Vitamin D has become the subject of debate in a wide range of health conditions and two systematic reviews of available evidence were published recently.1,2 The association between vitamin D levels and sunlight exposure, and the cofactors of latitude and skin colour are well documented.3
Vitamin D synthesis is primarily related to exposure of the skin to ultraviolet B (UVB) light. Darker skin colour reduces the penetrance of UVB and up to six times as much UVB exposure is required to synthesise an equivalent amount of vitamin D in a dark-skinned individual, compared with an individual with fair skin.4
There is extensive literature on the increased risk of vitamin D deficiency in darker skinned ethnic groups in temperate latitudes.5 Western Australian guidelines for testing vitamin D levels in pregnancy identify Aboriginal women as one of the groups at risk.6 However, there is limited literature specifically on Aboriginal women and their vitamin D status. Bendall et al3 found significantly lower vitamin D levels in Aboriginal and Torres Strait Islander women, compared with non-Indigenous women; however none of the women were found to be deficient (based on a definition of deficiency as levels of <50 nmol/L). This study was conducted in tropical northern latitudes of Australia. Perampalam et al7 measured levels of vitamin D in two populations of women in temperate areas of Australia and found ethnicity to be one of several predictive factors for deficiency; however, there were only 10 Aboriginal and Torres Strait Islander women included in the sample of 201 women.
Methods
A cohort study was conducted to determine whether there was an association between Aboriginality and vitamin D levels during pregnancy in temperate latitudes of Australia. The study site was the Western Australian city of Kalgoorlie (latitude 30.7489°S, longitude 121.4658°E), population 35,000, of which 8.8% are Aboriginal.8 The study period ran from March 2010 to March 2012. To minimise selection bias, 100 consecutive obstetric patients were enrolled at presentation at each of two antenatal clinics. Aboriginal patients attended the local ACCHS. Non-Aboriginal patients attended a private general practice in the same town. Data on Aboriginality were clearly documented for all patients at both clinics. Multivitamin supplementation was advised for the non-Aboriginal group at the first antenatal visit but was not commenced until serum vitamin D levels were collected. Supplementation was not routinely prescribed in the Aboriginal group of women; however, women found to be deficient in vitamin D in pregnancy were treated with 5000 IU daily of cholecalciferol as per guidelines6 and the local paediatricians were made aware of maternal vitamin D deficiency at the time of delivery, so that provision could be made for neonatal supplementation.
Laboratory testing of serum from both groups of women was done at a single pathology laboratory, using the DiaSorin LIAISON assay to measure 25 hydroxyvitamin D (25(OH)D). Although this commonly used radioimmunoassay has been found to show variability between laboratories, compared with the gold standard of liquid chromatography, particularly at levels of 25(OH)D <50 nmol/L,9 this imprecision does not affect the conclusions from this study.
During the data collection phase, community education was undertaken in the ACCHS and a community education day held to engage the community more fully in the project. A Plain English pamphlet was produced, advocating adequate sun exposure as the first lifestyle option and to explain the reason for supplementation.
Power calculations showed that an n of 100 women per group would have 80% power to detect a difference of at least 0.5 of the standard deviation (SD) difference between the means of the vitamin D levels in the two groups. Analyses were conducted using SAS (Version 9.3, SAS Institute Inc., Cary, NC, USA). Differences between the two groups were analysed using Student’s t-test or Wilcoxon rank sum test for numerical variables, and Fisher’s exact test for categorical variables. Analysis of variance was used to identify factors affecting serum vitamin D levels.
Ethical approval for this study was granted by the Western Australian Aboriginal Health Information and Ethics Committee, and the Human Research Ethics Office, University of Western Australia (HREC approval number RA/4/1/4736).
Results
Sampling occurred between March 2010 and March 2012 for the Aboriginal group and between July 2010 and September 2011 for the non-Aboriginal group. Despite the variation in duration of sampling between the two groups, there was consistency in the numbers of women tested in each season.
The vitamin D levels for the Aboriginal women (mean 46.7, SD 21.7 nmol/L) were significantly lower than those from the non-Aboriginal group (mean 65.4, SD 18.4 nmol/L, P <0.0001). Vitamin D levels were categorised as sufficient, insufficient or deficient according to accepted definitions10,11 (Figure 1) and showed 18% of Aboriginal patients had vitamin D deficiency at measurement, compared with 2% of non-Aboriginal patients. Less than half (44%) of the Aboriginal group had levels in the sufficiency range, compared with 80% of the non-Aboriginal group of women.
