General practitioner (GP) recruitment, migration and retention in rural and remote areas are issues of significant national importance in Australia1,2 and the US,3 given the well-documented shortages2–4 in rural areas in both countries. While the net flow of physicians from rural areas of the US is a well-studied topic,4 similar research from Australia is outdated, anecdotal, unpublished or based on small, focused samples.5 Australian researchers have studied the geographical mobility of recent medical graduates, with a focus on one6,7 or two states.5 While studying the mobility of medical trainees and graduates in local geographies is important, analysing the diffusion of established GPs in and out of rural areas on a national scale can yield important policy perspectives.
Studying the diffusion of GPs requires Australia-wide longitudinal data on GPs and their location. Researchers are beginning to harness longitudinal datasets, such as the Medicine in Australia: Balancing Employment and Life (MABEL) survey, for this purpose.8 While providing ‘depth’ information, surveys do not represent the entirety of the GP population, and are expensive and time-consuming to administer and analyse.5 By contrast, routinely collected administrative or membership databases, such as the American Medical Association’s Physician Masterfile, which was used in the US physician diffusion study,4 are relatively easy to obtain and analyse.
Similar national-scale studies have become possible in Australia since 2010, with the establishment of the Australian Health Professional Registration Agency (AHPRA). The AHPRA database includes a complete census of GPs in Australia who are registered as specialists in general practice. This database has some limitations (see Discussion), but it provides an invaluable source of national, longitudinal GP data including previously validated geographic location information.7
Our study used the AHPRA data for 2011and 2013 to answer two questions:
- What are the patterns of GP mobility across the urban–rural gradient in Australia?
- Is there a net flow of GPs from rural to urban Australia?
Our study does not aim to find the drivers of mobility among GPs, which datasets with greater depth, such as the MABEL survey, are in a better position to answer.
Methods
A list of all doctors with specialist registration in general practice in 2011 and 2013 was obtained from AHPRA. GPs’ names, postcodes or suburbs of the principal place of practice (PPP), and contact numbers, were available. Note that variables such as the GP’s age and ethnicity were not publicly available for reasons of confidentiality. The raw dataset from AHPRA had a total of 22,141 GPs in 2011 and 23,019 GPs in 2013 (Figure 1). This is markedly different from the approximately 30,000 GPs recorded in the Medicare system.9 The reason for the difference between the two systems is that general practice registrars, and doctors with general registration or other types of registration who provide general practice services, are not included as specialists in general practice in the AHPRA dataset.
After the removal of GPs with invalid or missing locations, the 2011 and 2013 datasets were linked using GPs’ contact numbers and names, resulting in a dataset of 21,274. Additional validity checks were implemented on the linkage process, for example, by matching names only, which achieved a slightly smaller level of matching (Appendix 1, available online only). The dataset was geocoded to the latitude–longitude at the geometric centre of the GP’s suburb and postcode locations, which offers greater locational precision than postcodes alone.10 These locations were then linked to Australian Bureau of Statistics (ABS) geographic Remoteness Areas (RAs).11 Valid RA information was available for 20,352 GPs in 2011 and 20,411 GPs in 2013; 20,072 GPs had valid RAs for both years. Figure 1 summarises the data creation flow and technical details of the linking, and geocoding process are provided in Appendix 1.
Summary statistics and tabulations of GP flows were calculated across RAs. Annual turnover (arrival and departure percentages) was estimated by calculating flows for the two years (2011 and 2013) and dividing by two. This provides a reasonable estimate of annual flows because the effects of compounding percentages are likely to be small over one year.
