 |
| Figure 1. Rash on the patient’s forehead |
|
 |
| Figure 2. Rash on the patient’s left lower leg |
|
Question 1
What differential diagnoses would you consider for the rashes shown?
Question 2
What further history would you take?
Question 3
What areas would you examine?
Question 4
What initial investigations would you perform in this case?
Answer 1
The differential diagnoses that should be considered are listed in Tables 1, 2.
Table 1. Differential diagnoses of the plaque rash shown in Figure 11
|
|
Condition
|
Features
|
|---|
|
Urticaria
|
Presents as itchy wheals, which disappear within 24–48 hours
|
|
Plaque psoriasis
|
Presents with erythematous, scaly plaques on extensors of the body. May involve scalp, nails, palms and soles
|
|
Tinea corporis
|
A common fungal infection of the skin involving a red, pruritic, scaly rash with an active edge and central clearing
|
|
Sarcoidosis
|
A multisystem granulomatous disorder. Skin lesions can be papules, nodules, plaques or scar infiltration, or non-specific (eg erythema nodosum)
|
|
Leprosy
|
Skin lesions can be hypopigmented or erythematous macules, papules, plaques, nodules, with associated peripheral nerve thickening and numbness
|
|
Syphilis
|
A sexually transmissible infection. Secondary syphilis may present as multiple, asymptomatic macules, papules or plaques
|
|
Neurofibromatosis
|
A genetic disorder presenting with multiple café-au-lait macules, neurofibromas (soft tumours) and freckles in the axillae/groins in its cutaneous manifestation.
|
Table 2. Differential diagnoses of the linear nodular eruption shown in Figure 21
|
|
Type of infection
|
Example
|
|---|
|
Bacterial
|
Leishmaniasis, fishtank granuloma (Mycobacteria marinarum), cutaneous tuberculosis, leprosy (rare)
|
|
Fungal
|
Sporotrichosis, cryptococcosis, histoplasmosis, blastomycosis
|
|
Viral
|
Human papillomavirus, cowpox
|
Answer 2
A systems review must be taken. The symptoms of sarcoidosis vary depending on the organ affected and there are accompanying constitutional symptoms. Sensory loss, initially temperature discrimination, is the first sign of leprosy in 90% of patients and may precede skin lesions by years.1 Take a sexual history to assess risk of syphilis, a travel history for leprosy, leishmaniasis and tuberculosis, occupational history for sporotrichosis and Mycobacterium marinum, and a family history for psoriasis, leprosy and neurofibromatosis. This patient migrated from Nepal 6 years earlier. There was no family history of skin disease. He worked in a restaurant and lived with his wife who was well.
Answer 3
It is important to examine the rest of the body. Psoriasis may affect the scalp and cause nail changes such as pitting. Syphilis often involves oral and genital mucosae with lymphadenopathy. Leprosy may cause anaesthetic patches and thickening of nerves (most commonly ulnar and lateral popliteal) with possible autonomic dysfunction (hair loss, anhidrosis) and motor loss.2 Sarcoidosis may manifest with chest crackles, pericardial rub or hepatomegaly.2 In this patient there was no lymphadenopathy or organomegaly, and mucosae were normal.
Answer 4
A punch biopsy specimen for histopathology is essential. Request polymerase chain reaction (PCR; available in some centres) of the biopsy if unusual fungal or mycobacterial infection is suspected.3 Skin scrapings should be performed for any scaly patches. Syphilis serology should be requested for a widespread asymptomatic rash. A chest X-ray is required if sarcoidosis or tuberculosis is suspected. Tuberculosis and leprosy may co-exist.