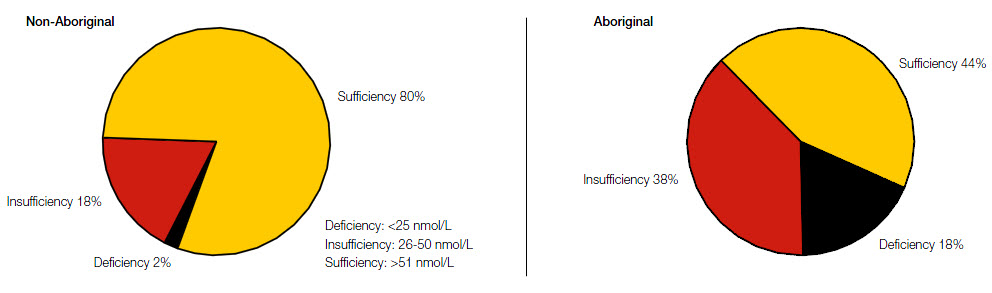 |
| Figure 1. Comparison of vitamin D levels in Aboriginal and non-Aboriginal pregnant women |
Along with vitamin D levels, data were collected on patient age, gestation at testing, BMI, baby birth weight, gestation at birth and complications of pregnancy and birth (Table 1).
Table 1. Demographics by antenatal group
|
|
|
Aboriginal
|
Non-Aboriginal
|
P value
|
|---|
|
Factor
|
Mean
|
SD
|
Mean
|
SD
|
|
|
Age
|
24.8
|
6.2
|
29.5
|
5.1
|
0.0001
|
|
BMI
|
29.3
|
6.2
|
28.5
|
5.7
|
0.382
|
|
Gestation at testing*†
|
20
|
9, 31
|
10
|
10, 11
|
0.0001
|
|
|
|
N
|
%
|
N
|
%
|
|
|
|
Tri 1
|
37
|
38.1%
|
90
|
90.0%
|
0.0001
|
|
|
Tri 2
|
24
|
24.7%
|
6
|
6.0%
|
|
|
|
Tri 3
|
36
|
37.1%
|
4
|
4.0%
|
|
|
Season at testing
|
|
|
|
|
0.956
|
|
|
Spring
|
23
|
23.0%
|
25
|
25.0%
|
|
|
|
Summer
|
22
|
22.0%
|
24
|
24.0%
|
|
|
|
Autumn
|
25
|
25.0%
|
23
|
23.0%
|
|
|
|
Winter
|
30
|
30.0%
|
28
|
28.0%
|
|
|
Vitamin D level at testing
|
46.7
|
21.7
|
65.35
|
18.4
|
0.0001
|
|
*Median and interquartile range (weeks); † Trimester unknown for 3 Aboriginal women; Total N for each group = 100
|
The Aboriginal women were significantly younger (P <0.0001) and presented later in pregnancy (P <0.0001). There were no statistically significant differences between the groups for BMI or season of testing. Univariate analysis of the effect on serum vitamin D levels of the other factors showed that increasing BMI was associated with lower levels of vitamin D (10 nmol/L per 10 BMI units; P = 0.0004) but there was no association between age and vitamin D levels (P = 0.94). The season in which the sample was taken had a significant effect (P = 0.0011) such that vitamin D levels during winter were significantly lower than during summer and autumn. Summer measurements were an average of 15.0 nmol/L higher and autumn measurements an average 13.4 nmol/L higher for both groups than measurements taken in winter (Figure 2).
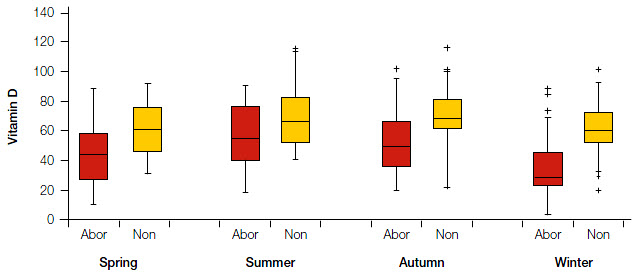 |
Figure 2. Vitamin D level (nmol/L) by season of measurement for Aboriginal and non-aboriginal pregnant women
The bottom and top edges of the boxes are located at the sample 25th and 75th percentiles, the centre horizontal line is drawn at the 50th percentile median, with the whiskers extending to 1.5x the interquartile range, and outliers represented by the plus signs |
The results showed an association between gestational age at testing and vitamin D levels (P = 0.0001), which, after controlling for season and BMI, were higher levels in trimester 1. Ninety percent of patients from the non-Aboriginal group had their levels measured in the first trimester, compared with 38% of the Aboriginal group, who had a much more variable time of testing. This related to the more variable stage of pregnancy that the Aboriginal women presented for their first antenatal appointment.
