In early 2016, following local consultation, the Australian and New Zealand Committee on Resuscitation (ANZCOR) released the latest updates to its resuscitation guidelines,1 which are based on the 2015 five-yearly international review of resuscitation science. The aim of this article is to inform general practitioners (GPs) about the changes that are relevant to general practice. The good news is that very little has changed overall and the resuscitation capability expectations for GPs remain much the same.
GPs are the medical role models in the community and, as such, are expected to remain up-to-date with current resuscitation practices. As one of the few specialities that has a continuing professional development requirement for regular renewal of cardiopulmonary resuscitation (CPR) competency, GPs are already demonstrating leadership in this area. Accredited courses on resuscitation offer one of the best ways to maintain competency in this area.
The lack of major changes in the guidelines is indicative of a relative lack of any new evidence and a desire not to implement changes without compelling supporting evidence. Table 1 contains a list of the relevant changes to first aid and resuscitation in the 2016 guidelines. The driving force behind new or updated guidelines is evidence-based medicine combined with the ease of teaching and delivery. The overarching statement that ‘any resuscitation is better than no resuscitation’ has been incorporated in the Australian Resuscitation Council (ARC) guidelines for the past 15 years. In this article, we provide a summary of the issues of relevance to general practice.
Table 1. Summary of relevant changes
|
Topics
|
Relevant changes
|
|---|
|
BLS – Breathing
|
- Emphasise the value of breaths
- Starting CPR with breathing or compressions is equally acceptable in children
|
|
BLS – Compressions
|
- Rate now 100–120 compressions per minute
|
|
First aid – C spine
|
- Cervical collar is no longer recommended in first aid
|
|
First aid – Shock
|
- Leg elevation is no longer recommended
|
|
First aid – Bleeding
|
|
|
First aid – Anaphylaxis
|
- Second dose of adrenaline is recommended if it is needed
- In individuals prone to tick allergy, remove tick with freezing if possible
|
|
First aid – Asthma
|
- Four to six puffs of salbutamol via spacer
|
|
First aid – Stroke
|
- Blood glucose measurement is recommended if it is possible
|
|
First aid – Oximetry
|
- The recommended target is 94–98%
|
|
First aid –
Good Samaritan
|
|
|
ALS – Airway
|
|
|
ALS – Drugs
|
- Lignocaine as a second choice to amiodarone is recommended
|
|
ALS – Paediatrics
|
- Minimal changes; note the permissive commencement with either breaths or compressions in BLS
|
|
BLS, basic life support; CPR, cardiopulmonary resuscitation; LMA, laryngeal mask airway
|
Basic life support – The approach to resuscitation
The DRSABCD (danger, responsiveness, send for help, airway, breathing, CPR, defibrillator) resuscitation flowchart remains the gold standard for basic life support (BLS; Figure 1).
