Epistaxis is a challenging and common condition. The lifetime incidence of epistaxis is difficult to determine, but has been reported to be as high as 60%. However, only a very small proportion requires specialist management.1 Many patients self-manage this condition as it is often spontaneous and self-limiting. They present to their general practitioner (GP) only when the condition changes or worsens. Application of proper first aid is often all that is required. Patients rarely need to be transferred to a hospital with the aim of being treated by an ear, nose and throat (ENT) specialist. As most episodes are minor, the GP’s role is important in recognising signs and symptoms suggestive of more sinister medical conditions.
The management of epistaxis has evolved significantly in recent years. Successful treatment requires knowledge of the possible causes of epistaxis and a detailed knowledge of nasal anatomy.
Anatomy
The nose has a rich vascular anatomy with multiple anastomoses. The arterial supply arises from branches of both the internal and external carotid arteries (Figure 1). The ethmoidal arteries, branches of the internal carotid, enter the nose superiorly and supply the upper extremes of the septum and lateral nasal wall. The facial and the internal maxillary artery are the two branches involved in the supply of the nasal cavity and are part of the external carotid. The internal maxillary divides into six branches and includes the greater palatine and sphenopalatine arteries (SPA). These contribute to Keisselbach’s plexus and supply up to 80% of the nasal vault. The facial artery is the second major branch of the external carotid to supply the nose, which also contributes to Keisselbach’s plexus.
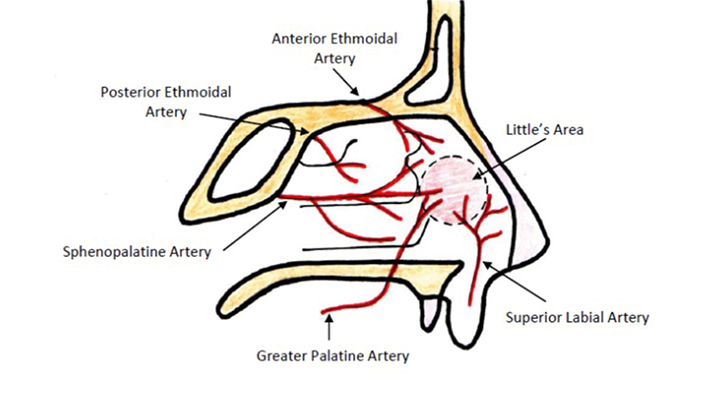 |
| Figure 1. Blood supply to the nasal septum |
Classification
Epistaxis is most commonly classified into anterior or posterior bleeds. This division lies at the piriform aperture anatomically. More than 90% of episodes of epistaxis occur along the anterior nasal septum, which is supplied by Keisselbach’s plexus in a site known as the Little’s area.2 The Keisselbach’s plexus is an anastomotic network of vessels located on the anterior cartilaginous septum. It receives blood supply from both internal and external carotid arteries.
Approximately 10% of episodes of epistaxis are posterior bleeds. Posterior bleeds are most commonly arterial in origin. It presents with a greater risk of airway compromise, aspiration and difficulty in controlling the haemorrhage.1
Epistaxis can also be divided into primary or secondary. Primary causes account for 85% of episodes and are idiopathic, spontaneous bleeds without any notable precipitant. Bleeds are considered secondary if there is a clear and definite cause (eg trauma, anticoagulant use, post surgical).3
Aetiology
The cause of epistaxis can be divided into local, systemic, environmental, medications or, in the majority of cases, idiopathic.1 Approximately 7–14% of the adult population will have experienced epistaxis at some point in their life.3,4 A thorough history and examination are vital in assisting with clinical decisions regarding further investigations and management.
Local
Local causes of epistaxis include trauma, neoplasia, septal abnormality, inflammatory diseases and iatrogenic causes. Local trauma is common among children who present with post-digital trauma or irritation. Causes such as neoplasia are uncommon. However, eliciting significant signs and symptoms is important. Uncommon causes, such as neoplasia, need to be ruled out through a thorough history and examination. Red flags for neoplasia include:5
- unilateral nasal blockage
- facial pain
- headaches
- facial swelling/deformity
- South-East Asian origin (nasopharyngeal carcinoma)
- loose teeth
- deep otalgia.
