Published literature provides information about the prevalence of obstetric and gynaecological problems in the population. Many of these conditions are more prevalent in specific age groups. For example, approximately 20% of women of reproductive age have menorrhagia.1 Chronic pelvic pain affects 15% of women aged 18–50 years,2 and pelvic floor disorders (urinary incontinence, faecal incontinence and pelvic organ prolapse) affect 24% of women aged ≥20 years and 50% of those aged ≥80 years.3 Population prevalence estimates do not provide insight into the impact of these problems on workload in general practice.
The Bettering the Evaluation and Care of Health (BEACH) program has already shown that general practitioners (GPs) in Australia refer female patients to gynaecologists and obstetricians at a rate of 0.8 per 100 GP–female patient encounters, most commonly for menstrual problems, ‘other’ genital disease (eg ovarian cyst, endometriosis), abnormal test results, uterovaginal prolapse and infertility/sub-fertility.4 This reflects the type of problems requiring specialist care, but we know little about the overall workload associated with management of obstetric and gynaecological (O&G) problems in general practice. The aims of this study were to describe the frequency of management of O&G problems at encounters with female patients in general practice, and to investigate differences by patient age.
Method
This is a secondary analysis of data from the BEACH program, a national study of general practice activity in Australia. BEACH methods are described in detail elsewhere.5 In summary, every year approximately 1000 randomly sampled GPs record details of 100 consecutive encounters with consenting patients on structured paper recording forms. Ethics approval for the BEACH program was obtained from the Human Research Ethics Committee of the University of Sydney (HREC 2012/130).
For this study, analyses of all encounters with female patients for the data period April 2004 to March 2014 were undertaken. O&G problems were defined as all problems classified in the International Classification of Primary Care, version 2 (ICPC-2)6 as ‘female genital’ (X chapter) and ‘pregnancy and family planning’ (W chapter); and selected urogenital problems classified in the urological chapter (including urinary incontinence, urethritis, and prolapse).
Results
O&G problems were managed at a rate of 19.2 per 100 encounters with female patients, accounting for 12.0% of all problems managed for female patients. The majority of O&G problems managed were for women aged 25–44 years (48.2%), followed by women aged 45–64 years (25.4%), 0–24 years (19.0%) and ≥65 years (7.4%).
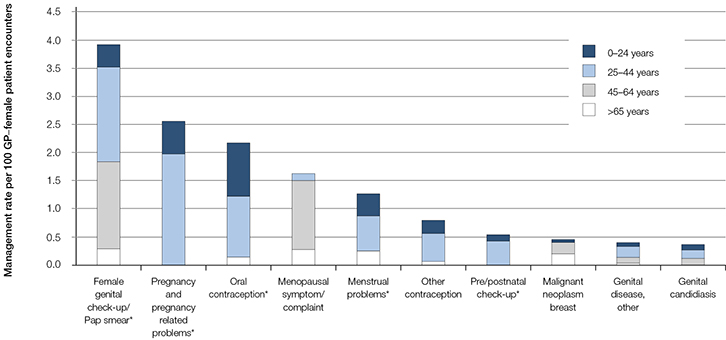 |
Figure 1. Ten most common gynaecological/obstetric problems managed at encounters with female patients in Australian general practice (2004–14)
*Includes multiple ICPC-2 or ICPC-2 PLUS codes (see Appendix 1, available online) |
Figure 1 shows the 10 most commonly managed O&G problems. The different colours illustrate the proportion of each problem managed in each age group. Overall, these 10 problems accounted for 73.3% of all O&G problems managed. Certain age groups predominated in each problem. For example, genital check-up/Pap smear was managed at a rate of 3.9 per 100 GP–female patient encounters, but the majority of these problems were managed for women aged 25–44 years (43.3%) and 45–64 years (39.5%). By contrast, malignant breast neoplasm was managed at a rate of 0.4 per 100 GP–female patient encounters; 46.3% of these problems were managed among women aged 45–64 years, and 45.1% among those aged ≥65 years (Figure 1).