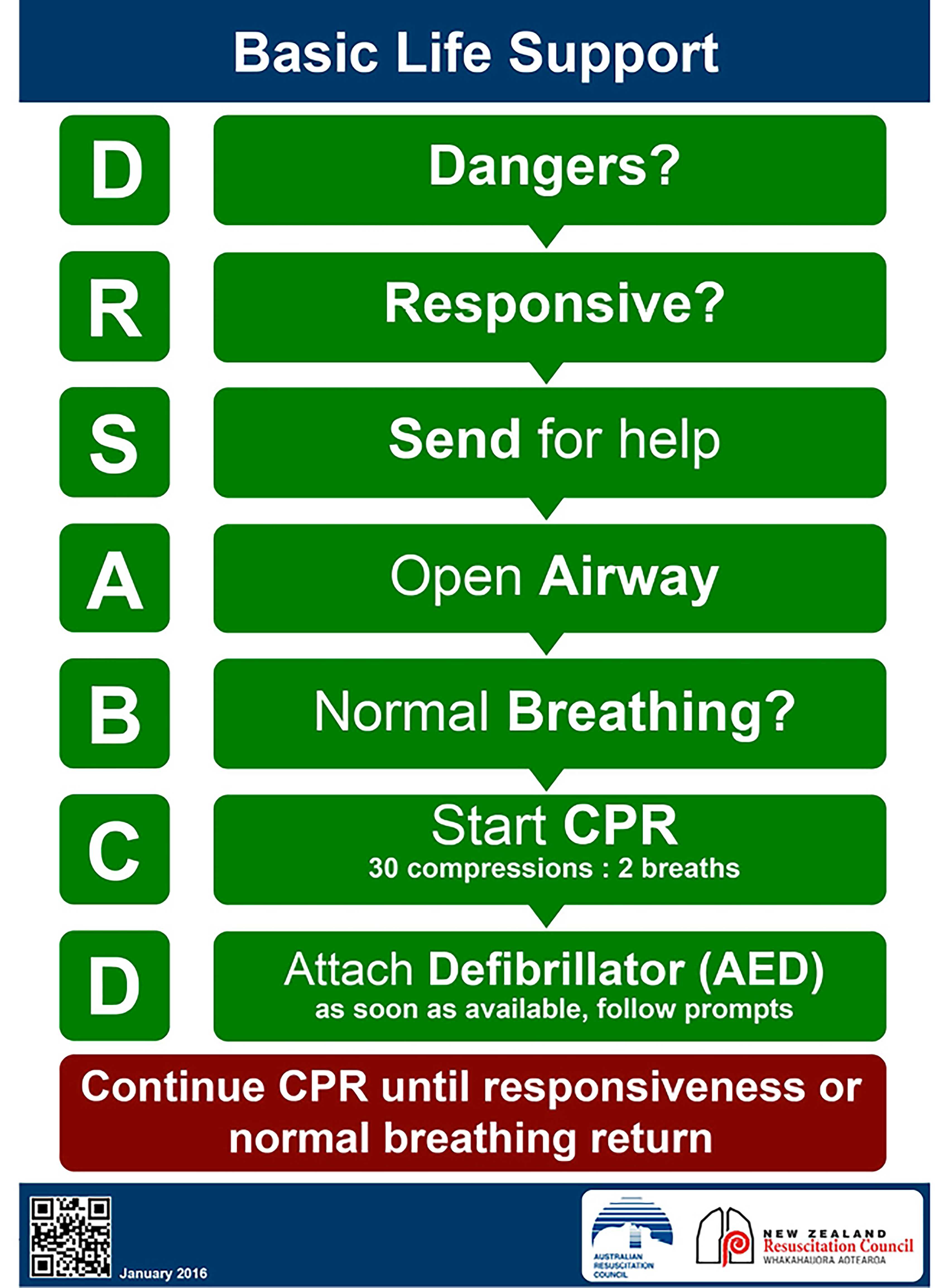
Figure 1. ANZCOR basic life support flowchart 1
Reproduced with permission from the Australian and New Zealand Committee on Resuscitation. Australian and New Zealand Committee on Resuscitation guidelines. Melbourne: ANZCOR, 2016. Available at https://resus.org.au/guidelines [Accessed 6 October 2016].
Airway
There are no changes in the recommendations for airway management. The rescuer should check that the airway is open with the patient on their back, and roll the patient to clear fluid obstruction if needed.
Breathing
The new guidelines emphasise the value of including ventilation in the CPR process; this is particularly important for health professionals. There has been no suggestion to remove ventilation from CPR except when giving telephone advice to untrained bystanders.
In paediatric resuscitation, the focus on supporting breathing is even more explicit. In trained hands, paediatric resuscitation is conducted at a ratio of 15:2 (compressions to ventilations) to allow for more breaths. Although many paediatricians would recognise children as a special circumstance and start CPR with breaths, it is considered equally acceptable to start with breaths or compressions for children.