Systemic
Examples of the systemic causes of epistaxis include age, hypertension, bleeding diathesis and alcohol. Epistaxis can occur in any age group, but predominately affects the elderly (50–80 years of age) and children (2–10 years of age). If an adolescent patient presents with epistaxis, it is important to consider other causes such as cocaine use or juvenile nasopharyngeal angiofibroma.6 Juvenile nasopharyngeal angiofibroma is a benign tumour that can bleed extensively. Other symptoms suggestive of this condition include nasal obstruction, headaches, rhinorrhoea and anosmia.6
Patients with hereditary haemorrhagic telangiectasia can present with epistaxis refractory to usual treatment methods.4 It is also common for patients with other bleeding disorders, such as Von Willebrand’s disease, to present with recurrent epistaxis. Further laboratory testing and consultation with a physician may be warranted if a bleeding diathesis is suspected.4
The association between hypertension and epistaxis is often misunderstood. Hypertension is rarely the direct cause of epistaxis, and is perhaps related to underlying vasculopathy in this group of patients. It has been suggested that hypertension may be related to anxiety, but studies have failed to find conclusive evidence.3
Other factors, such as alcohol, have also been shown to increase the risk of epistaxis. Studies found patients who present with epistaxis were likely to have consumed alcohol within 24 hours of hospitalisation. This relationship is thought to be related to decreased platelet aggregation and prolonged bleeding time.5
Environmental
The number of presentations of epistaxis has been found to increase during the dry winter months, often associated with changes in temperature and humidity.7 The incidence of epistaxis is also related to circadian rhythm, with peaks in the morning and late afternoon.4
Medications
The use of many over-the-counter and prescribed medications can alter coagulation. Nonsteroidal anti-inflammatory drugs (NSAIDS), warfarin, clopidogrel and the increasingly popular oral factor X inhibitors are commonly used medications that can affect clotting. It is imperative, therefore to take a thorough medication history. The use of complementary and alternative medicine must also be considered. Their use is increasing and can interfere with regular medications and clotting.3
History
What to ask about
Clinical stabilisation, including the control of significant bleeding, should always take priority over obtaining a lengthy history.
Questions should focus on the history of the acute episode and previous episodes, including duration, severity, frequency and laterality of bleed.1 Patients with posterior epistaxis can often bleed from both nostrils and it can feel as though blood is dripping down their throat rather than their nose. The methods they used to control previous episodes are significant from an education perspective. It is unfortunate that pinching over the nasal bones, rather than the soft cartilaginous tip, remains commonplace. It is important to ask questions about haematemesis and malaena. Upper gastrointestinal bleeding can often be overlooked in patients with epistaxis.4 It is also important to look for signs and symptoms of anaemia, which can give clues to the severity of bleeding.
To further define the cause of bleeding, clinicians should ask about local trauma, including nose picking, possible foreign body or current upper respiratory tract infection. Foreign bodies inserted in the nose are important, as objects such as batteries can cause significant damage and may lead to a medical emergency.1
A thorough medical history can give clues to the cause of bleeding. Significant history, including a history of hepatic impairment, hypertension, easy bruising or bleeding, or a family history of coagulation disorders, is important in epistaxis.1
Social history such as alcohol, smoking and recreational drug use is also significant. Questions should be asked specifically about cocaine use.
Anticoagulant use is an important aspect of history taking. It will not only increase the risk of bleeding, but can also alter management of the patient.
