Asthma is the most common chronic disease among children in Australia, placing significant burden on the individual, their family and the wider community. The prevalence of asthma in Australian children is among the highest in the world, affecting up to 20.8% of children at some point in their childhood.1
While there are various medications and practice guidelines available to assist healthcare professionals with optimising the management of childhood asthma, data indicate that management of childhood asthma in Australia remains suboptimal.2 Evidence suggests that long-acting beta-2 agonists (LABAs) are over-prescribed in the initial management of childhood asthma, both nationally and internationally.1,3
Adequate control of childhood asthma relies on the use of evidence-based medicines with established efficacy, as outlined by management guidelines.4–7 Implementation of, and adherence to, guideline-based childhood asthma management has been associated with improved clinical outcomes and reduced risk of exacerbations in children with asthma, as well as improved quality of life for the children and their families.8
The aim of this study was to investigate adherence to management guidelines for childhood asthma among Australian doctors. This study will provide baseline data to inform future interventions to improve the management of childhood asthma.
Methods
A total sample of 1000 doctors (500 general practitioners [GPs] and 500 paediatric specialists) were approached Australia-wide. These doctors were randomly selected from the Medical Directory of Australia,9 which lists details of qualifications and specialty of virtually all registered doctors in Australia. The random sample was obtained by AMPCo Direct (Australasian Medical Publishing Company Ltd).
The selected doctors were sent a personalised letter of explanation and the four-page survey. A follow-up reminder letter was sent to all of the doctors three weeks after the initial letter was sent.
The survey dealt with the demographics of the doctors, and assessed their familiarity with four available practice guidelines: those of the National Asthma Council (NAC),4 Global Initiative for Asthma (GINA),5 Therapeutic Guidelines,6 and the Thoracic Society of Australia and New Zealand (TSANZ).7 Three clinical vignettes were included to determine reported practice in recently diagnosed asthma requiring maintenance therapy, poorly controlled asthma requiring step-up therapy, and stable asthma requiring step-down therapy (Table 1). The stepped approach to adjusting asthma medication in children, as recommended by practice guidelines, recognises that all children with persistent asthma should be using an as-needed reliever initially, and treatment should be stepped up or down according to recent asthma control and risk. From an initial as-needed reliever, the next step would be the addition of a preventer (low-dose, inhaled corticosteroids [ICS], leukotriene receptor antagonist [LTRA], or cromone), then a stepped-up, regular preventer (higher dose ICS, or low-dose ICS plus LTRA, or ICS/LABA combination). When asthma is stable and well controlled for longer than three months, stepping down should be considered.4–7
Table 1. Overview of clinical vignettes and guideline recommendations*
|
|
Summarised vignette
|
Common guideline recommendations
|
|---|
|
Recently diagnosed asthma, preventive therapy indicated
- Salbutamol used 3–4 times per week
- Sleep disrupted once a week
- Current medications: salbutamol when required
|
Correct options
- Add an ICS
- Add an inhaled cromone
- Add an LTRA
Incorrect options
- Add an LABA
- Add an ICS/LABA combination
|
|
Poorly controlled asthma, ‘step-up’ therapy indicated
- Short of breath most days
- Sleep disrupted 2–3 times per week
- Missed three school days in two months
- FEV1 = 70% predicted
- Current medications: fluticasone 125 μg twice daily and salbutamol when required
|
Correct options
- Change to an ICS/LABA combination
- Increase ICS dose
- Add an LTRA
Incorrect options
- Add an inhaled cromone
- Change to maintenance and reliever therapy
|
|
Stable asthma, ‘step-down’ therapy indicated
- Never needs to use salbutamol
- FEV1 = normal
- No symptoms for past eight months
- Current medications: fluticasone 125 μg, salmeterol 25 μg twice daily, and salbutamol when required
|
Correct options
- Cease LABA while continuing ICS
- Decrease ICS dose while continuing LABA
Incorrect options
- Cease ICS while continuing LABA
- Cease ICS and LABA
- Do nothing to the treatment regime
|
|
*Fictional patients aged 5–9 years, all assumed to be adherent with therapy and have correct inhaler technique. FEV1, forced expired volume in one second; ICS, inhaled corticosteroid; LABA, long-acting beta-2 agonist; LTRA, leukotriene receptor antagonist.
|
All survey variables were entered into a statistical software package, SPSS version 21 (IBM, Armonk, New York). Comparisons between GPs and paediatric specialists were tested using the chi-square test for dichotomous variables (with Yates’ Correction for Continuity) and the Mann-Whitney U test for continuous variables; P values of <0.05 were deemed statistically significant.
To assess the impact of a number of factors on overall adherence to guidelines, respondents were classified as adherent if they followed all three recommendations for initial asthma management, step-up therapy and step-down therapy. Direct logistic regression was performed to assess the impact of a number of factors (profession, gender, years registered, location of practice, hours each week seeing patients, and new cases of childhood asthma each month) on the likelihood of overall adherence to guidelines for management of childhood asthma.
