Case
John, 72 years of age, presented with acute vestibular syndrome (AVS), a sudden onset of severe vertigo associated with nausea and vomiting. He described several hours of ‘light headedness’ and ‘feeling giddy’, which did not change relative to his position. There was no associated tinnitus or diplopia. His medical history included type 2 diabetes mellitus, hypertension and gout.
On examination, John had an elevated blood pressure of 210/104 mmHg, and a heart rate of 84 beats per minute that is regular. The three-step bedside oculomotor examination revealed a normal horizontal head impulse test, direction-changing nystagmus, and vertical ocular misalignment. The rest of his neurological examination was normal.
Question 1
What is the role of the three-step bedside oculomotor examination?
Question 2
How is the horizontal head impulse test performed?
Question 3
How does nystagmus associated with peripheral lesions differ from nystagmus associated with central lesions?
Question 4
How is the single cover test performed?
Question 5
On the basis of the examination findings, is John more likely to have a peripheral or central cause for his AVS?
Answer 1
In patients who present with AVS, the three-step bedside oculomotor examination is particularly good at screening for acute infarction, which may be missed on imaging. The findings of a normal horizontal head impulse test, direction-changing nystagmus and vertical ocular misalignment have 100% sensitivity and 96% specificity for stroke,1 making this examination more sensitive than early magnetic resonance imaging (MRI) for stroke.
Answer 2
The horizontal head impulse test is performed by asking the patient to keep focusing on an object while the examiner turns the patient’s head from side to side. For example, ‘look at my nose, now let me turn your head, and keep your eyes on my nose’. A normal vestibulo-ocular reflex (VOR) to rapid, passive head rotation is an equal and opposite eye movement that keeps the eyes stationary in space (ie the eyes remain focused on the target; Figure 1). Conversely, an abnormal VOR is when a patient is unable to maintain fixation during head rotation towards the side of the vestibular lesion, requiring a corrective gaze shift once the head stops moving (Figure 2).
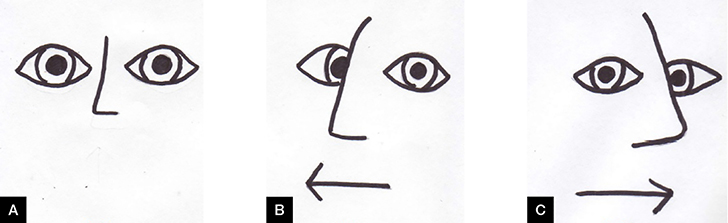 |
Figure 1. Normal vestibulo-ocular reflex
(A) Patient fixes gaze on examiner’s nose. Patient maintains visual fixation when head thrust to right (B) and left (C) |
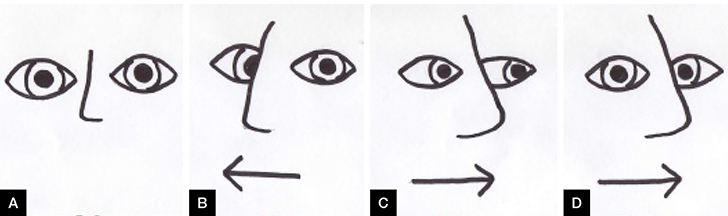 |
Figure 2. Abnormal vestibulo-ocular reflex
(A) Patient fixes gaze on examiner’s nose. Patient maintains visual fixation when head thrust to right (B), but not so on head thrust to left (C), requiring corrective gaze shift (D). Findings suggestive of left-sided peripheral vestibular lesion |
In a patient with AVS, a normal VOR by horizontal head impulse test strongly indicates a central localisation.2 An abnormal VOR is a predictor of peripheral localisation.2 For example, the findings of an abnormal or positive horizontal head impulse test to the left, and a normal or negative head impulse test to the right, is suggestive of a left-sided peripheral vestibular lesion.
Answer 3
Nystagmus associated with acute peripheral vestibular lesions such as in vestibular neuritis is typically horizontal and torsional.3 It increases in intensity when the patient looks in the direction of the nystagmus fast phase. For example, a left-beating nystagmus increases when a patient looks to the left. Conversely, the nystagmus tends to decrease and can disappear altogether when the patient gazes in the direction of the slow phase, but it never changes direction.1 Nystagmus associated with central lesions can also be unidirectional but may change direction with change in gaze direction.3
Answer 4
The single cover test, also known as the cover-uncover test, checks for skew deviation, also known as vertical ocular misalignment.1,4 It involves the patient fixating on a target and then covering each eye in turn. The examiner watches the eye as it is uncovered for any vertical re-fixation saccades. These saccades are a result of vertical ocular misalignment from right–left imbalance of vestibular tone.5 This test indicates if there is more or less neural firing to the oculomotor system on one side than the other. It is generally a central sign, indicating posterior fossa pathology, and is most commonly seen with brainstem strokes.5
Answer 5
The examination findings are most consistent with a central cause for AVS.
Conclusion
John’s cerebral MRI revealed an acute right-sided posterior, inferior cerebellar artery infarct. He was referred to a tertiary centre and worked up for his stroke. John’s cardiovascular risk factors, including diabetes mellitus and hypertension, were reviewed and optimised. He was started on aspirin and atorvastatin for secondary prevention against further strokes, and underwent a period of in-patient rehabilitation.
Key points
- Vertigo is a symptom of illusionary movement.
- Vertigo is due to dysfunction of the labyrinth, vestibular nerve or central vestibular structures in the brainstem.
- Bedside testing is very useful in helping to differentiate between peripheral and central causes of AVS.
- The three-step bedside oculomotor examination appears more sensitive for stroke than early MRI in AVS.
Author
Emma Foster MBBS (Hons), Neurology Registrar, Alfred Health, Neurosciences Department, Prahran, Vic. dr.ecfoster@gmail.com
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The author would like to thank Dr Anthony Fok, neuro-ophthalmologist, and Dr John Waterston, neuro-otologist, for their valuable input.