Mouth-to-mouth resuscitation is still recommended and the use of a face mask or shield, if available, is advisable. While there is a chance of acquiring an infection that has a high transmission rate (eg influenza), the chances of acquiring a bloodborne infection are very remote.4
Compressions
For CPR, the compression-to-ventilation ratio is still 30:2 for adult resuscitation, and paediatric resuscitation carried out by a rescuer without paediatric experience. The new ideal compression rate is 100–120 compressions per minute, rather than just aiming for 100 compressions per minute. The compression point to aim for is the ‘middle of the chest on the lower half of the sternum’, and the compression depth is one-third of the depth of the chest.5
Defibrillation
While defibrillators are not yet mandatory for general practice accreditation, they are certainly becoming more widespread in the community. There is good evidence that during the first few minutes of resuscitation, each delay of one minute prior to defibrillation equates to approximately a 10% drop in the likelihood of a successful outcome.6 This information, which is in the public domain, has supported many GPs in acquiring defibrillators for their practices and meeting the community expectations of patients and families.
Updates to first aid guidelines
GPs should be aware of the current first aid guidelines as a guide to their own treatment and in order to support the teaching of first aid in the community.
Shock
The position recommended for a conscious person in shock continues to be the supine position. However, the role of passive leg raising has been downgraded on the existing evidence and is no longer recommended.7
Bleeding
For the control of bleeding, there was inadequate evidence to support the use of proximal pressure points or limb elevation. The use of localised cold therapy is suggested for closed bleeding in extremities. The use of haemostatic dressings in first aid is supported when standard first aid for haemorrhage control (eg direct wound pressure) fails to control severe bleeding or cannot be applied. The use of tourniquets in the civilian setting is also supported when standard first aid fails to control severe life-threatening bleeding. If a tourniquet is used in a life-threatening situation, it should be broad enough to prevent local damage and not applied over a joint.8
Cervical spine
There has been a significant change with respect to the management of suspected spinal injuries. The ANZCOR guidelines emphasise the value of looking after potential spinal injuries with good manual inline stabilisation. However, they have ceased recommending the use of semi-rigid collars in pre-hospital environments by first aid providers. This change in approach is because there is evidence of harm, but no evidence of any benefit, associated with the use of a semi-rigid collar. Where rigid spine boards are used, it is important to be aware of the potential for harm from tissue pressure and unintended shearing forces on the spine. It is recommended that the time spent on these hard surfaces is minimised.3 ANZCOR has recently released a ‘frequently asked questions’ statement relating to changes to this guideline.15
Medical emergencies
The use of a second dose of adrenaline for anaphylaxis via an auto-injector or intramuscular injection is now recommended when a first dose fails to improve symptoms.9
For those working in areas where ticks are a problem and anaphylaxis might occur in response to tick bite, it is worth noting that the best recommendation for tick removal in an allergic person is to freeze the tick prior to attempting removal (eg using dry ice spray, wart remover or equivalent, if available).10
Aspirin administration by first aiders is now recommended for people with a suspected heart attack (no longer only when directed to do so).
For asthma emergencies, the new recommendation is to give four to six puffs of reliever via a spacer and wait four to six minutes before repeating.
To improve stroke diagnostic accuracy, it is recommended that first aid providers who are trained in the use of a glucometer measure the blood glucose of people with suspected stroke.11
The guidelines support the use of pulse oximetry by first aid providers. Oxygen is given until the oximetry is known when a target of 94–98% is recommended in normal situations.
Lastly, the medico-legal section of the guidelines has been updated so that it is in line with legislative changes in various jurisdictions. The take home message is that a bystander who attempts to render assistance in a first aid situation is covered under a variation of the ‘Good Samaritan’ law or clauses in all Australian states and territories, and cannot be sued.12
Advanced life support
Airway
The ANZCOR guidelines emphasise the use of a laryngeal mask airway (LMA) or other supraglottic airway as an advanced airway management device.2 The advantage of LMA is that it can be inserted without interrupting CPR, and does not require direct vision or use of a laryngoscope. These devices are increasingly being stocked in general practices as part of their emergency kit.