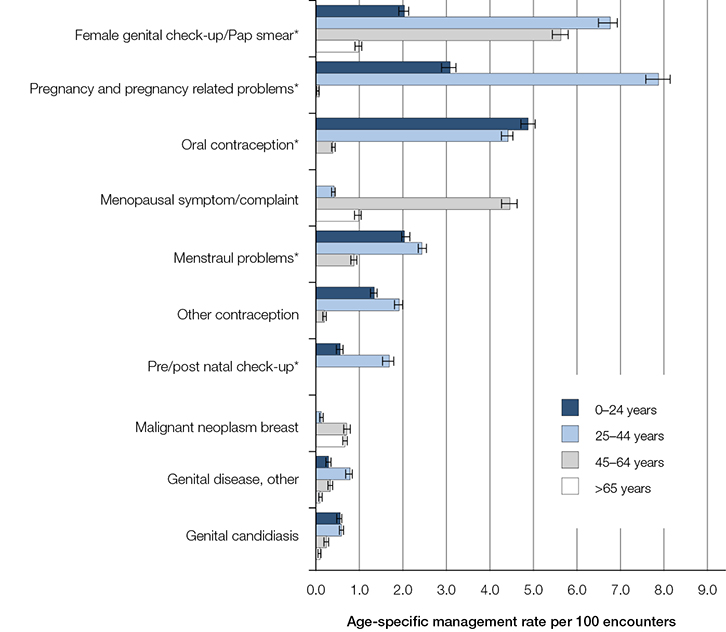 |
Figure 2. Age-specific management of the most common gynaecological/obstetric problems among females at Australian general practice encounters (2004–14) (95% confidence intervals)
*Includes multiple ICPC-2 or ICPC-2 PLUS codes (see Appendix 1, available online) |
As there were marked differences in the age-related distribution for each problem, we investigated the age-specific management rate (Figure 2). The proportion of all problems accounted for by O&G problems in each age group, and the most common O&G problems managed by GPs are described below.
0–24 years: O&G problems were managed at a rate of 19.2 per 100 encounters with female patients in this age group, and accounted for 14.9% of all problems managed with these patients. The most commonly managed problems were oral contraception (4.9 per 100 encounters in this patient group), pregnancy (3.1), menstrual problems (2.1), and check-ups related to the genital system/Pap smears (2.0 per 100 encounters) (Figure 2).
25–44 years: An average of 36.8 O&G problems were managed per 100 encounters with women aged 25–44 years, and these problems accounted for one-quarter of all problems managed for women in this age group. Pregnancy and pregnancy-related conditions (7.9 per 100 encounters) were the most commonly managed, followed by genital check-up/Pap smear (6.7), oral contraception (4.4) and menstrual problems (2.5).
45–64 years: O&G problems were managed at a rate of 17.7 per 100 encounters with women in this age group and these problems accounted for 10.5% of all problems at these encounters. The most common were genital check-up/Pap smear (5.6 per 100 encounters), menopausal symptoms (4.5), menstrual problems (0.9) and malignant breast neoplasm (0.7).
≥65 years: At encounters with older women, O&G problems were managed at a rate of 5.0 per 100 encounters and accounted for 2.7% of all problems. The most commonly managed were genital check-up/Pap smear (1.0 per 100 encounters), menopausal symptoms (1.0), malignant breast neoplasm (0.7; Figure 2) and urinary incontinence (0.4; results not shown).
Comparison of the age-specific management rates reveals some interesting differences. For example, oral contraception was most frequently managed among females in the youngest age group, whereas other forms of contraception were managed most frequently among women aged 25–44 years. Pregnancy and pre/postnatal check-ups were more than twice as likely to be managed at encounters with women aged 25–44 years, compared with any other age group. By contrast, management rates of breast cancer were similar among women aged 45–64 years and those aged ≥65 years.
Discussion
One in eight problems managed at encounters with female patients were related to O&G problems. A significant proportion of problems involved preventive care, particularly genital check-ups/Pap smears. If the recommendations for changes to the cervical cancer screening program are adopted (5-yearly human papillomavirus testing instead of 2-yearly Pap smears),7 it is likely that these types of check-ups will decrease.
