The aim of this study was to determine the accuracy of medication histories documented on GP referral letters for patients referred to emergency departments, and describe the nature of discrepancies detected in these referral letters. This study will provide baseline data to inform future interventions to improve the continuum of care.
Methods
This multicentre prospective observational study was undertaken in the emergency departments of eight Australian public hospitals across five states between January 2008 and May 2009. The study was approved by each hospital’s Human Research and Ethics Committees (HREC). The patient recruitment period varied between hospitals, depending on the rate of patient presentation, the number of hours a pharmacist was available in the emergency department and when site-specific HREC approval was granted.
Consecutive patients seen by a pharmacist during routine care in the emergency department were recruited if they were taking one or more regular medications, were referred to the emergency department by their GP or a locum doctor and presented with a GP or locum letter. Patients were excluded if they presented from a residential care facility or the emergency department pharmacist was unable to verify a BPMH with at least one other information source, in addition to the GP letter.
A structured data collection tool compiled information documented during pharmacists’ standard care. In obtaining the BPMH, pharmacists evaluated at least one, but preferably two or more, sources of information for each medication, in addition to the GP letter. Sources included patient/relative interview, medications and lists brought to the emergency department, telephone contact with the GP, community pharmacist and/or nursing services. The pharmacist, in collaboration with emergency department medical and nursing staff, subjectively determined if there were any communication difficulties with the patient.
The BPMH had to be of a standard that ensured the pharmacist would be confident that patient safety would not be compromised if it was used to make clinical decisions. The BPMH was that regimen the patient was actually taking, (not necessarily as prescribed), as that was the regimen on which future prescribing decisions should be based. Where a GP correctly noted both what was intended and actually taken, no discrepancy was recorded.
The main outcome measure was the proportion of patients with one or more medication discrepancies, pertaining to regular medications, between the GP referral letter and BPMH. Secondary outcomes were the nature and significance of discrepancies and the prevalence of discrepancies by whether the letter was handwritten or electronically generated.
Discrepancies were classified as omission of a medication that the patient was taking, medications listed that the patient was not taking (commission), discrepancy pertaining to dose, frequency, form, route of administration or medication class or no dose/frequency provided. Medication class discrepancies were where a medication was listed, but another within the same class was taken. Significance of discrepancies was assessed using a published tool3 that considered severity and likelihood of a potential adverse event on the basis of the discrepancy being prescribed on an admission medication chart and administered for at least 1 week. If medications were omitted, significance was assessed on the basis of clinical decisions being made without information about the particular medicine. Two senior emergency department pharmacist investigators, not involved in the care of the individual patient, independently assessed the significance, and differences in assessment were resolved through consensus.
Of 62 consecutive patients presenting with a GP letter during a pilot study, 73% of letters contained one or more discrepancies. To have 95% certainty that the proposed study error rate would lie within 5% of this pilot proportion, at least 318 patients needed to be enrolled. Therefore, at least 50 consecutive patients were recruited from each of the eight sites. Chi-square test (with Yates correction) and Mann Whitney U tests were used to compare proportions and non-parametric continuous data, respectively. Statistical Package for the Social Sciences (SPSS, version 22) was used for all calculations. The level of significance was 0.05.
Results
The characteristics of the 414 patients recruited and their GP referral letters are outlined in Table 1. The median age was 76 years and patients took a median of six regular and one as-needed medications. One in seven patients had communication difficulties, meaning that a reliable history could not be taken from the patient and, therefore, other sources of information were used. One-third of patients were admitted to a short stay unit and almost half to an inpatient ward. Two or more sources of information, in addition to the GP letter, were used to obtain the BPMH for 299/414 (72.2%) of patients. For the 115 patients where one source was used in addition to the GP letter, the patient was interviewed in 99 cases, their carer in 10 cases, the community pharmacy dispensing records in five cases and a recent hospital discharge list in one case.