This study was approved by the Tasmanian Social Sciences Human Research Ethics Committee (reference number: H0013070).
Results
Table 2. Characteristics of the responding doctors*
|
|
|
All doctors
|
GPs
|
Specialists
|
P value
|
|---|
|
Number
|
200
|
83 (41.5%)
|
117 (58.5%)
|
|
|
Gender
|
|
|
|
|
|
Male, n (%)
|
125 (62.5)
|
45 (54.2)
|
80 (68.4)
|
0.06
|
|
Female, n (%)
|
75 (37.5)
|
38 (45.8)
|
37 (31.6)
|
|
|
Years registered
|
|
|
|
|
|
Median
|
32
|
32
|
30
|
0.6
|
|
Range
|
4–53
|
6–49
|
4–53
|
|
|
Location of practice
|
|
|
|
|
|
Urban, n (%)
|
184 (92.9)
|
75 (90.4)
|
109 (94.8)
|
0.36
|
|
Rural, n (%)
|
14 (7.1)
|
8 (9.6)
|
6 (5.2)
|
|
|
Hours per week seeing patients
|
|
Median
|
35
|
35
|
32
|
0.14
|
|
Range
|
3–88
|
10–88
|
3–80
|
|
|
New cases of childhood asthma per month
|
|
Median
|
3
|
2
|
5
|
<0.0001
|
|
Range
|
0–25
|
0–25
|
0–20
|
|
|
*Values represent number (%) of respondents to each question; percentages may not add up to the total n for the group due to blank responses to individual questions.
|
Of the 1000 surveys distributed, 261 (26.1%) were returned. Sixty-one (25.7%) doctors reported that they did not regularly review children with asthma. Excluding those responses, the 200 relevant responses yielded a 20% response rate. The response rate of paediatric specialists was significantly higher than that of GPs (23.4% versus 16.6%, P = 0.007). Eighty-three (41.5%) respondents were GPs and 117 (58.5%) were paediatric specialists (Figure 1). Compared with GPs, paediatric specialists saw significantly more new cases of childhood asthma each month (Table 2).
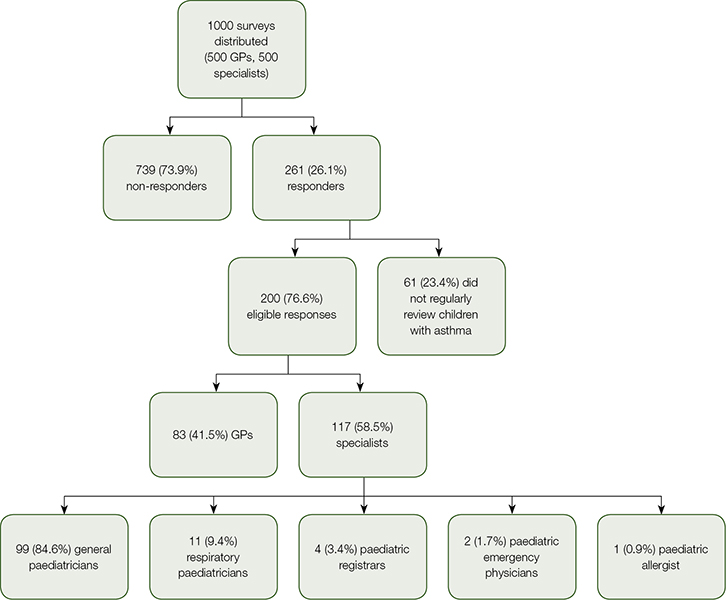 |
| Figure 1. Overview of respondents |
Respondents were most familiar with the NAC guidelines (91.5% had at least some awareness of the guidelines; Figure 2). In total, 109 (54.5%) respondents were very familiar with at least one of the guidelines: 50 GPs (60.2%) and 59 paediatric specialists (50.4%).
