Headache is a common presenting problem in the primary care setting and this is especially true for the paediatric population. There are variations in incidence but studies have shown a prevalence of >10% for migraines and chronic daily headache in adolescent populations.1–3 Interestingly, prior to puberty, boys are affected more commonly, whereas girls are affected more commonly thereafter.4 Headaches have a significant global health burden for children and adolescents in terms of school absenteeism, school performance and psychological conditions.5 This is irrespective of the underlying cause of the initial headache6 and may be related to the nature of chronic illness.7
Common causes of headaches in children include febrile illnesses, with or without ear, nose and throat involvement, migraines and tension headaches. Rarer and more serious causes such as meningitis, space-occupying lesions or subarachnoid haemorrhage must always be considered. Given the only symptom of this last group may be a headache, there can be a great deal of parental anxiety and it is imperative that a primary care physician assesses a child thoroughly to rule these out.
Assessment
Table 1. Red flags
|
- Acute and severe headache
- Progressive chronic headaches
- Focal neurology
- Age <3 years
- Headache/vomiting on waking
- Consistent location of recurrent headaches
- Presence of ventriculo-peritoneal shunt
- Hypertension
|
When faced with a patient presenting with headache, it is important to remember that a comprehensive history is the most likely way to elucidate the underlying cause. This is especially true for children, where clinical signs of serious pathology, such as a space-occupying lesion, will only be apparent at a late stage. However, careful clinical examination is also imperative, as almost all children with a serious underlying pathology will have at least one objective clinical sign on examination.8
A systematic approach to the history is essential and should include red flag symptoms (Table 1). It is useful to provide a chart with representations of headache patterns9 (Figure 1) to give the child a visual cue to explain their symptoms. It may be helpful to show the child and family this chart and ask them to identify the pattern themselves.
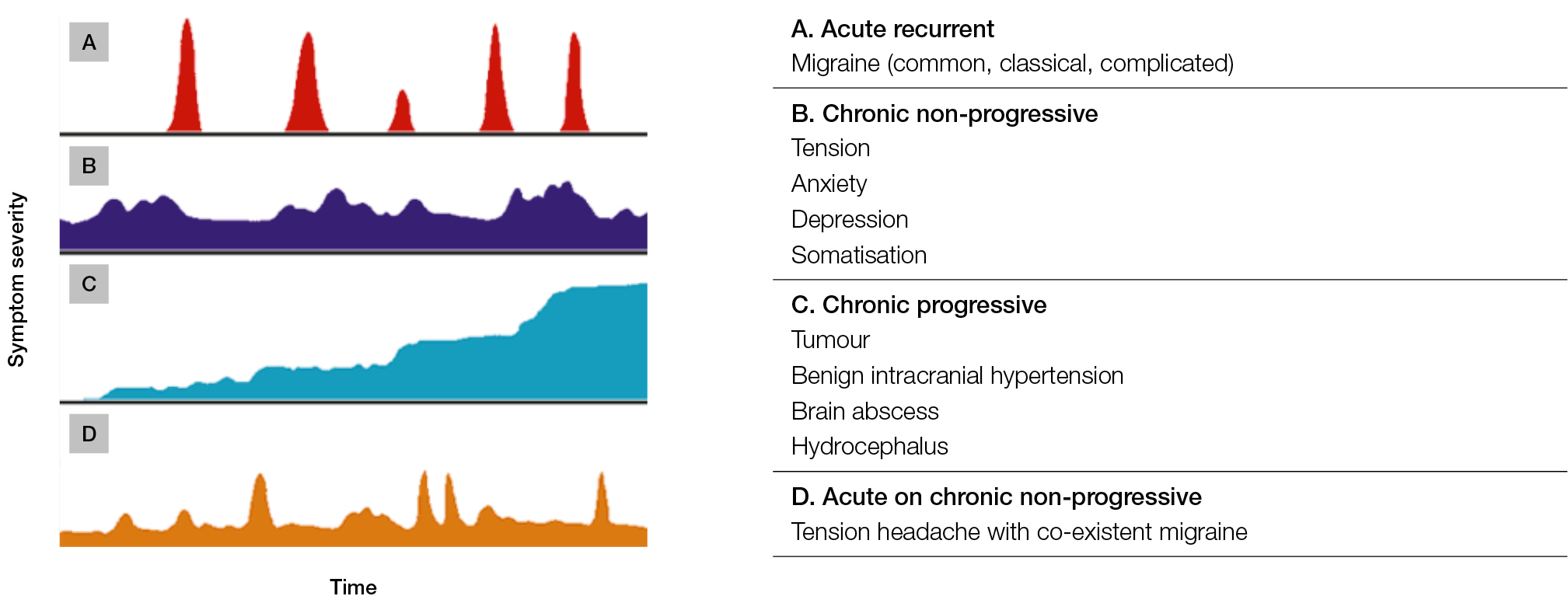 |
Figure 1. Headache patterns
Adapted, with permission, from resources at The Royal Children’s Hospital, Melbourne, Australia. |
Psychosocial factors must also be considered. An adolescent HEADSS (Home/Education/Activities/Drugs/Sexuality/Suicide and depression) screen may be helpful. A collateral history from parents or carers is essential and in certain cases it may be necessary to interview the child or adolescent separately, although clearly a sensitive approach is required in this situation. Evidence suggests that people who suffer abuse as children are more likely to have recurrent tension headaches or migraines as adults,10 and it is reasonable to extrapolate from this that the headaches and migraines may commence while they are still adolescents.