Table 1. Characteristics of the patients and the GP referral letters presenting to the emergency department
|
Characteristic (n = 414)
|
|---|
|
Male/female
|
204/210
|
|
Age, years, median (IQR )
|
76 (63–82)
|
|
Number of regular medications taken, median (IQR)
|
6 (4–-9)
|
|
Number of as-needed medications, median (IQR)
|
1 (0–2)
|
|
Number of patients with communication problems (for medical or language reasons)
|
58 (14.0%)
|
Number of patients admitted to hospital from ED
|
144 (34.8%)
190 (45.9%)
|
Medical practitioner who referred patient to ED
- General practitioner
- Locum doctor
|
392 (94.7%)
22 (5.3%)
|
How referral letter was written
- Typed/electronically generated
- Handwritten
|
350 (84.5%)
64 (15.5%)
|
|
ED, emergency department; IQR, interquartile range
|
|---|
Overall, 361 (87.2%) patients had one or more discrepancies between the BPMH and the GP referral letter pertaining to their regular medications; this percentage ranged from 80.0–95.2% across each of the eight hospitals (Chi square, P = 0.255). For as-needed medications, 182 (44.0%) of patients had one or more discrepancies between the BPMH and the GP referral letter. The distributions of discrepancies per patient, pertaining to the regular and as needed medications are outlined in Figure 1. The median number of discrepancies per patient was 3 (interquartile range [IQR]: 1–5) and 0 (IQR: 0–1) for the regular and as-needed (PRN) medications, respectively. One or more discrepancies of omission pertaining to regular medications occurred in 76.6% of handwritten letters, compared with 45.7% of typed letters (difference in percentages 30.9%, P <0.001). In 12.5% of hand-written letters, one or more regular medications were listed in the GP letter that the patient was not taking, whereas this discrepancy occurred in 48.9% of typed letters (difference in percentages 36.4%, P <0.001)
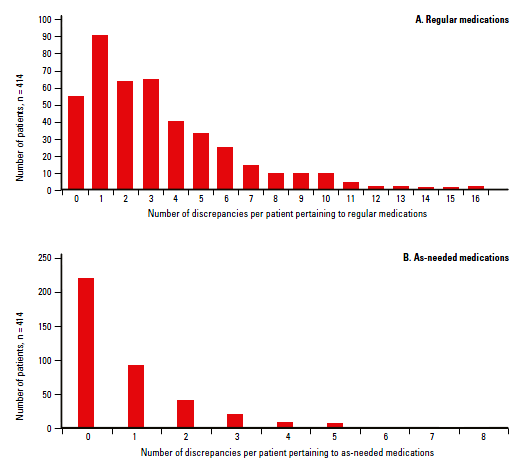 |
| Figure 1. Distribution of discrepancies between the best possible medication history and the general practitioner letter pertaining to medications |
The types of discrepancies and their significance are described in Table 2. The most prevalent discrepancies involved omission of a medication that the patient was taking or inclusion of a medication that the patient was not taking. Overall, 62.1% of patients had one or more discrepancies pertaining to their regular medications deemed to be of moderate or high significance. The majority of discrepancies pertaining to PRN medications were of low significance.
Table 2. Description of the types of medication discrepancies between the GP referral letter and the best possible medication history
|
Discrepancy category
|
Occurrence (%)
|
|---|
|
Regular medications
(n = 1383)
|
PRN medications
(n = 351)
|
|
Medication omitted from GP letter that patient was taking (omission)
|
483 (34.9)
|
137 (39.0)
|
|
Medication listed on GP letter that patient was not taking (co-mission)
|
450 (32.5)
|
149 (42.5)
|
|
No dose/frequency listed
|
203 (14.7)
|
11 (3.1)
|
|
Dose/strength discrepancy
|
158 (11.4)
|
10 (2.8)
|
|
Dose frequency discrepancy
|
69 (5.0)
|
42 (12.0)
|
|
Alternative medication from within a class listed*
|
11 (0.8)
|
0 (0)
|
|
Dose form discrepancy
|
7 (0.5)
|
2 (0.6)
|
|
Route of administration discrepancy
|
2 (0.1)
|
0 (0)
|
|
Discrepancy significance
|
|---|
|
Low
|
804 (58.1)
|
331 (94.3)
|
|
Moderate
|
511 (36.9)
|
20 (5.7)
|
|
High
|
68 (4.9)
|
0 (0)
|
|
*eg patient taking perindopril but ramipril listed
|
|---|
A selection of high significance discrepancies are summarised in Table 3. Warfarin was omitted from the letter in four cases (one referred to the emergency department with haematemesis and another with deep vein thrombosis), warfarin was listed but the dose was incorrect in four cases and in two cases, a potentially interacting medication was omitted (tramadol, NSAID) or listed but no longer taken (aspirin). In six cases, warfarin was listed but with no dose information.
Table 3. Selection of cases associated with highly significant discrepancies with the GP letter
- GP letter listed atorvastatin as a drug sensitivity (myopathy), but atorvastatin was still listed as a current medication, although the patient had ceased this as instructed.
- GP letter listed aspirin, but it had been ceased after a recent GI bleed.
- Two methotrexate doses incorrectly listed on the GP letter, both were prescribed on the hospital admission medication chart.
- 70 units/day of fast acting insulin omitted from GP letter.
- Patient presented with acute-on-chronic renal failure. Diclofenac omitted from GP letter.
- Slow release morphine 100 mg orally twice daily omitted from GP letter in a patient referred to ED with acute pain.
- Patient referred to ED with congestive heart failure taking 1.5 x 12.5 mg carvedilol twice daily. GP listed 3.125 mg twice daily as the current dose.
- Patient referred to ED with congestive heart failure. Warfarin, carvedilol, frusemide, ramipril, spironolactone and thyroxine omitted from the GP letter.