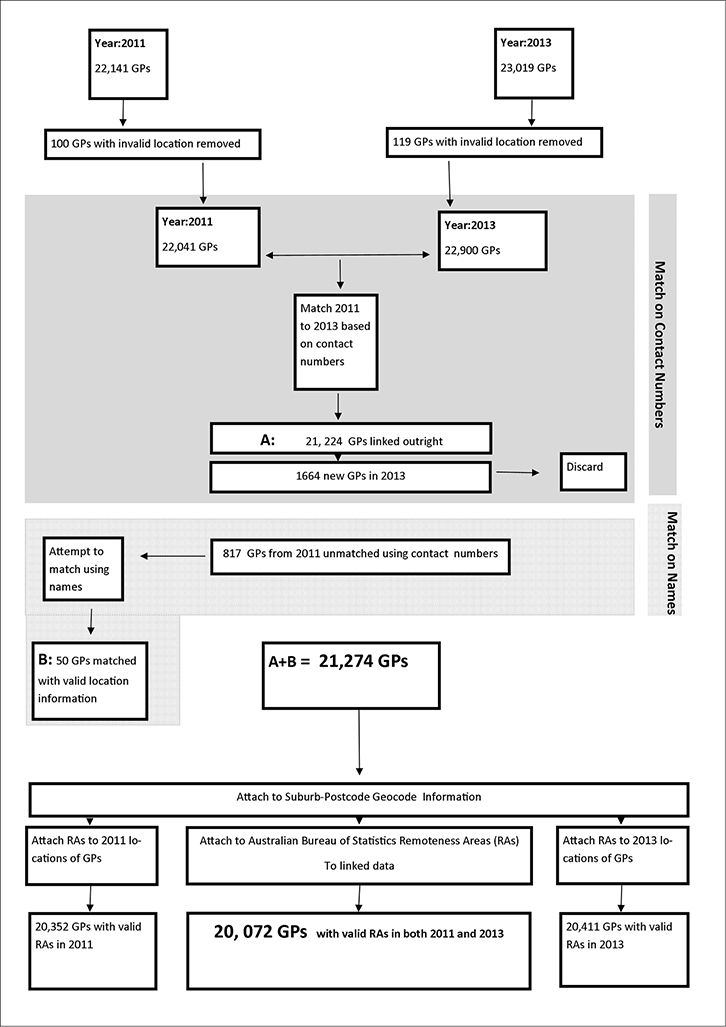 |
| Figure 1. Data linkage and flow |
Results
Between 2011 and 2013, 20.5% of GPs changed their PPP, which is equivalent to an annual rate of about 10%. Annually, about 1% of GPs moved between states. Table 1 shows diffusion out of the outer and inner regional and remote areas, and a net move into major cities. No net change was observed for very remote areas and the net change in remote areas was small. As the majority of GPs were located in major cities, most moves were by doctors in major city regions. The majority of moves in all RAs (except remote and very remote) were within the same category. While 94% of major city GPs who moved did so within major cities, 58% of GPs in inner regional and 55% in outer regional areas moved within the same RA. Fewer GPs changed PPP in remote areas (<26%) and very remote (<39%). Note that a GP who moves within an RA can be physically moving a long distance; for example, a GP may move from Sydney to Melbourne but stay within the major city RA, or may move long distances while staying within the remote or very remote area of a single state. Major cities remained the most favoured destination of GPs moving out of an RA, and the largest source of GPs moving into remote and very remote areas. Turnover was relatively high in very remote areas.
The modal distance moved represents the most frequent move by GPs. The modal distance moved by GPs was 1 km, dominated by major city GP moves (Table 2). However, there was a rapidly increasing gradient of distances moved with increasing rurality, and in 2011, the modal distance for those moving to very remote areas was almost 600 km.
Table 1. Pattern of GP geographic mobility in 2011 and 2013
|
|
Destination (2013)
|
|---|
|
|
|
Major city
|
Inner regional
|
Outer regional
|
Remote
|
Very remote
|
Total GPs who moved out of a practice
|
Average annual
turnover (departures) ‡,§
|
Total resident GPs in 2011
(20,352)
|
|
Source (2011)
|
Major city
|
2,855
|
146
|
52
|
14
|
*
|
3,076
|
10%
|
15,330
|
|
Inner regional
|
239
|
398
|
34
|
*
|
*
|
681
|
10%
|
3,403
|
|
Outer regional
|
82
|
41
|
160
|
*
|
*
|
293
|
11%
|
1,359
|
|
Remote
|
16
|
*
|
*
|
*
|
*
|
39
|
11%
|
184
|
|
Very remote
|
10
|
*
|
*
|
*
|
*
|
26
|
17%
|
76
|
|
Total GPs who moved into a practice
|
3,202
|
599
|
257
|
31
|
26
|
4,115
|
|
|
|
Average annual turnover (arrivals)%†,§
|
13%
|
11%
|
12%
|
11%
|
24%
|
|
|
|
|
Total resident GPs in 20134
|
15,507
|
3,330
|
1,318
|
176
|
80
|
|
|
|
|
Movements to more rural areas are in grey
*Indicates <10 persons
†Arrivals % is calculated as: (Total GPs that moved in)/Total resident GPs in 2013 – Total GPs that moved in)
‡Departures % is calculated as: (Total GPs that moved out)/(Total resident GPs in 2011)
§Annual averages were calculated by dividing the 2 year rates (Calculated as shown in †, ‡) by 2 (see Methods, Figure 1)
|
Table 2. GPs who moved practice from 2011 to 13: Modal distance moved by GPs when they move to a specific remoteness area
|
|
Remoteness area moved to
|
Modal distance moved (km)
|
|---|
|
Metropolitan
|
1
|
|
Inner regional
|
1
|
|
Outer regional
|
4
|
|
Remote
|
44
|
|
Very remote
|
599
|
|
Overall mode
|
1
|
Discussion
This is the first attempt to delineate a census of GP diffusion in Australia. The data clearly shows a drift from rural areas to major city areas. In all areas (except very remote areas), 10–13% of GPs move annually. While in agreement with emerging unpublished evidence, these percentages indicate a degree of ‘churn’ between practices within what is generally the same area; presumably, this arises as GPs move between practices without the dislocation of moving house. It is difficult to estimate the proportion of these GPs with the current data.