Despite the variations between the two groups there was still an independent effect of ‘grouping’ (P = 0.0078), the Aboriginal group having serum levels 11.5 nmol/L lower than those from the non-Aboriginal group after controlling for the confounding variables of BMI, season and gestational age at testing.
Discussion
 |
| Figure 3. Painting by local Aboriginal artist commissioned as part of the community engagement in the vitamin D project |
This is the first study to compare vitamin D levels in pregnant Aboriginal women with non-Aboriginal women living in the same community at temperate latitude. Aboriginal women in this study were significantly more likely to have lower levels of vitamin D than non-Aboriginal women and more likely to be deficient. Of note, one in five Aboriginal women were deficient and more than half had vitamin D levels in the insufficient range.
Our results show the relationship between season of testing and vitamin D level, deficiency being more prevalent in winter than in summer.7 This has led to recommendations for healthy levels of sun exposure in winter of at least 20 minutes (at midday) at latitudes similar to the that of the location in our study.12 This recommendation is for individuals with fairer skin type and there is evidence that people with darker skin require 3–6 times more exposure with as much bare skin exposed as is practicable.11
Latitude has an impact on vitamin D levels and there is evidence that vitamin D deficiency in pregnancy is not as prevalent in tropical regions of Australia.3 A study from temperate Australia (two towns at a similar latitude as Kalgoorlie) with predominantly non-Aboriginal women, confirmed suboptimal vitamin D rates of 26–35% in an antenatal population.7 This evidence makes it clear that clinicians need to be familiar with patterns of deficiency that affect their own locale. This study supports the argument that latitude and ethnicity (skin colour) influence vitamin D levels.
There was a considerable variation in the timing of testing between our two groups. The non-Aboriginal group was tested consistently in the first trimester, whereas there was a more marked variation of gestation of testing in the Aboriginal group. Plasma levels of 25(OH)D are not known to alter over the course of a pregnancy and remain comparable to the non-pregnant state.11 During pregnancy there is known to be an increase in conversion to the active form of vitamin D (1,25 dihydroxy vitamin D).13 The increased conversion is due to enzyme activity in placental tissue, maternal kidney and fetal decidua, and results in an increase in maternal calcium absorption, presumably to cater for fetal bone mineralisation.13
Infants born to mothers who are vitamin D deficient will inevitably be deficient themselves.11 Breast milk is a poor source of vitamin D, and supplementation for infants of deficient mothers is recommended until the age of 12 months.11
Two recent systematic reviews have analysed the evidence surrounding the poor health outcomes associated with suboptimal vitamin D levels. After extensive review of a large number of trials, no conclusive results could be found and further well designed trials were recommended.1,2 Vitamin D supplementation was found to be linked to an increase in maternal vitamin D at term and subsequent infant birth weight, and to a decrease in dental caries in children. This finding supports the current recommendation for supplementation in pregnancy.6 Currently, vitamin D supplements are not PBS-listed for any indication apart from end-stage renal failure.
This study was limited by a small sample size and the fact that other predictors of vitamin D level, such as skin pigmentation and time spent outdoors, were not measured. Standardisation of blood collection to the same trimester for the two groups would have added strength to the outcomes. The results do, however, reinforce how an understanding of the patterns of deficiency in relation to local geography and ethnicity can direct the decision to test for vitamin D deficiency in pregnancy. This study has helped identify a group of pregnant women for whom efforts could be focused.
Implications for general practice
- Targeted testing for vitamin D deficiency in pregnancy is worth considering for Aboriginal women in temperate parts of Australia.
- Lifestyle messages about adequate and safe sun exposure in dark-skinned women needs to be a routine part of antenatal education.
- Individuals with darker skin types and high BMI are at risk of vitamin D deficiency.
- PBS-listing of vitamin D in a formulation specified in locally used antenatal guidelines will make supplementation more accessible to Aboriginal women who are found to be deficient.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
The authors would like to acknowledge the editorial contributions of David Atkinson and Andrew Kirke, and the Rural Clinical School of Western Australia for provision of an Early Research Career Grant. We also acknowledge the Bega Garnbirringu Health Service staff and community.