Resuscitation drugs
In the cardiac arrest scenario, lignocaine (100 mg intravenous [IV]) is considered a reasonable alternative anti-arrhythmic to amiodarone (300 mg IV). This is particularly relevant to GPs as amiodarone is not available in the doctor’s bag.13
In the ‘Acute coronary syndrome’ guideline, the value of antiplatelet agents is noted, but no specific agent is recommended over another.
Advanced life support flowchart
As is the case with BLS, the advanced life support (ALS) flowchart (Figure 2) begins with the importance of commencing CPR and applying a defibrillator, either an automated external defibrillator (AED) or a manual model. Repeating cycles of two minutes of CPR followed by rhythm checks is the basis of the flowchart. An AED will advise the timing of the cycles and whether to provide a shock. If using a manual mode, the shockable rhythms are ventricular tachycardia and ventricular fibrillation; the non-shockable rhythms are pulseless electrical activity (PEA) or asystole.
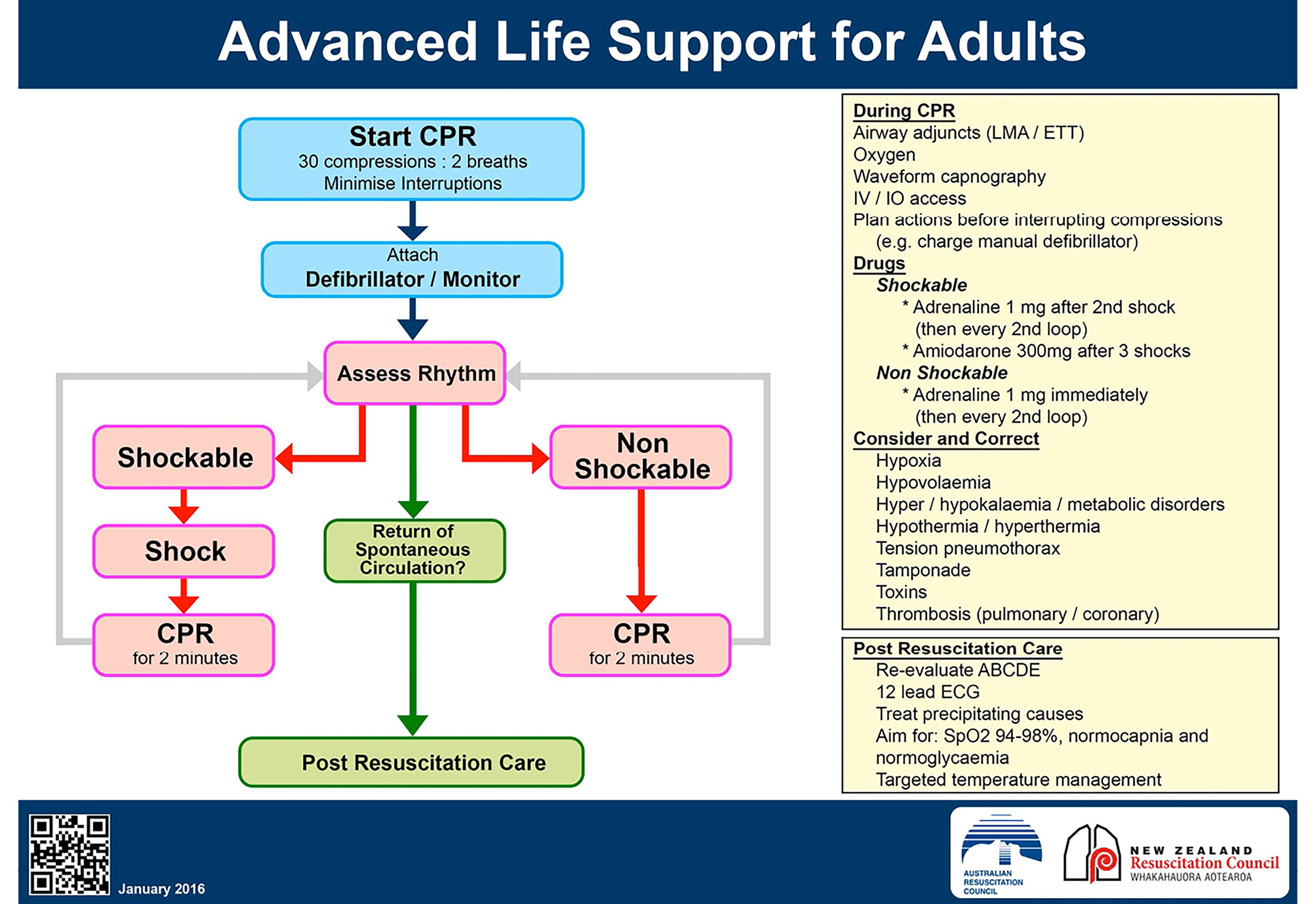
Figure 2. ANZCOR’s advanced life support flowchart 1
Reproduced with permission from the Australian and New Zealand Committee on Resuscitation. Australian and New Zealand Committee on Resuscitation guidelines. Melbourne: ANZCOR, 2016. Available at https://resus.org.au/guidelines [Accessed 6 October 2016].