Headaches related to specific conditions may have typical associated symptoms, although there can be considerable overlap with these. The most important initial distinction to make is whether the headache is recurrent as this will immediately give the physician a very different group of potential diagnoses to consider. The typical features of recurrent and other types of headaches are described in Table 2.
Table 2. Typical features of headaches
|
|
Recurrent
|
|
Tension-type headaches (approximately 50% incidence25)
- Non-pulsatile band
- Often at end of day
- Few associated symptoms
|
|
Migraines (approximately 25%)
- Pulsing pain
- Nausea
- Photophobia
- Phonophonia
- Often unilateral
|
|
Other
|
- Fever without associated meningism
- Upper respiratory tract infection
- Pneumonia
- Septicaemia
- Local sinusitis
- Focal facial tenderness
- Otitis media
- History of recent head injury
- Meningitis (NB: classic signs less common in paediatric population)
- Irritability
- Decreased consciousness
- Petechiae/purpura
- Photophobia/neck stiffness
- Subarachnoid haemorrhage
- Sudden onset (‘thunderclap’)
- Vomiting
- Often occipital
- Rebound/overuse headache
|
Recurrent headaches
On the condition that there are no red flag symptoms and that the headache history is one of multiple episodes without increasing severity or frequency, it is reasonable to class them as recurrent. The next useful distinction involves attempting to separate tension-type headaches from migraines as this will help with ongoing management plans. There is often overlap within this group and migraine sufferers report tension-type headaches and vice versa. However, the characteristics described in Table 2 may help to distinguish one from the other.
Childhood migraines
The prevalence of migraines within paediatric populations varies significantly. Interestingly, a study has shown a higher prevalence (roughly 25%) of migraines in US medical students, possibly giving an insight into the underlying stressors that can contribute to their development.11 In general, it is thought that 5–10% of children and adolescents self-report or have a physician diagnosis of recurrent migraines.12,13 They are more common in females. It is important to remember that up to 15% of children who present with recurrent abdominal pain may be suffering from abdominal migraines;14 these will require specialist referral. The possibility of an association between obesity and headaches, including migraine, has been raised, but the evidence is limited.15
Managing migraines is difficult in both primary and emergency settings. It is made more complex in the paediatric population because of the difficulty with diagnosis, parental concern and limited treatment options approved for paediatric use, as well as poor adherence to medical therapies. Within the primary care setting, the goals of treatment should include confident diagnosis, elucidation of causative or underlying factors and an attempt to address them, consideration of abortive treatments and discussion around ongoing management, including possible referrals to specialists or other healthcare professionals. This must obviously be set against the time and resource constraints experienced by general practitioners (GPs).