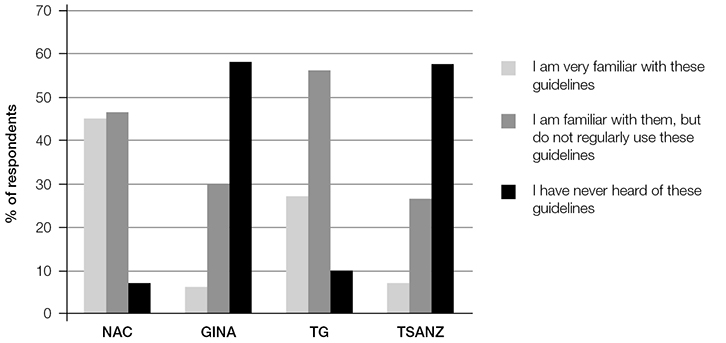 |
Figure 2. Level of familiarity with guidelines as reported by all respondents
GINA, Global Initiative for Asthma; NAC, National Asthma Coucil; TG, Therapeutic Guidelines; TSANZ: Thoracic Society of Australia and New Zealand |
Table 3 displays the responses to clinical vignettes, compared to childhood asthma management guideline recommendations. Of the respondents, 171 (86.8%) followed guideline recommendations when prescribing initial maintenance therapy for childhood asthma, with 121 (61.4%) prescribing ICS, 46 (23.4%) prescribing LTRAs and four (2.0%) prescribing inhaled cromones. Twenty-six (13.2%) respondents did not adhere to guideline recommendations, with 21 (10.7%) prescribing an ICS/LABA combination and five (2.5%) prescribing LABA as initial therapy.
Table 3. Adherence to asthma management guidelines*
|
|
Clinical situation
|
All respondents
(n = 200)
n (%)
|
GPs (n = 83)
n (%)
|
Specialists (n = 117)
n (%)
|
P value
|
|---|
|
Initial maintenance therapy
|
|
Adherent to guidelines
|
171 (86.8%)
|
63 (75.9%)
|
108 (94.7%)
|
<0.0001
|
|
Non-adherent
|
26 (13.2%)
|
20 (24.1%)
|
6 (5.3%)
|
|
Step-up therapy
|
|
Adherent to guidelines
|
173 (89.2%)
|
66 (80.5%)
|
107 (95.5%)
|
<0.01
|
|
Non-adherent
|
21 (10.8%)
|
16 (19.5%)
|
5 (4.5%)
|
|
Step-down therapy
|
|
Adherent to guidelines
|
132 (68.0%)
|
50 (61.7%)
|
82 (72.6%)
|
0.15
|
|
Non-adherent
|
62 (32.0%)
|
31 (38.3%)
|
31 (27.4%)
|
|
*Values represent number (percent) of respondents to each question. Percentages may not add up to the total n for the group due to blank responses to individual questions.
|
When step-up therapy was indicated, 173 (89.2%) respondents followed guideline recommendations, with 94 (48.5%) changing to an ICS/LABA combination, 45 (23.2%) increasing ICS dose, 28 (14.4%) adding an LTRA, and six (3.1%) treating the symptoms as an exacerbation with oral corticosteroids. Twenty-one (10.8%) respondents did not follow any specific guideline recommendations, changing to budesonide/eformoterol maintenance and reliever therapy.
When step-down therapy was indicated, 132 (68.0%) respondents followed guideline recommendations, with 90 (46.4%) ceasing LABA while continuing ICS, and 42 (21.6%) decreasing ICS while continuing LABA. Sixty-two respondents (32.0%) did not follow any specific guideline recommendations, with 29 (14.9%) choosing to do nothing to the treatment regime, 27 (13.9%) ceasing both ICS and LABA, five (2.6%) ceasing ICS while continuing LABA, and one (0.5%) switching to budesonide/eformoterol maintenance and reliever therapy.
When factors were compared to overall guidelines adherence, paediatric specialists were significantly more likely to adhere to management guidelines than GPs (67.0% of paediatric specialists versus 39.8% of GPs, P <0.0001). Respondents who spent fewer hours each week seeing patients, and those who saw more new cases of childhood asthma each month, were also significantly more likely to adhere to management guidelines (median 30 hours each week for adherent respondents versus 40 hours each week for non-adherent respondents, P = 0.01; median four new cases for adherent respondents versus two new cases for non-adherent respondents, P = 0.01). The logistic regression model assessing the impact of a number of factors on overall adherence to guidelines was statistically significant (ⅹ2 = 19.9, df = 6, P = 0.003), indicating that the model was able to distinguish between respondents who were classified as adhering and those classified as not adhering to management guidelines. The model as a whole explained between 10.0% (Cox and Snell R squared) and 13.3% (Nagelkerk R squared) of the variance in guidelines adherence, and correctly classified 65.3% of cases. Only one independent variable made a unique statistically significant contribution (profession), where it recorded an odds ratio of 3.1 (95% CI, 1.6–6.25; p = 0.001). This indicated that paediatric specialists were more than three times more likely to be adherent to management guidelines than GPs, controlling for all other factors in the model.
Discussion
Our data shows that self-reported practice among these doctors was consistent with guideline recommendations in some areas but discrepant in others. The adherence rate to guidelines was approximately 85% for initial asthma management and step-up therapy, and 66% for step-down therapy. The reasons for this may be attributed to some doctors disagreeing with guideline recommendations and, instead, following clinical judgement based on their own experience and that of their peers. Indeed, previous habits and peers’ beliefs have been found to shape how doctors act on clinical information.10 While international studies have described barriers such as lack of awareness, confidence, knowledge and understanding, and lack of agreement and outcome expectancy,11–13 further research investigating the barriers and facilitators of adherence to guidelines among Australian doctors is required.