When operating in an ALS mode, additional interventions are recommended during CPR. These interventions include insertion of an advanced airway device (eg LMA/supraglottic airway or endotracheal tube), provision of oxygen and obtaining IV or intraosseous access to allow medications to be given parenterally. Any interruption to the CPR should be minimised and planned in advance.14
For a shockable rhythm, 1 mg of adrenaline should be given after the second shock and then every second loop; 300 mg of amiodarone (or 100 mg of lignocaine) should be given after the third shock. For a non-shockable rhythm, 1 mg of adrenaline should be given as soon as possible and then every second loop.
During resuscitation, it is also important to look for reversible causes and consider the ‘4Hs and 4Ts’ as listed on the flowchart (Figure 2). Should return of spontaneous circulation (ROSC) occur, the recommendations for post-resuscitation care should be followed.14
Paediatric advanced life support
The paediatric advanced life support flowchart (Figure 3) is very similar to the adult version (Figure 2). Energy settings for defibrillation are 4 J/kg. As a manual defibrillator is calibrated in increasing energy steps, the next energy level above 4 J/kg is selected. The manufacturers recommend that an automatic defibrillator may be used in individuals over the age of 8 years. There are also paediatric adapters that are available for use with AEDs to accommodate smaller children. The dose of adrenaline is 10 µg/kg and amiodarone is 5 mg/kg.
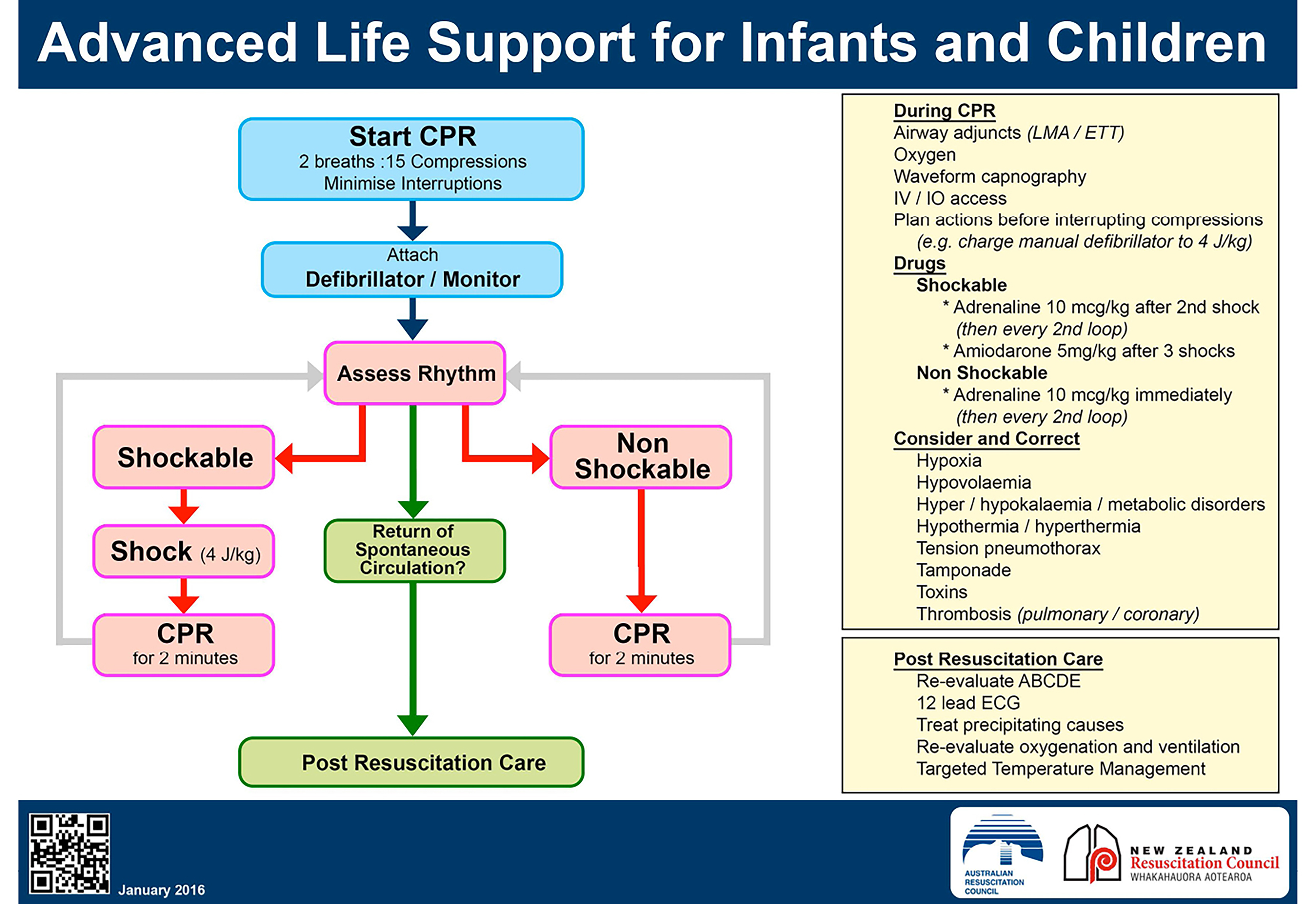