Before pharmacological intervention is commenced, it is important to address the environmental factors that can either trigger a migraine or make it more likely to persist. Many people develop an awareness of particular triggers but this is highly idiosyncratic and there has been no evidence proving any particular trigger exists across large cohorts; this includes the supposed bête-noire, chocolate.16 What is clear is that either fasting or skipping meals can precipitate the onset of a migraine and that an exclusion diet can be a useful tool to attempt to establish patient-specific triggers;17 this is best performed through the GP. Other simple measures, such as ensuring regular bedtimes and adequate hydration, may also help to decrease the frequency of episodes.
Simple analgesia
The mainstay of pharmacological treatment has previously been limited to simple analgesia, usually paracetamol alone or combined with a non-steroidal anti-inflammatory drug (NSAID) such as ibuprofen. This was because of a lack of large trials involving other medications, especially in children and adolescents. Although simple analgesia may be effective in tension-type headaches and migraines, many people receive limited or no relief. Moreover, regular use is associated with the development of analgesia-related headaches, which can be more problematic. However, simple analgesia is appropriate for a first presentation; the substitution of aspirin (not used in the paediatric group because of the risk of Reye syndrome) may be more effective with ibuprofen in the adolescent population.
Triptans
Over recent years there has been an increasing use of medications from the triptan group, most commonly sumatriptan. These agents work through 5-HT(1B/1D) receptors in three ways:
- promoting vasoconstriction of painfully dilated cerebral blood vessels
- inhibiting the release of vasoactive neuropeptides by trigeminal nerves
- inhibiting nociceptive neurotransmission.18
The efficacy of triptans has been established in several large studies and recently there has been more evidence for their safety and effectiveness in the adolescent population.19 In the paediatric population (<12 years of age), triptans have been shown to be reasonably safe but not overly effective in the termination of recurrent migraines. Different formulations are available, including nasal sprays and sublingual wafers, and it is likely that these will become a mainstay of migraine termination treatment, especially in the adolescent population.20–23
Treatment of migraine is most effective if instigated at the onset of symptoms. It is important, therefore, to educate children, to increase their awareness of triggers and how to recognise the onset of an episode, then encourage early pharmacological intervention along with adjustments to their environment. Schools or colleges should also be made aware of the condition to permit effective treatment as well as minimisation of stigmatisation and class absence.
Prophylaxis
There is limited evidence for any specific therapies and most of those used in paediatric groups are done so off-label and on the background of anecdotal case studies. Propranolol is often used in children and appears to be associated with few adverse effects.24 Given the significant potential side effects of other proposed prophylactic agents and the lack of evidence regarding their efficacy, these are best started by specialists.
Conclusion
Childhood migraines create a significant health burden and are probably under-diagnosed and treated. A systematic approach to their presentation can help to alleviate both parental and physician anxiety and allow for an accurate diagnosis. Treatment is multifactorial but pharmacological intervention certainly should play a role along with adjustment of environmental factors and addressing possible underlying psychosocial factors. Referral is an important tool for the family doctor and possible routes would be GPs with specialist interests, neurologists or adolescent clinics. In extremis, the ED is a reasonable option to allow aggressive abortive treatments but ongoing management should be coordinated through the family doctor. The future for this field will involve:
- increased evidence for specific pharmacological interventions within the paediatric population
- development of better and cheaper formulations
- development of an effective paediatric-specific migraine questionnaire to allow accurate monitoring of individuals
- an analysis of the link between obesity and migraines.15
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.