Paediatric specialists were significantly more likely to follow asthma management guidelines for the initial treatment of childhood asthma than GPs. Approximately 95% of paediatric specialists and 75% of GPs prescribed a preventer medication as initial maintenance therapy, in accordance with guideline recommendations. As the survey options indicative of non-adherence in this vignette were LABA monotherapy or ICS/LABA combination therapy, around 5% of paediatric specialists and 25% of GPs reported inappropriately over-prescribing LABAs to children for initial therapy. This finding is consistent with other Australian data indicating an over-use of LABAs in childhood asthma.1,14 Our data confirm that combination therapy is indeed a preferred treatment option among a minority of doctors.
When step-up therapy was indicated in a patient on medium-dose ICS, approximately 85% of respondents followed guideline recommendations. There is an unresolved issue in asthma management regarding the stage at which LABAs should be introduced for a patient whose symptoms are not optimally controlled with regular ICS therapy,15 which may have contributed to some of the reported non-adherence.
When step-down treatment was indicated in a patient taking medium-dose ICS in combination with LABA, two-thirds of respondents followed guideline recommendations, while one-third of respondents reported non-adherent treatment preferences. The preferences deviating from guideline recommendations were fairly evenly split between choosing to do nothing to the treatment regime, and the other extreme of ceasing both ICS and LABA at once.
Asthma management guidelines stress the importance of reducing medications once good asthma control is achieved and maintained,4–7 an option that should be regularly considered and will be frequently successful.16 However, there is still considerable uncertainty regarding how and when treatment should be stepped down.17 Unclear recommendations and reports of patients deteriorating when stepping down18 may lead to hesitancy to step-down asthma therapy after achieving symptom control.
Respondents more likely to adhere to management guidelines in the treatment of childhood asthma included paediatric specialists and those who spent fewer hours per week seeing patients and those who saw more new cases of childhood asthma per month. This was not surprising considering paediatric specialists and GPs who see more new cases of childhood asthma per month would undoubtedly be more experienced in childhood asthma management. Additionally, doctors who spent less time seeing patients may have more time for continuing education activities; time limitations have previously been described as a barrier to adherence to guidelines.11
The fact that specialisation (paediatric specialists versus GPs) was a significant independent predictor for adherence to guidelines – paediatric specialists were three times more likely to adhere to management guidelines – indicates that any educational programs aimed at improving the management of childhood asthma should focus on GPs.
The data collected were from a 20% response rate and may not provide a true representation of Australian prescribing for childhood asthma medication. However, the response rate was similar to other surveys of doctors’ treatment practices,19–21 and was considered acceptable for this form of research, especially given the relatively long questionnaire.22 Nevertheless, it should be borne in mind that the results may underestimate the problem of non-adherence to guidelines in Australia, as it is reasonable to assume that doctors may have been less likely to respond if they were unsure of, or did not adhere to, current guidelines. Additionally, vignettes may not provide a true illustration of real-life prescribing as they are not real-life scenarios. Notwithstanding these limitations, the results of this study provide valuable information regarding Australian prescribing practices in childhood asthma and are consistent with previous findings.
In conclusion, although the majority of respondents adhered to guideline recommendations, overall familiarity with the guidelines was suboptimal, and there is scope for improvement in adherence to these guidelines for prescribing in childhood asthma. LABAs are still being over-prescribed in childhood asthma, and there seem to be some uncertainties surrounding step-up and step-down recommendations. Further studies are needed to investigate the apparent gap between guidelines and current practice before strategies can be placed to improve the management of childhood asthma.
Implications for general practice
- There is scope for improvement in the adherence to guidelines for prescribing medication in childhood asthma.
- Responses to clinical vignettes suggest LABAs are over-prescribed to children for initial asthma management.
- There are uncertainties and inconsistencies among doctors regarding step-up and step-down asthma treatments.
- Innovations to improve prescribing practices in childhood asthma may be warranted.
Acknowledgements
We gratefully acknowledge the doctors who participated in our study.
Authors
Bonnie J Bereznicki BPharm (Hons), PhD, Lecturer, University of Tasmania, Hobart, TAS. Bonnie.Bereznicki@utas.edu.au
Sean Beggs MBBS, MPH, RACP, Paediatrician, Royal Hobart Hospital; Senior Lecturer in Paediatrics and Child Health, University of Tasmania, Hobart, TAS
Caitlin Duff, BPharma (Hons), Pharmacy Graduate, University of Tasmania, Hobart, TAS
Luke Bereznicki, BPharm (Hons), PhD, MPS, Associate Head (Pharmacy) and Deputy Head of School (Medicine), University of Tasmania, Hobart, TAS
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.