Management
Resuscitation
Primary first aid is a priority in a patient who presents with epistaxis and this includes the ABCs of resuscitation (airway, breathing, circulation). Clinicians need to assess patients for haemodynamic stability, including pulse and respiratory rate, and look for signs of shock, such as sweating and pallor. If the patient is actively bleeding, sit them upright. Lean the patient forward to minimise swallowing of blood and apply digital pressure at the cartilaginous part of the nose for a minimum of 10 minutes. Insert a large-bore intravenous cannula and, if appropriate, take a blood sample (for full blood evaluation and blood group determination) and hold. Consider transfer to an emergency department, or referral to an ENT specialist if bleeding continues. The urgency of this transfer will depend on the clinical situation at the time, but given the age distribution of epistaxis, prompt management is paramount.
Assessment
Preparation is key in the assessment of a patient with epistaxis. Position the bed at the correct height, have sufficient lighting, suction, eye protection, gloves and mask. Ensure the equipment is easily accessible and assistance is available. Access to a hands-free light such as a headlight is ideal as this will enable the use of both hands to assess and treat the patient further.
To get a good view, it may be necessary for the patient to blow their nose and clear any clots. Be aware that this may lead to a recurrence of bleeding but could assist in identifying the bleeding point. With a nasal speculum in one hand, attempt to view the nasal cavity while suctioning simultaneously with the other hand. A systematic examination of the nasal cavity should be performed. Pay particular attention to the septum and Little’s area for an anterior bleed, and remember also to look for scabbed or excoriated areas.
It may be appropriate at this point to prepare the nose with adequate anaesthesia and a vasoconstrictor agent, depending on the examination findings. A well-primed nose is invaluable. Apply a topical spray such as 5% lignocaine with 0.5% phenylephrine to both nostrils.6 Alternatively, an unravelled cotton ball can be soaked with the spray and carefully inserted into the nasal cavity.4 The use of topical sprays reduces haemorrhage to allow for better visualisation and analgesia for possible cautery or nasal packing.
Posterior bleeds need to be considered if an anterior bleeding site is not visualised on examination. Clues include bilateral bleeding from both nostrils, or blood may be dripping down the posterior pharynx. If there are further concerns, consider referral to an ENT specialist or emergency department. Nasendoscopy can be performed by an ENT specialist, with a rigid endoscope, and the source of bleeding can be identified in a further 80% of cases.3 Most patients tolerate this procedure with the use of topical anaesthesia. Rigid endoscopy allows for inspection of the entire nasal cavity including the nasopharynx to examine for posterior bleeds.1
Cauterisation
Management of an anterior bleed can often be performed safely in primary care, provided appropriate equipment is available along with appropriate follow-up. Options include cautery or nasal packing if direct pressure fails to stop the bleeding. Cautery sticks are impregnated with silver nitrate, which reacts with the mucosal lining to produce a chemical burn.8 Care must be taken during bilateral cautery to prevent septal perforation and treatment should only be administered to a small area surrounding the bleeding point. After cauteristation, patients should then be placed on a nasal moisturiser such as Kenacomb or paraffin.
Nasal packing
If cauterisation is unsuccessful in controlling the bleed, or if no bleeding point is seen on examination, anterior or posterior nasal packs are available.
Anterior nasal packs work by applying direct mechanical pressure on the site of the bleeding. Traditional methods used lubricant or antibiotic-soaked ribbon gauze; however, modern packs have been developed for simple insertion and are effective. The Rapid Rhino has an inflatable balloon coated in a compound that acts as a platelet aggregator.4 The balloon is inflated after insertion, to tamponade bleeding, and can be left for up to 3–4 days.1 Care must be taken when inserting a nasal pack. Use a firm but not forceful hand to direct the pack posteriorly, along the floor of the nasal cavity rather than superiorly. The correct placement will allow the entire length of the pack to be inserted.