Figure 3. ANZCOR’s paediatric advanced life support flowchart 1
Reproduced with permission from the Australian and New Zealand Committee on Resuscitation. Australian and New Zealand Committee on Resuscitation guidelines. Melbourne: ANZCOR, 2016. Available at https://resus.org.au/guidelines [Accessed 6 October 2016]
Conclusions
GPs play an important role, not only providing immediate resuscitation in accordance with the ANZCOR’s guidelines, but also as visible community leaders and role models in resuscitation. The 2016 changes are relatively minimal, and are based on evidence and ease of teaching.
Resources
- ANZCOR’s updated guidelines, flowcharts and all available statements can be found on the ARC website (www.resus.org.au). Questions, comments or feedback relating to any of the guidelines should be sent to the RACGP representative for the ARC: rchr@unimelb.edu.au
Authors
Hugh Grantham ASM, MBBS FRACGP, Professor of Paramedics, Assistant Dean Student Affairs School of Medicine, Flinders University, Adelaide, SA; State Chair SA ARC; BLS Chair ANZCOR. hugh.grantham@flinders.edu.au
Rowena Christiansen BA (Hons), LLB, GradDipEd, MBA, MBBS, ACCAM, DCH, MEH, GradCert Space Studies, Associate Fellow, Aerospace Medical Association; RACGP Representative for the ARC; Medical Educator, University of Melbourne Medical School, Parkville, Vic; Medical Officer, Ormond College, University of Melbourne, Parkville, Vic; Chair, Australian Ski Patrol Medical Association Medical Advisory Committee and ARC Victorian Branch Representative.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.