Case continued
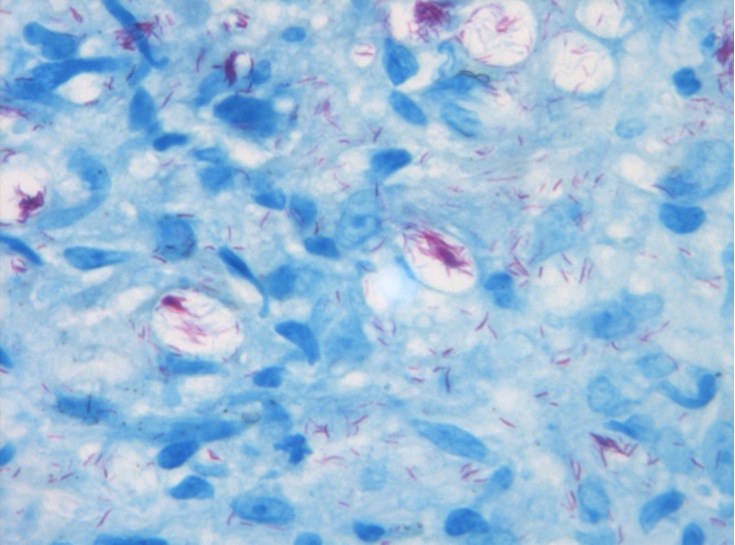 |
Figure 3. Fite modification of
Ziehl-Neelsen stain. High power view
showing multiple acid-fast bacilli |
The GP performed a punch biopsy of a papule on the left leg. The patient remarked that he did not feel the procedure and mentioned 12 months of numbness in the distribution of the left common peroneal nerve for which he had been referred to a neurologist but had not attended.
Fite modification of Ziehl-Neelsen stain of a section of the biopsy is shown in Figure 3. It shows large numbers of acid-fast bacilli and their appearance is typical of Mycobacterium leprae infection (histiocytoid pattern). Syphilis serology was non-reactive.
Question 5
What is the likely diagnosis?
Question 6
What is the management of this condition?
Answer 5
This is a case of leprosy.
Answer 6
Prompt referral to a dermatologist, infectious diseases specialist and neurologist is required.
Case continued
Leprosy is a notifiable disease in Australia so the GP notified the local public health unit. The patient was diagnosed with multibacillary leprosy and was started on the regimen recommended by the World Health Organization (WHO), which involves 12 months of monthly supervised rifampicin and clofazimine treatment, and daily self-administered clofazimine and dapsone treatment.4
His progress was complicated by leprosy reaction shortly after starting treatment, requiring high-dose oral prednisone, and a burn to his numb left pretibial area from prolonged contact with a laptop, requiring skin grafting. His wife did not show any signs of leprosy but needs annual screening for at least 5 years.
Discussion
Leprosy is a rare disease in Australia and the majority of cases occur in migrants from leprosy-endemic countries and, occasional, locally acquired cases in Aboriginal and Torres Strait Islander communities.5 Most of the people with leprosy (86% ) reside in six countries (India, Brazil, Indonesia, Myanmar, Madagascar and Nepal).2 Humans are the only known reservoir for M. leprae4 but leprosy has been identified as a zoonosis in armadillos and certain species of monkeys.6 It is thought to be transmitted by long-term close skin contact and respiratory aerosols.4 Most of those infected mount an appropriate immune response and never develop signs of leprosy.1 Household contacts of a person with untreated multibacillary leprosy have up to 10% risk of disease; children are at greater risk.7
Cell-mediated immunity (CMI) determines the clinical presentation. Preserved CMI leads to localised disease (paucibacillary) with 1–5 skin lesions and single or few nerves being involved, whereas impaired CMI leads to disseminated disease (multibacillary) with six or more skin lesions, extensive loss of sensation and involvement of many nerves.8
Key points
- Leprosy should be considered in any patient with progressive skin lesions, especially if they have neurological deficits or have lived in an endemic area.
- Consider leprosy as a cause of unexplained numbness in a person from an endemic area.
Competing interests: None.
Provenance and peer review: Not commissioned, externally peer reviewed.
Acknowledgements
We thank Andrew Gal, the pathologist who provided the biopsy photograph and report.