It is well known that professionals tend to avoid moving house over long distances without appropriate incentives, especially when issues such as spousal employment and children’s schooling are involved.12 Table 2 shows that Australian GPs face the prospect of moving large distances if they wish to move to rural and remote Australia, underscoring the need for strong rural relocation incentives.
The results of the analysis show a small drift away from rural areas, and the largest numbers of GPs move into or out of major city areas simply because this group has the greatest pool of GPs. While there is clearly some flow (in both directions) between the other rural and remote categories, the sizes of the flows are dominated by major city GPs. Thus, targeting of registered specialist GPs to work in rural areas must start in the major city areas, as the number of doctors in other areas is small. Targeting non-specialised GPs or general practice registrars outside the pool of registered specialist GPs is another established policy option.6
This study has a number of limitations. First, it included only GPs who were registered with AHPRA as specialising in general practice. Thus, it excluded general practice registrars, interns, other specialists, doctors with general, provisional or limited registration, and international medical graduates, who are not yet fully registered, but all of whom may offer varying degrees of general practice services. On the other hand, by providing a census of the specialist GPs and their flows, this study provides policymakers with a perspective on the size of the movements needed within the specialist GP pool, or from the other components of the GP market to compensate for these flows. Updating the PPP field is not mandatory on re-registration with AHPRA, resulting in possible underestimation of movement numbers.7 By contrast, overestimation could occur when GPs who work in a number of practices change PPP designation from one practice to another on the basis of shifting workloads while continuing to work in the same practices.7
A second limitation is that this study enumerates GPs on the basis of headcounts rather than workload, which may bias the analyses; for example, the loss or gain of a GP who works extra hours (as is the case with many rural GPs) is different from the loss or gain of a GP who works full-time or less than full-time.
Third, this research observed movement over a short period. Long-term trends in GP mobility4 will be able to be analysed as the national AHPRA database continues to grow with time. A fourth, minor limitation is that some GPs who were present in 2011 or 2013, but not both years, may bias the denominators of the mobility ratios. This may occur when GPs die or move abroad (present in 2011, absent in 2013), are new entrants to the workforce (absent in 2011, present in 2013) or are not matched by our algorithm.
Despite the limitations, the approximately 10% annual rate of movement reported by this study tends to agree with anecdotal reports and unpublished research. This study is therefore a call to health services researchers for additional research into GP mobility in Australia.
Implications for general practice
- This study shows, for the first time, that GPs move between practices at an annual rate of around 10%.
- GPs choosing to relocate to rural and remote areas face the prospect of moving long distances, requiring appropriate incentives for such a move.
- If the number of GPs is to be maintained in regional and remote areas, new doctors will be required to move to these areas to accommodate the drift away.
- Given that most of the movement is within RAs, incentives aimed at optimising moving within an area are likely to be successful.
- As the largest numbers of moves between areas are from major cities, targeting GPs to work in rural areas must start in the major city areas, as the pools of doctors in other areas are too small.
- The methods used in this study can be used for long-term surveillance of GP mobility in Australia, providing that AHPRA data are available in the future, to inform policy and research.
Authors
Soumya Mazumdar PhD, MPh,MSc, Research Fellow, The Centre for Research and Action in Public Health, University of Canberra, ACT, and Visiting Fellow, Australian Primary Health Care Research Institute, Australian National University, Canberra, ACT. soumyamazumdar@yahoo.com.