This study shows that the management rates and types of O&G problems differed considerably by patient age. Younger women were more likely to have contraception, pregnancy, and menstrual problems managed, whereas for older women, menopausal symptoms, genitourinary problems and breast cancer were more commonly managed. This article provides a quantitative description of GPs’ management of O&G problems and may provide context for other articles in this edition of Australian Family Physician.
Authors
Clare Bayram BAppSc (HIM) (Hons), PhD, Research Fellow and Project Manager, BEACH program, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW. clare.bayram@sydney.edu.au
Allan Pollack MBBS (Hons), MBiomedE, FRACS (Orth), Research Officer, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Carmen Wong BHS, MHI, Research Officer, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Helena Britt BA, PhD, Director, Family Medicine Research Centre, Sydney School of Public Health, Sydney Medical School, University of Sydney, NSW
Competing interests: None.
Provenance and peer review: Commissioned, externally peer reviewed.
Acknowledgements
We wish to thank the general practitioners who participated for their generosity. During the data collection period of this study, the BEACH program was funded by the Australian Government Department of Health, AstraZeneca Pty Ltd (Australia), Novartis Pharmaceuticals Australia Pty Ltd, bioCSL (Australia) Pty Ltd, Merck Sharp & Dohme (Australia) Pty Ltd, Pfizer Australia Pty Ltd, Sanofi-Aventis Australia Pty Ltd, GlaxoSmithKline Australia Pty Ltd, National Prescribing Service Ltd; Janssen-Cilag Pty Ltd; Abbott Australasia Pty Ltd; Roche Products Pty Ltd; and the Australian Government Department of Veterans’ Affairs.
BEACH data coded using the ICPC-2 PLUS terminology are usually reported at the level of the ICPC-2 classification (for example, genital candidiasis female is ICPC-2 code X72). However, there are some exceptions where data are grouped either above the ICPC-2 level or across the ICPC-2 level. These grouped morbidities are marked with an asterisk in Figures 1 and 2, and are defined below.
Appendix 1. Code groups from ICPC-2
|
|
Group
|
ICPC-2 rubric
|
ICPC-2/ICPC-2 PLUS label
|
|---|
|
Female genital check-up/Pap smear
|
X30
|
Medical examination/health evaluation, complete, genital female
|
|
|
X31
|
Medical examination/health evaluation, partial, genital female
|
|
|
X37
|
Histological/exfoliative cytology, genital F
|
|
Menstrual problems
|
X02
|
Menstrual pain
|
|
|
X03
|
Intermenstrual pain
|
|
|
X05
|
Menstruation absent/scanty
|
|
|
X06
|
Menstruation excessive
|
|
|
X07
|
Menstruation irregular/frequent
|
|
|
X08
|
Intermenstrual bleeding
|
|
|
X09
|
Premenstrual symptom/complaint
|
|
|
X10
|
Postponement of menstruation
|
|
Oral contraception
|
W10
|
Contraception post-coital
|
|
|
W11
|
Contraception, oral
|
|
|
W50
|
Medication prescription/request/renewal/injection reproductive system
|
|
Pregnancy and pregnancy related problems
|
W01
|
Question of pregnancy
|
|
|
W78
|
Pregnancy
|
|
|
W79
|
Unwanted pregnancy
|
|
|
W05
|
Pregnancy nausea/vomiting
|
|
|
W84
|
Pregnancy high risk
|
|
|
W29
|
Pregnancy symptom/complaint
|
|
|
W03
|
Antepartum bleeding
|
|
|
W92
|
Complicated labour/delivery, livebirth
|
|
|
W90
|
Uncomplicated labour/delivery, livebirth
|
|
|
W81
|
Toxaemia of pregnancy
|
|
|
W99
|
Disorders of pregnancy/delivery
|
|
|
W70
|
Puerperal infection/sepsis
|
|
|
W93
|
Complicated labour/delivery, stillbirth
|
|
|
W96
|
Complications of puerperium
|
|
|
W91
|
Uncomplicated labour/delivery, stillbirth
|
|
|
W71
|
Other infection complicating pregnancy/puerperium
|
|
|
W75
|
Injury complicating pregnancy
|
|
Prenatal/postnatal check-up
|
W30
|
Medical examination/health evaluation, complete, pregnancy
|
|
|
W31
|
Medical examination/health evaluation, partial, pregnancy
|