specialist ophthalmological opinion should be sought if there is any doubt of diagnosis.
Authors
Amali F Navaratna MBBS, FRACGP, DCH, General Practice Registrar, Balmain Hospital GP Casualty and Hospital in the Home, Balmain, NSW. amali_ fernando@yahoo.com
Alannah Walsh MBBS, BLibStuds, Ophthalmology Registrar, Sydney Eye Hospital, Sydney, NSW
Parker Magin PhD, FRACGP, Medical Educator, General Practice Training – Valley to Coast, and Conjoint Professor, Discipline of General Practice, University of Newcastle, Sydney, NSW
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgments
Dr Owen Hutchings, Director, Balmain Hospital GP Casualty and Hospital in the Home