Ian McRae PhD, Visiting Fellow, Australian Primary Health Care Research Institute, Australian National University, Canberra, ACT
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Appendix 1. Data linkage and geocoding
Appendix 1A: Linking data from 2011 with 2013
The 2011 data consisted of 22,141 GPs and there were 23,019 GPs in the 2013 data. Of the GPs in 2011, 100 postcodes were found to be missing or internationally-based, and were therefore removed. Similarly, 119 GP postcodes were removed from the 2013 data. These records were discarded, resulting in a dataset of 22,041 GPs in 2011 and 22,900 GPs in 2013. We linked the 2011 data with the 2013 data using the contact numbers of GPs with robustness checks (discussed below). Using this matching method, 817 of the 22,041 GPs in 2011 GPs were not found in the 2013 data. Additionally, 1664 GPs appeared in the 2013 data that were not present in the 2011 data, resulting in a dataset of 21,224 GPs. We attempted to rematch the 817 GPs from the 2011 data whose contact numbers did not appear in the 2013 data using their first and last names instead. An additional 53 GPs were found and linked to the 2013 data. Three of the linked GPs from the group of 53 in the 2013 data had invalid location information. Thus, 21,274 GPs with seemingly valid location information were found in the 2011 and 2013 data. Note that some GPs may still have invalid location information in the form of post office boxes or misspelt suburbs, which would make them difficult to geocode and attach to remoteness area geographies. Figure 1 provides a diagrammatic outline of this process.
A number of robustness checks were implemented to verify the validity of this linkage. First, a rough visual inspection was implemented to verify that the matches were correct. Next, for the linked GPs, we compared the first and last names of the GPs between the 2011 and 2013 data. Only 58 GPs were identified to have their first, middle and last names not exactly the same between the two time periods. These names were inspected manually, and it was found that 57 GPs had changed their first, last or middle name (but never all three names together). Only one GP was found to have had the same contact number but a completely different name in the 2013 data. Given that 57 GPs had changed some aspect of their name, it was assumed that this GP had changed his name in its entirety and was thus not removed from the data.
To test an alternative matching procedure, we also attempted to use the first and last name of GPs to link the datasets, using the Jaro-Winkler algorithm and ‘A fine-grained record integration and linkage tool’ (FRIL) software.1 A somewhat smaller set of 21,078 GPs were matched using this approach.
Appendix 1B. Relating GP location to remoteness geographies
The suburb and postcodes (suburb-postcode) of all the GPs’ principal place of practice (PPP) were known. A list of latitude-longitudes for centroids of all suburb-postcode geographies in Australia was downloaded from an online repository.2 The authors of the online repository utilised the freely available Google geocoding ‘Application programming interface’ to geocode their data. Their methods can thus be easily reproduced, or the data can be obtained from the authors on request. By attaching the list of PPP suburb-postcodes to this list, the location of the PPP was surmised to be at the centroid latitude-longitude of the suburb-postcode combination geography. This process was implemented for the 2011 and 2013 data.
The preferred contact address of the GP was available in the dataset. However, it was not known if this address was residential or the place of practice. There is evidence from the US that biases are introduced from analyses that use physician mailing address instead of practice address,3 and hence, the PPP locations were used. To relate the location of a GP with geographic categorisations of remoteness, the PPP latitude-longitudes were spatially joined to Statistical Area-1 (SA-1) level remoteness information from the Australian Bureau of Statistics (ABS). The SA-1 is a fine aerial geography consisting of approximately 400 people.4 The location of the GPs in 2011 and 2013 in the linked data (21,274 GPs) were geocoded to the centroid of their suburb-postcode locations. Of the 21,274 GPs in the linked dataset, 20,352 GPs could be related to valid RA locations in 2011, 20,411 in 2013 and 20,072 for both years. Note that not all GPs could be attached to an RA because of invalid location information as discussed in Appendix. 1A.
Data management and geocoding were implemented in ArcGIS 10.1 and the R programming language.
References
- Jurczyk P, Lu JJ, Xiong L, Cragan JD, Correa A. FRIL: A Tool for Comparative Record Linkage. AMIA Annual Symposium Proceedings 2008;2008:440–44.
- Liu F. Australian Postcodes with Geocoding 2013 [internet]. Sydney: Orite, 2009 [updated January 2009]. Available at http://blog.orite.com.au/tag/australian-postcode [Accessed 4 August 2015].
- McLafferty S, Freeman VL, Barrett RE, Luo L, Shockley A. Spatial error in geocoding physician location data from the AMA Physician Masterfile: implications for spatial accessibility analysis. Spatial and spatio-temporal epidemiology 2012;3(1):31–38.
- Australian Beauru of Statistics. Australian Statistical Geography Standard (ASGS): Volume 1 – Main Structure and Greater Capital City Statistical Areas. Canberra: ABS, 2011. Available at www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/7CAFD05E79EB6F81CA257801000C64CD?opendocument [Accessed 4 August 2015].