Posterior packing may be required if the bleeding continues despite anterior packing. Commonly used posterior packs include balloon catheters. In combination with an anterior pack, a posterior pack is placed to tamponade the area of choanae and sphenopalatine foramen.2 A Foley catheter is inserted along the floor of the nasal cavity into the posterior pharynx. The balloon is then inflated and retracted anteriorly to sit in the nasopharyngeal space.4 A clamp is used to secure the device. The nose should then be packed anteriorly, using materials such as Kaltostat or ribbon gauze to tamponade any potential anterior bleeds. The clamp and Foley’s catheter must be regularly reviewed by the nursing staff as there is a risk of pressure necrosis on the nasal tip. It is recommended that insertion of a Foley catheter be performed only by a clinician who has been trained in this skill.
The use of nasal packs can have complications. Oral antibiotics are usually prescribed as a prophylactic measure against toxic shock syndrome while the packs are in situ.4 The duration and use of oral antibiotics is consultant, clinician and department dependent. Given that this condition is rare, there is little convincing evidence in the literature around the use of prophylactic antibiotics. Other complications from the use of nasal packs include acute sinusitis and obstruction of the nasal airway, leading to sleep apnoea or hypoxia.8 Patients with posterior packing, as well as bilateral packs, are at a higher risk of hypoxic episodes, myocardial infarction, cerebrovascular accident and death. This can often result in being admitted to the intensive care unit for monitoring.9
Arterial ligation
If epistaxis continues despite packing, surgical options may be considered. There are three main types of surgical options: external carotid artery ligation, internal maxillary artery ligation or SPA ligation.8 The decision around which artery to ligate will depend on the site of bleeding and its likely source. The aim will be to ligate as close as possible to the site of bleeding.
Endonasal ligation of the SPA is the most specific and currently the most widely used technique.8 Studies have shown that ligation of the SPA can control 98% of posterior epistaxis.10 Patients are placed under general anaesthetic, an incision is made at the lateral nasal wall, a mucosal flap is raised, and the SPA is identified. The vessel is then clipped, divided or coagulated with diathermy. Recognising variations in the anatomy is important in the success of this procedure. Risks with this procedure are rare, but include blindness, decreased lacrimation, local infection, infraorbital nerve injury, oroantral fistula, sinusitis and epiphoria.9
Embolisation
Angiographic embolisation in epistaxis is another method of controlling bleeding. Access to the vascular system through a femoral punch leads to identification of the bleeding point. A catheter is then placed in the internal maxillary artery and the bleeding vessel is embolised. The success rate of this procedure is high, although not without risk. Major complications such as cerebrovascular accidents and blindness can occur in up to 4% of cases.2 It remains a strong alternative to SPA ligation in posterior epistaxis for patients who are medically unfit for general anaesthesia, or who have had a failed SPA ligation.
Follow-up and patient education
It is important for patients with epistaxis to be followed up by a GP or specialist, depending on the severity of their condition. Patients need to be educated about proper first aid, should they have a recurrence of epistaxis. Patients should apply digital pressure at the cartilaginous part of the nose for a minimum of 10 minutes without letting go. They should be advised to sit up, lean forward and use an ice pack, and to attend the nearest emergency department or local medical officer if bleeding continues. If the cause of the bleeding is unknown or suspicious, appropriate investigations and referrals should be sought. Patients should avoid hot foods, strenuous activity, digital trauma and nose blowing on discharge from hospital. Patients should also be prescribed a topical ointment such as Kenacomb, Nasalate or paraffin for 7 days. This ensures moisturisation of the nasal mucosa and reduces the risk of bleeding recurrence.
Conclusion
Epistaxis continues to be a common presentation to GPs and can quickly escalate into a medical emergency. Simple procedures and principles can be effective in managing epistaxis until the patient can be treated in hospital. For most patients, simple first aid is all that is required to control this, often self-limiting, condition. However, this requires the general public and those prone to nosebleeds to have the correct education regarding this condition. Advances in the management of epistaxis will allow it to continue to evolve to an outpatient managed condition. This therefore leads to financial and patient benefits.
Author
Stephanie Yau MBBS, ENT Non-training Registrar, The Townsville Hospital, Townsville, QLD. stephstephyau@gmail.com
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.