- Twice daily glibenclamide listed on the GP letter; 70 year old patient no longer taking.
- Patient referred to ED with chest pain and shortness of breath. Incorrect warfarin dose listed, fentanyl patch listed but no longer used and frusemide omitted but current dose was 120 mg daily.
|
Quantifying the causes of discrepancies was beyond the scope of this study but various reasons for discrepancies were identified. Patients often had not recently reviewed their entire regimen with their GP and at the time of referral to the emergency department there were higher clinical priorities. Patients often took some medications prescribed by a specialist, such as a cardiologist or psychiatrist, which were not listed in the GP records. Often, a medication was replaced by another, but the ceased medication remained on the list of medications included on the referral letter. Warfarin was often dosed and sometimes prescribed by an external pathology service. Where the GP was not prescribing the warfarin, it may not have appeared on the medication list and where the GP was not involved in the dosing, the current dose was not provided. Occasionally, the patient was not taking a medication as the GP had intended, but this was rarely an explanation for discrepancies.
Discussion
This study found that for the majority of patients presenting to the emergency department, the referral letter from a GP had discrepancies between the medication listed in the letter and the BPMH. This study has implications for many individuals involved in maintaining the continuum of care as patients move between care settings. GPs should routinely review medication regimens with their patients and medications no longer being taken should be archived. Software providers should enable this to occur easily and prescribers should be prompted at appropriate times. The date of the last review should be included in extracts of the medication regimen in referral letters. If documentation of the medication regimen cannot be incorporated within the time constraints of a GP consultation, a periodic home medicines review with a pharmacist should be considered. Where medications are prescribed by specialists and during hospital admission, these prescribers have a duty of care to inform the patient’s GP of changes made to the patient’s regimen in a timely, legible format, and this information should be incorporated into the GP’s records.
Hospital doctors, nurses and pharmacists need to be aware of the pitfalls of using GP referral letters in isolation to determine the BPMH at the time of hospital presentation. Electronically generated letters are legible, but not necessarily accurate. Referral letters, as for any other information source, must be verified with at least one other source before making medication-related decisions. The letter must not replace a patient/family interview, as patients may not divulge non-adherence or use of complementary medicine to their GP.9,10 Patients with language barriers are particularly vulnerable to medication misadventure; therefore, correct information from the GP is vital for this group.11 Our study found that discrepancies of omission occurred more often in handwritten letters, whereas discrepancies involving inclusion of a medication that the patient was not taking occurred more often in typed letters. This is consistent with anecdotal observations that ceased medications frequently remain on GP lists generated from software programs, whereas handwritten lists frequently include the medication name without the dose/frequency or only list the medications relevant to the referral.
Accurately determining a medication history on admission is a challenge that all hospitals face. This national study found no significant differences in discrepancy rates at any one site; the primary endpoint of having one or more discrepancies pertaining to the regular medications occurred in at least 80% of patients across all hospitals. An audit conducted in 2011 in a regional hospital found that 75% of patients had one or more discrepancies in their GP medication list.12 In 2012, St Vincent’s Hospital, Sydney participated in the Personally Controlled Electronic Health Record (PCEHR) Wave 2 Site Project, where GP referrals were electronically submitted to the hospital from participating GPs.13 The emergency department pharmacist used the same methodology described in this study to compare electronically submitted GP referrals (eGP) and paper-based GP referrals, and found electronically submitted GP referrals had one or more discrepancies in 65% of medication lists, compared with 79% in paper-based referrals (P <0.001). Hence, accuracy of the medication lists remains a clinical handover and continuum of care issue and electronic tools require maintenance to maximise accuracy.
This study has some limitations. Only patients seen by the emergency department pharmacists were included, which may not be representative of all patients presenting with a GP referral letter. Patients were recruited only at times when an emergency department pharmacist was available. Future work must evaluate whether discrepancies result in prescribing errors and patient harm.
In summary, GP referral letters should not be relied on in isolation to accurately reflect the medication regimen taken by patients before presentation to the emergency department. Hospital staff should use the GP letter as an adjunct to other sources for determining a patient’s medication history. Interventions are needed to improve awareness of this issue and improve accuracy of medication histories forwarded to emergency departments from GPs.
Implications for general practice
GPs should routinely review their patient’s medication regimens and archive ceased medications. Software providers should readily enable this to occur and prompt prescribers at appropriate times.
GPs should include the date of the last comprehensive medication review in extracts of the medication regimen that appear on their referral letters.
Where reviewing the medication regimen cannot be incorporated within a GP consultation, a periodic home medicines review with a pharmacist should be considered.
Where medications are prescribed by specialists and during hospital admission, these prescribers have a duty of care to inform the GP of changes made to their patient’s regimen, in a timely, legible format. GPs should actively acquire this information if it is not forthcoming.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.